Abstract
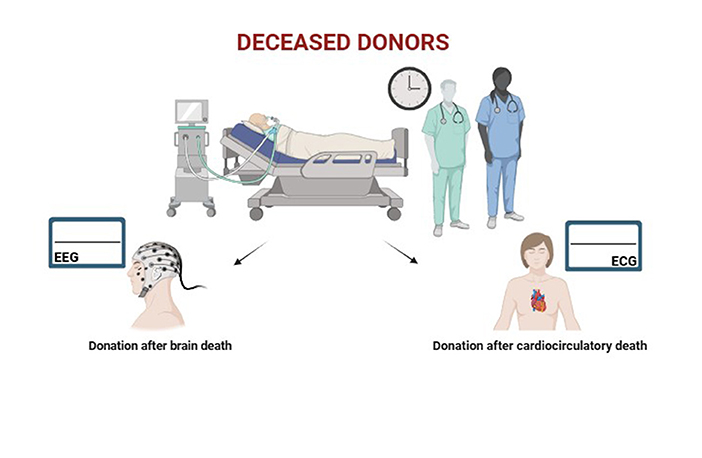
The human body is an extraordinary machine that works through the actions of many organs and tissues, such as the kidneys, liver, heart, lungs and cornea, each one carrying out a specific function that helps to keep us alive and functioning. Unfortunately, diseases can cause organs to break down, the so-called organ failure, sometimes putting a person’s life or wellbeing in danger. The good news is that medical science has developed ways to successfully implant a healthy organ into a patients when one of their own organs has stopped functioning. The sad news is that there are not enough available organs for those in need. Who can give organs? People can donate their organs when, at the end of their lives, the brain loses its vital activities. But medical science has also found ways to let living people safely give part of an organ (or one organ when there are two, like the kidneys), with minimal risk for the donor’s health.
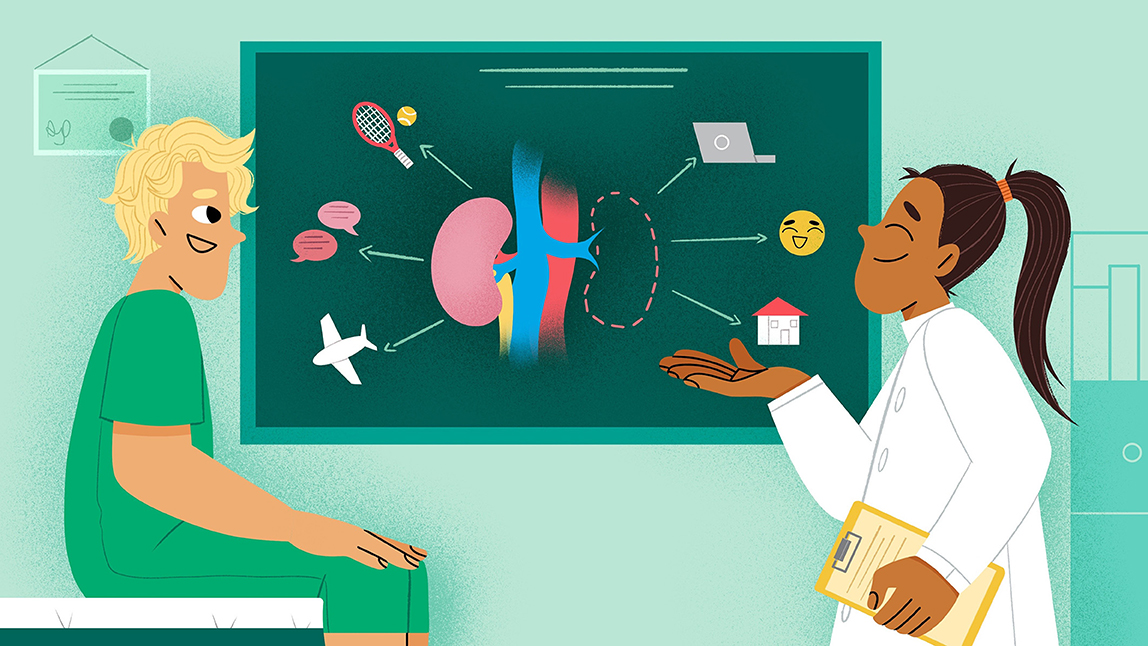
Every year, many people all over the world need new organs to continue enjoying their lives. This is possible thanks to transplantation. Transplantation is a medical procedure that consists of replacing a diseased, no longer functioning organ or tissue, or one suffering form “organ failure”, with a healthy one from another healthy person, called donor (Figure 1). Organ donation is an active choice made freely by the donor, and it is an anonymous act, meaning the person who receives the organ may not know who the organ came from [1].
- Figure 1 - Many organs and tissues can be donated.
An organ is a structure in the body composed of multiple types of cells that work together to perform a specific task. For instance, the liver is composed of several cell types with fancy names like hepatocytes, cholangiocytes, Kupfer cells, and endothelial cells. Various cells group together to form tissues, which perform the organ’s tasks.
Transplantation of an organ between two individuals of the same species, like between two humans, is called allotransplantation. When the organ comes from another species, such as when a heart or kidney from a pig is transplanted into a human, this is called xenotransplantation. Finally, the term autotransplantation describes when doctors transplant a tissue or organ from one place to another in the same individual, for example, skin or bone to fill a hole caused by a traffic accident. Finally, our tissues also contain special cells called stem cells that can produce every other type of specialized cell. The most widely used stem cell transplantation is the transplantation of hematopoietic stem cells, to help treat blood cancers or other blood diseases.
For the rest of this article, we will use the term “transplantation” to refer to allotransplantation of solid organs such as the kidney, liver, heart, lung, pancreas, gut, or various combinations of these organs.
Thanks to advances in modern medicine and an increasingly efficient organizational network that keeps track of potential donors and recipients, transplantation is now a routine procedure that saves thousands of lives every year, worldwide. The sad news is that there are not enough available organs for those in need, so, for the time being, not all people are guaranteed a new life through an organ transplant. Until doctors can produce organs and stem cells in the laboratory, more donors must become available to save the lives of the many patients in need.
So, who can give an organ? All healthy people can potentially become organ or tissue donors. Organ and tissue donors can be either deceased (no longer alive) or living.
Deceased Donors
Deceased donors are people who are no longer alive. While they were still alive, these people expressed their desire to donate their organs after they died. In the past, most deceased donors were young healthy people who died in traffic accidents. Nowadays, to increase the number of available organs, elderly people make up an increasing proportion of deceased donors. Doctors first make sure the organs are functioning as well as they should be.
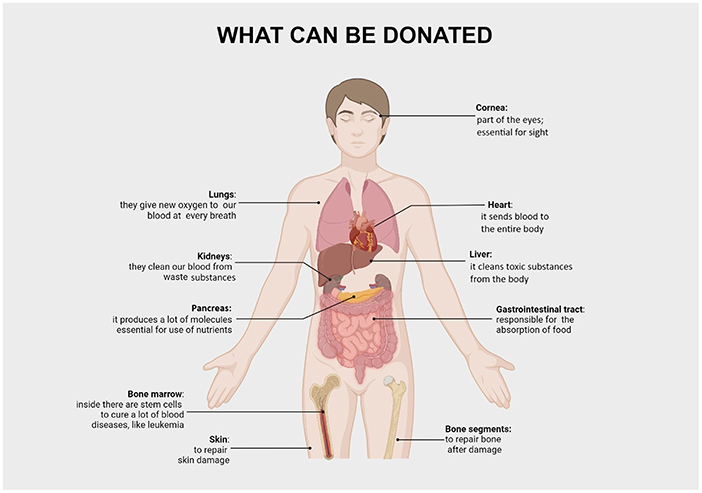
There are two types of deceased donors (Figure 2). Donors after brain death are people who lost all their brain functions forever. For example, severe head injury can cause massive damage to the brain, leading to brain cell death. When this occurs, the person’s other organs may be functioning, but the person will never wake up and breathe on his/her own. Although such people are no longer alive, they may look like they are because a machine pumps air into their lungs, allowing the heart to beat for a while, to continue sending blood with oxygen and nutrients to the organs. Every country of the world has strict laws for diagnosing brain death. The laws are based on various tests performed by specialized doctors, proving that every function of the brain has stopped forever.
- Figure 2 - There are two types of deceased organ donors, meaning people who donate their organs after death.
- In donation after brain death, the donor’s brain has permanently stopped working, which means the donor is no longer alive even though machines are keeping their heart beating and lungs breathing. In donation after cardiocirculatory death, the blood has permanently stopped flowing. With no blood flow, every organ will be damaged. Machines can keep the blood flowing until the organs are ready for transplantation.
On the other hand, donors after cardiocirculatory death are people whose blood has stopped flowing forever. Without blood, the body and the brain will no longer function. After several minutes with no blood flow, every organ will be damaged beyond repair. There are machines that can temporarily restore blood flow, to prevent any damage to the organs before doctors get those organs for transplantation. Blood flow can stop when the heart stops beating, which is called cardiac arrest. Cardiac arrest can occur either out of or in the hospital. Sometimes doctors see that the treatments they are using to support the lungs and blood flow are not helping and will not make the person better—therefore, doctors might decide to stop those treatments. Doctors want to make sure the patient is comfortable and not in pain during his/her last days. Once the treatments keeping the lungs and heart functioning are stopped, the patient will have cardiac arrest and die. Then these patients can be considered potential organ donors.
Each potential organ donor must be evaluated before organ retrieval, to make sure they do not have dangerous diseases that could be transmitted to organ recipients. International procedures are in place through which relatives are interviewed and a number of tests are performed to rule out any risky condition.
Living Donors
The very first transplantation, conducted 70 years ago, was a kidney transplantation from a living donor. Doctors have safely performed hundreds of thousands of living transplantations ever since, all over the world. Living donor transplantation is possible for organs that naturally exist in pairs, such as the lungs and kidneys, in which one organ is donated and the other is left in place. For some organs (liver, pancreas, gut) it is possible to take a part of the organ without damaging its overall function. The quality of organs from living donors is usually superior to that of deceased donors, allowing the recipient an even healthier life. Living donor transplantation also enables doctors to plan the day of transplantation. Therefore, recipients of organs from living donors know in advance the exact date when they will possibly be cured of their disease. Patients who do not have a suitable living donor must wait an unknown length of time for a transplant from a deceased donor. It can be months or years before a suitable organ is available.
Living donors can be related (mum, dad, brother, sister) or can be unrelated but with an emotional or social relationship with the recipient (wife, husband, friend). All potential donors must be evaluated to ensure that the donation will not negatively affect the donors’ health for the rest of their lives. For this reason, people with illnesses (for example heart, kidney, or lung disease; cancer; chronic infection), or with other signs that they are at risk of developing an illness after donation, are not accepted as living donors. Organ donation is one of the rare situations in which a healthy person undergoes surgery, and that is why it is so important that donors can continue their normal lives afterwards (Figure 3).
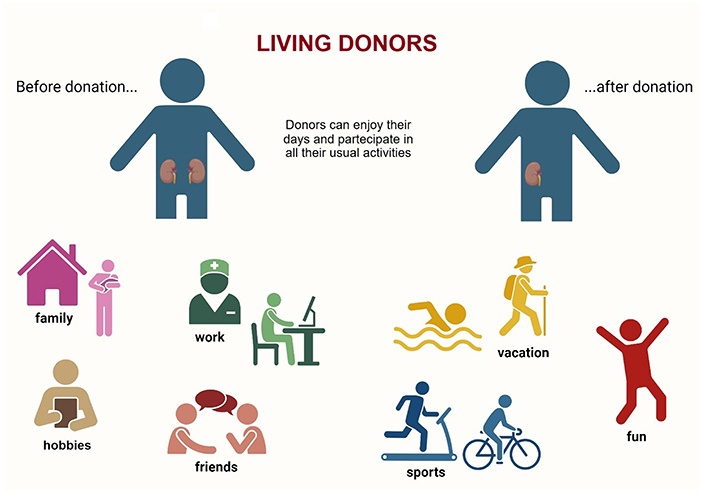
- Figure 3 - Living donors can enjoy a normal life after they donate organs.
Compatibility Between Donor And Recipient
After assessing the suitability of the donor, the organ recipient must be found. The first step is identifying the blood type of both the donor and the recipient. There are four different blood types: group A, B, AB and 0. In addition, everyone has a different set of molecules on all their cells, called HLA alloantigens. What matters the most for a safe transplantation is that, before transplantation, recipients do not have antibodies that will attack the donor’s blood or organ alloantigens. Doctors test for these antibodies and, if they exist, the recipients must receive specialized treatments before transplantation, to prevent organ rejection from occurring. The donor’s gender does not matter, as organs work equally well even if they come from a person of the opposite gender. The donor’s gender does not affect the character of the organ recipient in any respect. If you want to learn even more about organ donation, check out this link.
The Future Of Organ Donation
Since the number of available organs is not enough for all the people who need transplants, researchers are working hard to solve this problem. If studies in the upcoming years will show satisfactory results, xenotransplantation could become a new hope for patients, especially for those waiting for life-saving transplantation of a heart, for example [2, 3].
In summary, people affected by major organ problems can hope to live long, healthy lives thanks to the generosity of other people. This article has described several kinds of organ donors and the ongoing work of medical science to find new strategies. Now it is your turn! Enjoy a healthy and beautiful life, but do not forget to become a donor so that you too may have the opportunity to help others do the same!
Glossary
Organ Failure: ↑ An organ that stops functioning due to disease.
Donor: ↑ Persons who decide to donate their organs after death
Organ: ↑ A structure in the body composed of multiple types of cells that work together to perform a specific task.
Tissue: ↑ A set of various cells.
Allotransplantation: ↑ Transplanting organs from different individuals of the same species (e.g., humans).
Xenotransplantation: ↑ Transplanting organs from another species into humans. This procedure is not yet ready for day-to-day medical practice.
Autotransplantation: ↑ Transplanting a tissue or organ from one place to another in the same individual, for example, skin or bone to fill a hole caused during a traffic accident.
Alloantigen: ↑ Molecules present on all cells that another person’s body might recognize as foreign, putting a transplanted organ at risk.
Organ Rejection: ↑ It is the organism’s attempt to destroy the transplanted organ because it is recognized as foreign.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Sever, M. S., Mueller, T. F., Oniscu, G. C., Schena, P., and Vanholder, R. Facts and myths about altruistic organ donation. Nephrol. Dial. Transplant. (2024) 39:1218–1220. doi: 10.1093/ndt/gfae039
[2] ↑ Porrett, P. M., Orandi, B. J., Kumar, V., Houp, J., Anderson, D., Cozette Killian, A., et al. First clinical-grade porcine kidney xenotransplant using a human decedent model. Am. J. Transplant. (2022) 22:1037–1053. doi: 10.1111/ajt.16930
[3] ↑ Mallapaty, S., and Kozlov, M. First pig kidney transplant in a person: what it means for the future. Nature. (2024) 628:13–14. doi: 10.1038/d41586-024-00879-y