Abstract
Sometimes, when organs like the kidneys or liver get sick, the only way to make people better is by replacing the sick organ with a healthy one. This special surgery is called organ transplantation, and the person who gets the new organ is called the recipient. White blood cells in the recipient’s body, which act like soldiers to protect people from microbes that make them sick, might think the new organ is a dangerous invader and try to destroy it. To prevent this attack on the new organ, recipients need to take special drugs called immunosuppressive agents, which make their soldier cells “sleep”. However, these drugs can make the recipient more likely to get sick from microbes, and they might develop diseases like pneumonia, urinary or wound infections. In this article, we will discuss the main characteristics of infections in transplant recipients and what can be done to prevent them.
What is Organ Transplantation?
Organ transplantation is a special kind of surgery in which a sick organ is replaced with a healthy one from another person. The person who gives the organ is called the donor and the person who receives it is called the recipient. Sometimes, organ transplantation is the only way to cure a disease, and it can save lives [1]. A lot of organs can be transplanted: kidney, liver, heart, lung, pancreas, and intestine. However, the donor organs must be perfectly functional to be transplanted. For example, if the donor is ill or suffers from an infection, their organs cannot be donated. In addition, before donor organs are transplanted into the recipient, they are carefully stored in the cold and covered with liquids that keep them in good condition until they reach the recipient. Medical professionals are careful to preserve the organs as much as possible.
There are two types of donors. Sometimes, a person who is still alive can donate an organ—such people are called living donors. For example, someone can donate a kidney because people can survive well with only one of the two they are born with. Also, in some cases, a part of the liver can be donated because the liver can grow back. People can also donate their organs to others after they die—these are called deceased donors. A single deceased donor can save multiple lives with their organs. Doctors check to make sure the deceased donor’s organs are in good shape before the transplant. Most transplants occur thanks to this generous gift from deceased donors.
Why is it Important for Soldier Cells to Sleep After a Transplant?
One of the biggest challenges for people who have had an organ transplant is dealing with infections. Infections can be caused by many types of microbes such as viruses, bacteria, fungi, and parasites. Our bodies defend themselves from infections thanks to cells called white blood cells, which act like soldiers that fight off dangerous invaders. However, the white blood cells can think that a transplanted organ is an enemy, and then they try to destroy it. This reaction is called rejection. Doctors work hard to prevent and manage rejection by giving transplant recipients special medicines called immunosuppressive agents and monitoring transplant recipients closely. These medicines make the white blood cell soldiers go to sleep. Unfortunately, this means that transplant recipients are also more likely to get infections. So, doctors need to find the right balance between protecting the new organ and keeping the person safe from infections. If the patient gets too much medicine, the person’s body cannot fight off infections well, and they can get sick more easily. If the patient gets too little medicine, the person’s body might reject the new organ, which means the new organ might stop working [2].
Why are Infections After Transplantation so Dangerous?
Transplant recipients are more likely to develop infections due to the white blood cell soldiers “napping”. Because of this, the body might not show the usual signs of being sick, like having a fever, chills, or pain, or feeling tired. The signs of infection might be weaker or show up later than they should. When it is more difficult for doctors to know that the patient has an infection, the patient might not be treated soon enough and the infection may spread to other parts of the body. Thus, managing infections after transplantation can be challenging, and it might affect the patient’s health and how the transplanted organ works.
Infection Risk and Timeline
Some transplant patients have a higher chance of getting infections than others. For example, people who receive a lung transplant are more likely to catch viruses that affect the lungs, like the viruses that cause the flu or COVID-19. Also, as patients get older, their risk of infections can increase. If the transplant surgery is very difficult, it can also become easier for transplant patients to get infections. Doctors must consider all these factors to figure out how likely it is that a transplant patient will get infections.
When predicting the risk of infection, doctors generally consider 3 main time periods related to when the surgery was performed: the early days after transplant, 1–6 months after the transplant, and 6 months or more after the transplant (Figure 1) [1].
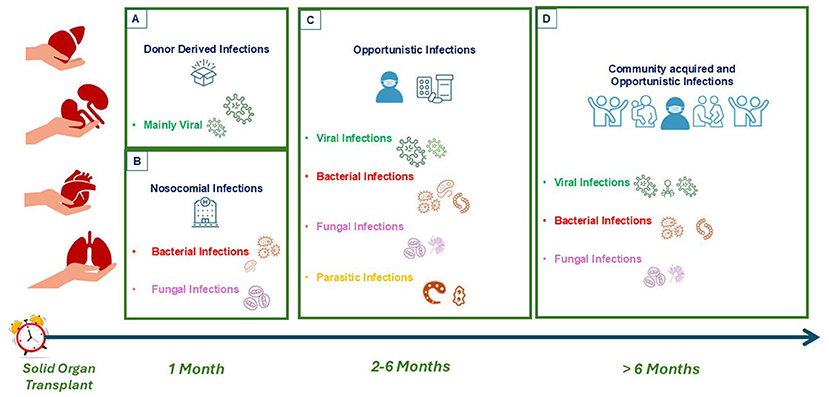
- Figure 1 - Timeline of infections in organ transplants.
- Up to about 1 month after transplantation, (A) donor-derived infections from the transplanted organ and (B) nosocomial infections (caught during the hospital stay) are the biggest worry. (C) From 2–6 months after transplantation, opportunistic infections are common. These are infections from microbes that do not usually cause problems in healthy people. (D) From 6 months post-transplantation, transplant patients are generally susceptible to infections spread in everyday places like schools or playgrounds where people interact with one another.
During the 1st days to weeks after transplantation, the recipient is still in the hospital recovering from the surgery. Most of the infections during this time are the same as the infections seen in other hospital patients after other types of surgeries. These are called nosocomial infections (nosokomio means hospital in Greek). Nosocomial infections can be different depending on the type of transplant. For example, people with new kidneys might get urinary infections, and those with new lungs might get pneumonia—a lung infection usually caused by bacteria. Unfortunately, all over the world, bacteria have found ways of surviving the drugs that doctors use to fight infections—making it harder to get rid of the infections they cause. This is known as antimicrobial resistance and it is more dangerous for people with weaker defenses, like transplant recipients [3].
In the period between 1 month and 6 months after the transplant, the medicines to stop the body from rejecting the organ are the strongest. This makes it easier for microbes that do not usually bother healthy people to cause problems, which are called opportunistic infections. Types of opportunistic infections can vary depending on where the person lives. Sometimes, the microbe is already in the person’s body in a “sleeping” form, but it can wake up after a transplant. This can happen with some viruses (for example the cytomegalovirus, a cousin of the virus that causes chickenpox) or bacteria like the kind that cause tuberculosis. However, the number of opportunistic infections has decreased in recent years, because doctors give patients drugs to keep these microbes from waking up.
Finally, after 6 months, the risk of infections goes down because the immunosuppressive medicines are less strong. But transplant patients can catch bacteria and viruses from the community more easily than most people, such as microbes that cause the flu or pneumonia.
An Unexpected Gift: Donor-Derived Infections
A very rare but sometimes difficult problem with organ transplants is getting an infection from the donor organ. This is called a donor-derived infection. These infections can come from bacteria, fungi, viruses, or parasites present in the organ. To prevent this, doctors check donors very carefully. If they find an infection, they might treat it before the donation or give the recipient special medicine during the transplant. When checking a donor, doctors look at things like where the donor is from, if they have traveled to places with lots of infections, and if they have a fever or other symptoms suggestive of infection at the time of donation. If the donor is alive and has an infection, the transplant can be delayed until the infection is gone. But if the donor has died, the donation might be stopped if doctors find an infection that is hard to treat. Otherwise, specific drugs will be used during surgery to avoid the spread of the infection to the organ recipient [4]. Although donor-derived infections are a risk, most patients are very sick while they are waiting for a transplant, so the risk is usually worth it for the patients’ long-term health.
Preventing Infections in Organ Transplant Recipients
Some of the infections that happen in transplant recipients can be prevented by vaccines. Vaccines are medicines that help the body to defend itself against diseases. They work by showing the body a very weak version of the microbes that cause a disease. This weak version will not make people sick, but it helps the body’s soldiers learn to recognize and fight the real germs if they show up later. So, if a vaccinated person meets the real microbe in the future, their body will already know how to defend itself and keep them from getting sick. Every patient waiting for a transplant needs to check which vaccinations are necessary. It is best to get these vaccines before the transplant [5]. Some vaccines using living organisms cannot be given in transplant recipients due to the risk of severe infections that may develop.
Besides vaccines, some medicines can help protect recipients from microbes that cause illness. These medicines are called prophylaxis. They help prevent bacterial, fungal, and viral infections. Transplant patients might need to take these medicines for a long time, up to 6–12 months after the transplant, to avoid getting sick [1].
Final Insights
Now you have learned about what a transplant is and why people need to take special medicines to help their bodies accept their new organs. These medicines, called immunosuppressive agents, are important to prevent transplant rejection, but they also make it easier to get infections. We told you about when these infections appear after transplant, and how doctors follow and prevent infections. Managing infections in people with transplants is complex but exciting work. That is why doctors are always doing research to find better ways to stop infections and their effects after transplantation. Thanks to this research, most transplant patients can live healthy lives without worrying too much about infections.
Glossary
Donor: ↑ The person who gives the transplanted organ is called the donor.
Recipient: ↑ The person who receives the transplanted organ is called the recipient.
Rejection: ↑ A reaction of the recipient’s white blood cells, which think that the transplanted organ is an enemy so they try to destroy it.
Immunosuppressive Agents: ↑ Drugs used to stop the recipient’s white blood cells from attacking the transplanted organ.
Nosocomial Infection: ↑ An infection that someone gets while staying in a hospital. The name comes from the Greek word nosokomio, which means hospital.
Antimicrobial Resistance: ↑ When bacteria become so strong that the antibiotics doctors use to kill them no longer work.
Opportunistic Infections: ↑ Infections caused by microbes that do not bother healthy people. These microbes can cause infections in transplant patients due to the reduced activity of their white blood cells.
Prophylaxis: ↑ Medicines can protect transplant recipients from microbes that cause illness.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Fishman, J. A. 2017. Infection in organ transplantation. Am. J. Transplant. 17:856–879. doi: 10.1111/ajt.14208
[2] ↑ Nelson, J., Alvey, N., Bowman, L., Schulte, J., Segovia, M. C., McDermott, J., et al. 2022. Consensus recommendations for use of maintenance immunosuppression in solid organ transplantation: endorsed by the American College of Clinical Pharmacy, American Society of Transplantation, and the International Society for Heart and Lung Transplantation. Pharmacotherapy 42:599–633. doi: 10.1002/phar.2716
[3] ↑ Soave, R. 2001. Prophylaxis strategies for solid-organ transplantation. Clin. Infect. Dis. 33:S26–S31. doi: 10.1086/3209014
[4] ↑ Wolfe, C. R., Ison, M. G., and AST Infectious Diseases Community of Practice. 2019. Donor-derived infections: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transplant. 33:e13547. doi: 10.1111/ctr.13547
[5] ↑ Danziger-Isakov, L., Kumar, D., and AST ID Community of Practice. 2019. Vaccination of solid organ transplant candidates and recipients: guidelines from the American society of transplantation infectious diseases community of practice. Clin. Transplant. 33:e13563. doi: 10.1111/ctr.13563