Abstract
Organ transplantation is a surgery in which doctors replace a person’s sick or damaged organ with a healthy organ from another person. The new organ can come from a living person who wants to help, or from someone whose brain died and thus does not need their organs anymore. The main problem with organ transplants is rejection, which happens when the immune system treats the new organ like a foreign invader such as an infection and tries to remove it. To prevent rejection, patients who received an organ transplant need to take many pills for the rest of their lives. These pills, called immunosuppressants, weaken the immune system and prevent it from attacking the new organ. Unfortunately, immunosuppressants also make the patients more susceptible to infections or cancer. Scientists are looking for ways to “re-program” the immune system, to decrease the likelihood of rejection.
The Purpose of Organ Transplantation
Our organs (such as the heart, liver, and kidneys) work together to keep our bodies functioning and healthy. If a critical organ gets sick or damaged and fails to work properly, the person could die very quickly. The function of some organs can be briefly replaced by machines. For example, a dialysis machine can replace failing kidneys for months, or a heart-lung-machine can replace a failing heart and/or lung for a few days. To replace failing organs for many years, organ transplantation is needed. This is a surgery in which doctors replace the sick person’s failing organ with a healthy organ from another person. The person receiving the organ is called the recipient, the organ is called the graft, and the person giving the organ is called the donor. In some cases of kidney, lung, or liver transplantation, the graft comes from a living donor—usually a close relative (check out this Young Minds article). In most cases, the graft comes from a donor whose brain died and who thus no longer needs their organs. Organ transplantation is a complicated surgery but the delicate part comes afterwards: to keep the graft working, it must be hidden from the recipients’ immune system [1].
The Immune System—The Body’s Police Force
The immune system is the body’s very own “police force”. Its main purpose is to defend the body against infections. Therefore, the immune system is always alert and continuously “scans” the body for foreign substances already within it or trying to enter. If it recognizes foreign molecular structures on the surface of an intruder (called antigens), a reaction is triggered to eliminate the intruder. Normally, the immune system only reacts to foreign substances (e.g., insect toxins) and organisms (e.g., bacteria) and does not fight against its own body (ourself). To achieve this very important discrimination between foreign and self, the immune system has evolved as a complex community of different white blood cells (so called leucocytes; Figure 1). Each leukocyte has different purposes and functions, some of them, so-called T cells, certain cells of the immune system, must go to “school” in an organ called the thymus, to learn what is foreign and should be eliminated and what is part of its own body and should not be touched [2].
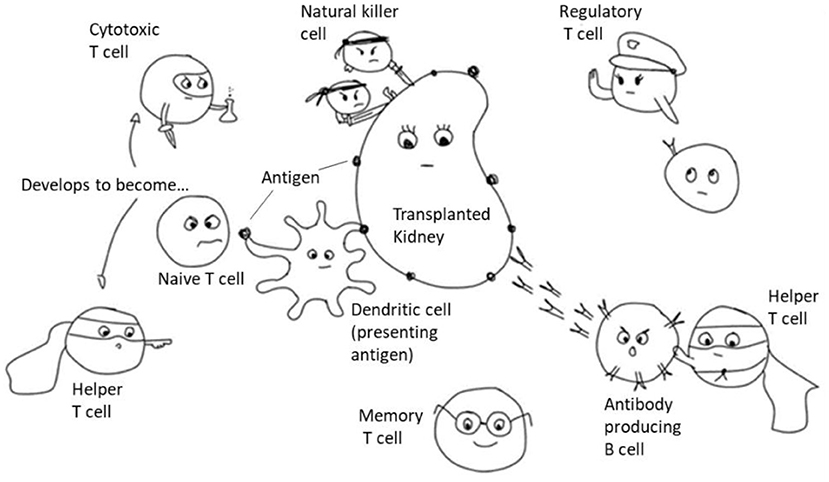
- Figure 1 - Immune cells involved in rejection of a kidney transplant.
- Dendritic cells pick up an antigen from the transplanted kidney and present it to naïve T cells which can become either cytotoxic or helper T cells. The helper T cells aid the antibody producing B cells to destroy the transplanted organ. The cytotoxic T cells and the Natural Killer cells directly attack the transplanted organ. The regulatory T cells tell them when to stop. Some T cells “keep records” of the attack, becoming memory T cells that are ready to respond if the same threat is faced again.
Our immune system has two lines of defense: the innate system is the body’s first line of defense and responds immediately to any intruder. For example natural killer (NK) cells attack everything that does not look familiar (or misses a specific “tag” saying it belongs to the body). Dendritic cells on the other hand “eat” foreign, damaged, or destroyed cells to clean up after an intruder and show parts of the intruder to the adaptive system. The adaptive system is the second line of defense. It constantly learns and develops memory to react even stronger and faster to the next encounter of the same intruder. The main cell types involved in rejection of a transplanted organ are T cells and B cells. Important T cell types are helper T cells that assist other cells in the immune response, cytotoxic T cells that directly kill infected cells, and regulatory T cells which prevent that the immune reaction gets out of control or starts attacking its own body. B cells are responsible for the production of antibodies.
Antigen Recognition—Let The Battle Begin
All cells of a person’s body have unique antigens on their surfaces, like a fingerprint. This antigen “fingerprint” is encoded in our genes and, except for identical twins, varies between people. An important part of this “fingerprint” are the HLA antigens. Among other roles, HLA antigens help the cells of the immune system to distinguish between our own cells and foreign cells. This means that HLA antigens are also the main targets of the immune system once a foreign organ (from a non-identical donor) is transplanted into the body [3].
Many immune cells are constantly patrolling the body. Upon a potential threat, cells called phagocytes (e.g., dendritic cells) will “eat” the intruding cells or debris, collect their antigens, and go to the nearest lymph node (bean-like structures located throughout the body) where they “show” the antigens to T cells. Lymph nodes are the “precinct” for the T cells, where they wait until somebody comes in to alarm them about an intruder. T cells carry a specific molecule on their surfaces that can recognize one particular antigen. But with millions of T cells patrolling the body, any potentially harmful antigen can be recognized by the immune system. When T cells recognize the evidence of an intruder, they multiply to form an army of clones, which are sent out to attack the intruder (cytotoxic T cells) or get the mission to help cytotoxic T cells become active and help B cells (helper T cells). Activated B cells produce antibodies that are released into the body and bind specific foreign antigens. Antibodies directly neutralize (e.g., viruses) or mark foreign structures for destruction (e.g., bacteria or cells of a transplanted organ; Figure 2).
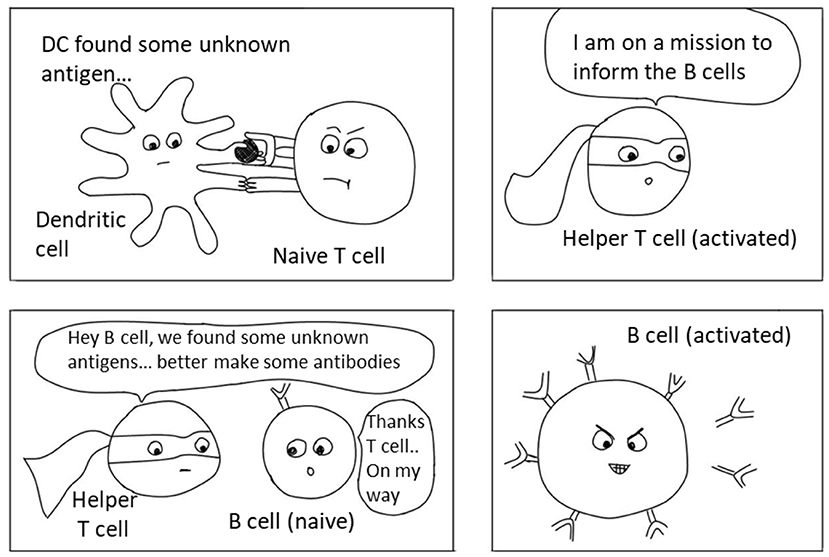
- Figure 2 - Antigen recognition in the lymph node and activation of immune cells.
- Dendritic cells (DCs) take up small parts of the foreign object (in this case the transplanted kidney) and bring these “antigens” to the lymph nodes to “show” them to the T cells. T cells who recognize the antigen interact with B cells. They are called “Helper T cells” because they help the B cells to become activated themselves and produce antibodies which are important in the immune response and fight against intruders (bacteria, viruses or in this case a transplanted organ).
T and B cells hold the “records” of all battles our immune system fought. After a battle is over, regulatory T cells will calm everyone down to prevent exaggerated inflammation and damage. Most T and B cell clones will die after the battle due to exhaustion. Some of these cells become memory cells which survive long-term and continue to circulate throughout the body or rest in lymph nodes.
This process explains how a transplanted organ is recognized as foreign, attacked, and destroyed by the immune system, leading to organ rejection.
Immunosuppressants—A Double-Edged Sword
To prevent the immune system from attacking the new organ, special medications are needed to “handcuff” and disarm the recipient’s immune system (Figure 3). These powerful drugs that weaken the immune system are called immunosuppressants. In the case of organ transplantation, immunosuppressants prevent the immune system from hurting the transplanted organ (for more details, check out this Young Minds article or this one).
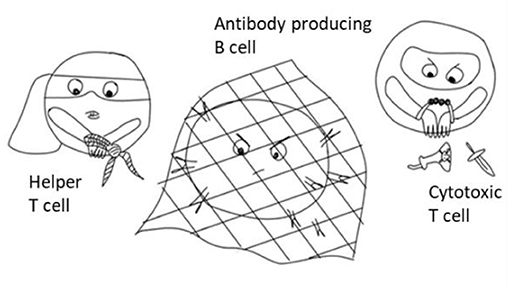
- Figure 3 - Immunosuppressive drugs prevent the immune cells, like T cells and B cells, from attacking the transplanted organ (or any other intruder).
- When a person takes immunosuppression, the immune cells are still alive in this person’s body, but are “handcuffed” or “trapped” and are not able to work/attack anymore. The main problem is that this immunosuppression is not specific and although the immune cells cannot fight the transplanted organ anymore, they also cannot fight other intruders (like bacteria or viruses). This makes our body defenseless and simple infections can become a life-threatening problem.
Because immunosuppressants are very powerful but also potentially toxic, patients taking them must be monitored carefully. It is really important for patients to take these medicines at the same time each day, to make sure that the level of medicine in the blood is always the same. Immunosuppressants are a double-edged sword. On one hand, they keep the life-saving transplanted organ safe and functioning. But on the other hand, they can also make the organ recipient very sick. Levels of immunosuppressants that are too high can cause unpleasant to life-threatening side effects (e.g., dizziness, infections, and cancer), whereas levels that are too low can lead to rejection. Finding the right dose of immunosuppressants is critical, and patients taking these medicines must be very careful to avoid people who have contagious diseases (e.g., the flu, measles) and should wear face masks in crowded public places. They must also be really careful to avoid sunburns, which could lead to skin cancer.
It is a major problem that immunosuppressants dampen all immune responses, not just those directed against the transplanted organ. Since these medicines are toxic to the body, it would better if recipients only needed to take them for a short time, not for the rest of their lives.
The Holy Grail—Tolerance
If an organ is transplanted between identical twins [like in the first successful transplantation [4]], immunosuppression is not needed due to the similar “fingerprints” between the donor and recipient. Some years ago, doctors encountered a very strange phenomenon: some kidney transplant recipients did not reject their organs even without immunosuppressants, similar to identical twins [5]. The special thing about these patients was that, years before the kidney transplant, all of them received immune cells through a bone marrow transplantation from the same person who donated the kidney (to treat another issue). The immune cells from the donor replaced the patient’s immune cells, like changing the staff of the “police station”. Consequently, newly produced immune cells, especially the stubborn T cells, are “re-programed” in the thymus, learning that the transplanted organ is harmless and can been seen as self. This is called immunological tolerance and, for the affected patients, it was a blessing in disguise! This mixture of cells with different fingerprints, from different people, in the body of a single person is called chimerism.
The development of immunological tolerance is considered the “holy grail” in transplantation, which means best or most perfect thing, like a treasure that’s really hard to get and therefore the goal of researchers all over the world. Scientists are now conducting studies on how to safely create chimerism in patients, “re-program” their immune system and make their immune cells tolerant toward the transplanted organ [6]. The ability to make transplant patients tolerant of their grafts would make life-long immunosuppressant medication unnecessary—preventing rejection and the nasty side effects from immunosuppressive drugs.
In summary, the bodies superhero immune cells target and attack any intruder, infections and transplanted organs alike. To prevent the immune cells from attacking the transplanted organ (rejection) powerful immunosuppressant medication is used to “handcuff” and disarm the recipient’s immune system. This medication, however, is a double-edged sword, as it also may cause unpleasant to life-threatening side-effects. Therefore, scientists are looking for ways to “re-program” the immune system to only attack threatening intruders and not a transplanted organ. This may enable patients one day to not rely on the strong effects, and suffer from side-effects, of immunosuppressants anymore.
Glossary
Immune System: ↑ Your immune system is like a team of superheroes that protects your body from intruders.
Antigen: ↑ Any substance that causes the body to start an immune response and produce antibodies for protection (e.g., toxins, chemicals, bacteria, viruses, and foreign cells).
Leucocytes: ↑ White blood cells with different specializations (T cells, B cells, NK cells, dendritic cells, …). Their main purpose is to keep the body healthy and fight off intruders and infections.
Antibodies: ↑ Small Y-shaped proteins produced by the immune system to stick to a specific antigen and help destroy it.
Fingerprint: ↑ Line marks on the skin of a person’s finger. Fingerprints are unique to every individuum and everyone’s fingerprints are different.
Organ Rejection: ↑ When the immune system attacks and ultimately destroys a transplanted organ.
Immunosuppressants: ↑ Medications that weaken the immune system on purpose, to prevent organ rejection. They have dangerous side effects like making people more susceptible to infections and cancer.
Immune Tolerance: ↑ teaching your body’s immune system to know the difference between “friends” like your own body, helpful bacteria or (in the case of transplantation) the new organ.) and “enemies”.
Chimerism: ↑ As used here, a state in which a mixture of immune cells from two different individuals exists inside the body of a single person.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the patients of the Division of Pediatric Nephrology and Gastroenterology for reading and Nina’s daughter Lisa (12) for her help with the figures.
References
[1] ↑ Calne, R. Y. 2012. It can’t be done. Nat. Med. 18:1493–5. doi: 10.1038/nm.2926
[2] ↑ Murphy, K. M., and Weaver, C. 2017. Janeway’s Immunobiology. 9th ed: New York: Garland Science.
[3] ↑ Danovitch, G. M. 2017. Handbook of Kidney Transplantation. Lippincott Williams & Wilkins (LWW).
[4] ↑ Harrison, J. H., and Merrill, J. P. 1956. Murray JE. Renal homotransplantation in identical twins. Surg. Forum. 6:432–6.
[5] ↑ Eder, M., Schwarz, C., Kammer, M., Jacobsen, N., Stavroula, M. L., Cowan, M. J., et al. 2019. Allograft and patient survival after sequential HSCT and kidney transplantation from the same donor-A multicenter analysis. Am. J. Transplant. 19:475–87. doi: 10.1111/ajt.14970
[6] ↑ Pilat, N., and Wekerle, T. 2010. Transplantation tolerance through mixed chimerism. Nat. Rev. Nephrol. 6:594–605. doi: 10.1038/nrneph.2010.110
