Abstract
A heart transplant is a life-saving surgical procedure that replaces a severely diseased or failing heart with a healthy heart from an organ donor. Donor hearts are matched to patients who need them based on factors like blood type, body size, and urgency. The transplant procedure involves removing the failing heart, connecting the donor heart to the major blood vessels, and ensuring the heart functions properly after surgery. Transplant patients need to take medications for the rest of their lives to prevent organ rejection, and they must receive ongoing monitoring for complications. While heart transplants significantly improve quality of life and survival rates, challenges like donor shortages and the risk of rejection persist. Advances in surgical techniques, donor management, and post-operative care continue to improve heart transplants, underscoring the vital role of organ donation in offering new hope to patients.
What is a Heart Transplant?
Sometimes, a person with a very sick, poorly working heart can get a new, healthy heart from an organ donor. This process is called a heart transplant. A heart transplant involves a surgery in which doctors replace a person’s diseased or failing heart with a healthy heart from a donor who has died and chosen to donate their organs. The donated heart can make a huge difference, allowing the recipient to live a much better and longer life.
The first heart transplant was performed in 1967, by a surgeon named Christiaan Barnard in South Africa. Barnard learned a lot from earlier work done by another surgeon, Norman Shumway, in the United States. The rest of this article will explain who might need a heart transplant, how hearts are donated, what happens during the operation, and what the outcomes are for people who receive new hearts.
Who Might Need a Heart Transplant?
Not everyone who has heart problems needs a heart transplant. Transplants are reserved for those with the most severe problems. There are several main reasons why someone might need a new heart [1].
The first reason is severe heart disease. Some people have serious heart conditions that damage their heart muscles, making the walls of the heart and its blood vessels weak or stiff. Heart diseases include conditions like cardiomyopathy, where the heart muscle becomes enlarged or thickened, and coronary artery disease, where the blood vessels that supply the heart with blood become narrow or blocked. These conditions can severely impact the heart’s ability to function properly. Severe heart disease can lead to heart failure, which happens when the heart cannot pump blood as well as it should. Heart disease can make it hard for a person to breathe and do everyday activities. Imagine your heart as a pump that pushes water through a hose. If the pump is weak, it cannot push enough water through, and the water flow slows down. Similarly, if the heart is weak, it cannot push enough blood through the body, causing fatigue and difficulty breathing.
Congenital heart defects are another common reason for heart transplants. Some people are born with heart problems that can be very serious and might require a transplant later in life. These defects can affect the structure of the heart and include holes in the heart, abnormal valves, or problems with the heart’s chambers. Sometimes these issues cannot be fully corrected with surgery, and a transplant becomes necessary. Finally, there are other heart conditions, like viral infections or inflammation, that can damage the heart so much that it needs to be replaced.
How are Hearts Donated?
Heart donation is a very generous act of giving after people have died. People can choose to become organ donors, usually when they get a driver’s license or sign up through an organ donor registry. In some countries, everyone is assumed to be an organ donor unless they decide to opt out. Becoming an organ donor is a decision to give others the gift of life after you pass away. The donor’s family should give their permission for the donor’s heart to be used in a transplant. Even if someone has registered already as a donor, their family should agree to the donation at the time of death. Special nurses are trained help families understand organ donation and guide them through the process in these situations.
When a donor heart becomes available, doctors look at a list of people who need a heart transplant to find the best match. Doctors consider the blood type, body size, and how sick the patient is. Matching is crucial to reduce the risk of rejection, in which the recipient’s body attacks the new heart. Once a match is found, the heart is checked to make sure it is functioning well, then it is removed from the donor’s body by expert surgeons. The heart is then carefully transported to the hospital where the recipient is waiting. Time is critical because the heart needs to be transplanted within a few hours after being removed from the donor’s body.
The Heart Transplant Operation
A heart transplant is a major operation and needs many doctors and nurses to work closely together, including cardiologists, transplant coordinators, surgeons, anesthetists, and intensive care specialists. Here is a step-by-step look at how a heart transplant is done [2, 3].
First, to prepare for the transplant, the recipient is put under general anesthesia, which means they will be asleep and will not feel anything during the surgery. Anesthesia helps ensure that the patient is comfortable and pain-free throughout the procedure. The surgeon then makes a cut in the chest and carefully accesses the heart. The patient is connected to a heart-lung machine, which pumps blood throughout the body during the operation.
The surgeon removes the failing heart by cutting through the major blood vessels that connect the heart to the body. This part of the operation is delicate and requires great precision to ensure the blood vessels that have been cut are ready to connect to the new heart (Figure 1). Once the sick heart is removed, the new, healthy donor heart is sewn into place, connecting it to the major blood vessels in the recipient. This ensures that blood can flow properly through the new heart.
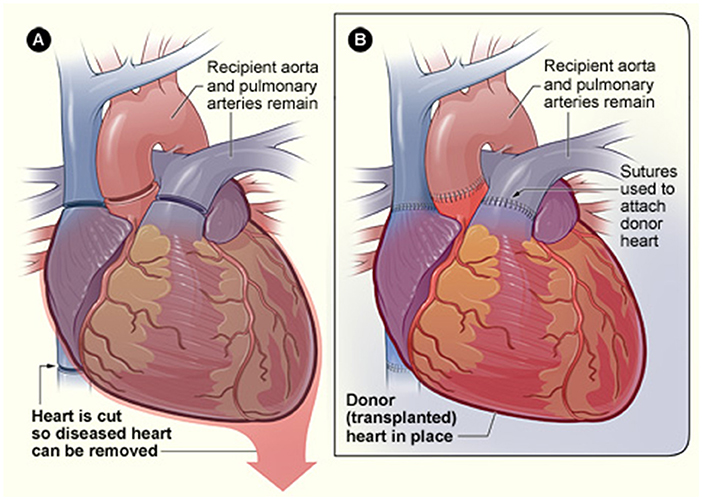
- Figure 1 - In a heart transplant, the recipient’s heart is removed and the donor heart is connected by joining the major blood vessels together.
- Once the heart receives a good blood supply, it will then start beating and pumping blood throughout the body. The time that the donor heart is outside of the body and without a blood supply must be kept as short as possible.
Once everything is connected, the new heart starts beating when its blood supply is returned. Sometimes doctors may need to give the new heart a little electric shock to get it going. They also use medications to help the heart start beating regularly and strongly. Finally, the surgeon closes the chest, and the recipient is moved to the intensive care unit (ICU) to recover. The chest is closed with wires, to put the breastbone back together, and stitches are used to close up the skin.
What Happens After a Heart Transplant?
Recovery from a heart transplant takes time and care. After the surgery, the patient stays in the ICU for a few days to make sure the new heart is working well. A transplant patient will spend several weeks in the hospital to ensure everything is healing properly. Doctors and nurses closely monitor the patient’s heart function, blood pressure, and overall health. Heart transplant recipients need to take special medicines called immunosuppressants for the rest of their lives. These medicines help prevent the body from rejecting the new heart. Without these drugs, the immune system would see the new heart as foreign and attack it.
After leaving the hospital, frequent visits to the doctor are necessary to check on the health of the new heart and make sure there are no complications. These check-ups include blood tests, heart biopsies, and imaging studies to monitor the heart’s condition and function. Transplant recipients are encouraged to eat healthy, exercise, and avoid smoking or drinking alcohol to keep their new hearts healthy. Maintaining a healthy lifestyle is crucial to the long-term success of the transplant. Transplant recipients must watch closely for any signs of infection, as they are more prone to getting sick because the immunosuppressants they must take can make infections more likely.
Long-Term Outcomes of Heart Transplants
A heart transplant can be life changing. Most people who get a heart transplant feel much better. They have more energy and can do things they could not do before, like walking longer distances and enjoying hobbies. Activities that were once difficult or impossible become possible again. People can live for many years after a heart transplant. With good care, some can live 10–20 years with their new hearts. Advances in medical care continue to improve the outcomes for transplant recipients.
There are challenges, too. The immune system always tries to reject the new heart, which is why immunosuppressants are so important. Sometimes, the new heart might develop problems, but doctors can help manage these issues. Regular monitoring and prompt treatment of any complications are essential. If you know someone who has had a heart transplant, being a good friend and offering support can make a big difference. Simple acts of kindness and understanding can help them through their recovery.
Donation is a Gift of Life
Heart transplants save lives. When people who are very sick and have no other treatment options get a new heart, they have a chance to live a full life. Because there are fewer donors than there are people in need of hearts, not all patients will get the chance to have a heart transplant. Some patients may have a heart pump inserted to give them more time to find a donor (Figure 2), but not everyone is suitable for this procedure and the pumps can have complications.
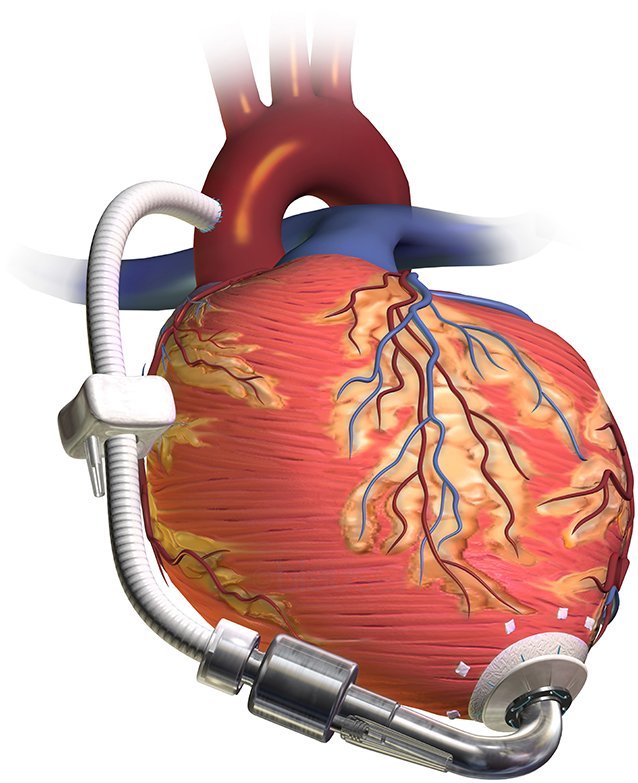
- Figure 2 - Heart pumps are sometimes used in patients to help with their heart failure.
- There are too few donor hearts for waiting patients, so these pumps can be used to keep the heart beating and keep patients alive while they wait for a donor organ. Heart pumps are powered by a battery outside the body, through a driveline cable that passes into the chest. When a donor heart becomes available, the pump and the recipient’s heart are removed together and replaced with the transplanted heart.
Heart transplantation is only possible because of the kindness of donors and their families. In short, organ donation provides a second chance at life for those who might otherwise have no hope [4]. By understanding who might need a heart transplant, how the process works, and what the outcomes are, we hope you are now better able to appreciate the incredible gift of a healthy heart. One day, you might be part of this life-saving process, whether by raising awareness or making the choice to donate your own heart [5].
Glossary
Donor: ↑ A person who has been declared dead by doctors or who has non recoverable brain damage. They can provide their heart and other organs to patients who need a transplant.
Recipient: ↑ The recipient is the patient who receives a heart transplant.
Congenital: ↑ The word to describe abnormalities or conditions that people are born with, rather than those that develop later in life.
Rejection: ↑ The body has an immune system that recognizes a donors heart as being from another person. Cells and antibodies in the blood attack the new organ in a process called rejection. Drugs are used to prevent or stop this.
Cardiologist: ↑ A doctor who has a specialist interest in heart diseases. This is different to a cardiac surgeon who does operations on the heart and performs heart transplant surgery.
Anesthetists: ↑ Doctors that use various drugs to make patients temporarily unconscious and pain free during surgeries. They keep patients stable during surgery and look after them on intensive care.
Intensive Care Unit (ICU): ↑ A hospital ward where patients with complicated issues go for specialized care, including after major surgeries like heart transplants.
Immunosuppressants: ↑ A combination of drugs taken by patients after a transplant to prevent the body from rejecting the new organ. These drugs must be taken forever.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Mehra, M. R., Kobashigawa, J., Starling, R., Russell, S., Uber, P. A., Parameshwar, J., et al. 2006. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates. J. Heart Lung Transplant. 25:1024–42. doi: 10.1016/j.healun.2006.06.008
[2] ↑ Abbas, M., El-Sabawi, B., and Nurok, M. 2013. Current surgical techniques in heart transplantation. Ann. Cardiothorac. Surg. 2:34–42.
[3] ↑ Mahle, W. T., and Kanter, K. R. 2009. Heart transplantation in pediatric patients: recipient selection and outcome. Pediatr. Transplant. 13:89–99.
[4] ↑ Reich, H. J., and Czer, L. S. C. 2014. Donor selection and management in heart transplantation. J. Thorac. Dis. 6:1080–89. doi: 10.3978/j.issn.2072-1439.2014.08.27
[5] ↑ Al-Obaidi, M. N., Hashim, A. T., and Faggian, G. 2023. Heart transplantation: current status and challenges. J. Heart Lung Transplant. 40:15–30.
