Abstract
Have you ever noticed itchy, red patches on your skin that just will not go away? You might have a condition called psoriasis. In this article, we will explore what psoriasis looks like and its causes. We will talk about how treatments can help, in the form of creams, ointments, light therapy, and medicines that work all over the body. We will also look at how psoriasis can affect a person’s daily life and what people can do to feel better. With the right care and treatment, kids can manage psoriasis and continue with all their amazing adventures!
What are Those Red, Itchy Patches On Your Skin?
Psoriasis is a skin condition that can cause thick, red patches, called plaques, covered with silvery scales. These patches can be very itchy and uncomfortable. Psoriasis can appear at any age, but for kids, it usually happens between ages 8 and 11. In North America, around 20,000 children are diagnosed with psoriasis each year, and about one-third of adults with psoriasis also had it as kids [1]. Having psoriasis can be tough, and sometimes kids worry about passing it on to their friends. But psoriasis is not contagious—it just means that some of the skin cells work differently! Skin has many important functions, like acting as a barrier to protect the body and fighting off intruders with immune system cells.
So, why do some people get psoriasis while others do not? That is a great question, and scientists around the world are still figuring it out. What they do know is that the immune system, genetics, and environment all play a role in whether a person develops psoriasis.
The skin, officially known as the integumentary system, is the body’s largest organ, which also includes hair, nails, and glands. The skin has three important layers: the epidermis, dermis, and hypodermis (Figure 1). Each layer has unique jobs and special cells to help carry out those jobs [2].
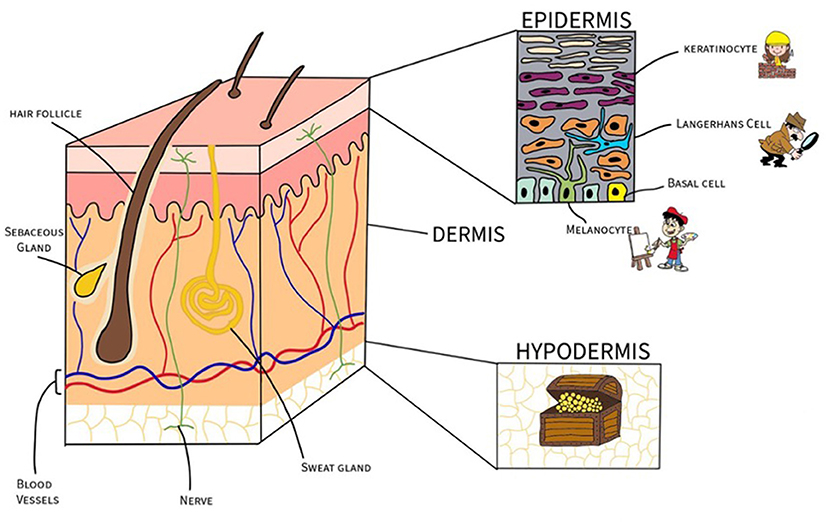
- Figure 1 - The layers of the skin: the epidermis, dermis and hypodermis.
- Each layer is shown with its corresponding cells: keratinocytes (bricklayers), melanocytes (artists), Langerhans cells (super spies), basal cells, and adipocytes (fat cells). Also shown are structures within the dermis: hair follicles, sebaceous (oil) glands, blood vessels, and nerves.
The outermost layer of the skin is called the epidermis. It contains cells called keratinocytes, which are like bricklayers. They build a strong wall to protect the body by keeping intruders out. Melanocytes are like artists—they make melanin, which gives the skin its color and helps protect it from the sun. Langerhans cells are also found in the epidermis. These cells are like spies—they watch out for intruders and warn the immune system to start fighting germs. Deep inside the epidermis, basal cells act like factories that make new keratinocytes to keep the wall strong.
Beneath the epidermis lies the dermis, a thick layer of substances called collagen and elastin, which keep the skin firm and stretchy. The dermis is packed with blood vessels that deliver nutrients, nerve endings that pass information to the brain, sweat glands for cooling the body down, hair follicles for trapping heat, and sebaceous glands for producing oil to keep the skin soft. Phew, that is a lot of functions!
The deepest layer, the hypodermis, is like a treasure chest filled with fat cells. Fat cells store energy like precious treasures, ready to be called into action whenever the body needs an extra boost. This fatty layer also acts like a warm blanket, keeping the body nice and toasty, even when it is chilly outside.
What Causes Psoriasis in Children?
As we mentioned earlier, there is no simple explanation for what causes psoriasis, but scientists do know that it involves the immune system, genes, and the environment. These three elements come together like pieces of a puzzle to cause psoriasis. Let us dive into each puzzle piece.
Immune System
The immune system is the body’s superhero team, fighting off intruders to keep people healthy. It is made up of many kinds of cells all working hard as a team. Langerhans cells, as we already mentioned, are immune cells that hang out in the epidermis and act like spies. They alert their friends the T-cells when there is danger. The T-cells act as guards, and when they are alerted to this danger they release cytokines—little messenger molecules that send signals back to the keratinocytes, telling them to grow fast and multiply (Figure 2). When somebody has psoriasis, the T-cells can get a little confused and continue to send out cytokine danger signals long after the danger has gone, leading to the production of too many keratinocytes. This causes inflammation, leading to the thick, red, swollen, and often itchy skin patches that are a symptom of psoriasis [3].
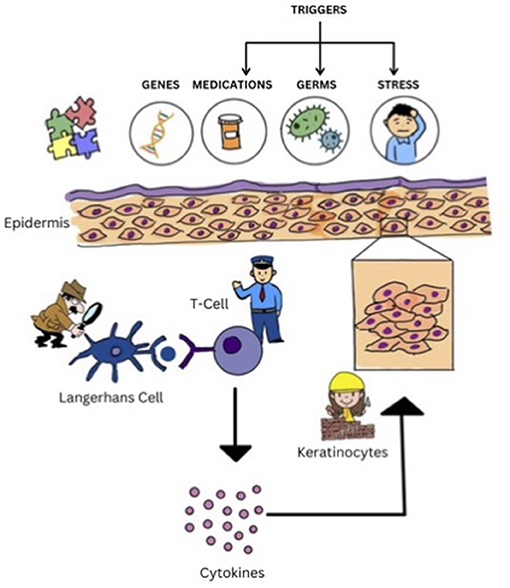
- Figure 2 - Puzzle of psoriasis: genes, medicines, germs, and stress can disrupt the skin’s immune system “superhero team” and destroy the skin barrier (epidermis).
- The Langerhans cells (spies) signal the T-cells (guards) that release cytokines. Cytokines are messengers that send signals to the keratinocytes (bricklayers) to make them grow and multiply, which leads to thick, red, scaly patches on the skin.
Genes
Genes are like tiny instruction guides inside almost every cell in the body. They give the body directions on how to grow and work, determining things like skin color, eye color, and even how the immune system works to fight off sicknesses. You get your genes from your parents, so if someone in your family has psoriasis, you might get it too. Scientists have found a special gene, called PSOR1, that is connected to psoriasis. If this gene is not working properly, it can confuse the Langerhans cells. When this happens, the skin can start making too many cells too quickly, leading to the red, itchy patches seen in psoriasis [4].
Environment
Having the PSOR1 gene does not always mean that a person will get psoriasis. Certain things in the environment can trigger it, such as certain medicines, infections (like a sore throat), and stress. These triggers can either cause psoriasis to start or make it worse (Figure 2) [1].
What Does Psoriasis Look Like?
Psoriasis does not look the same for everyone. There are lots of different types of psoriasis, and each has a unique appearance.
The most common type is plaque psoriasis, which looks like thick, red patches on the skin, covered with silvery flakes. These patches can be itchy and are usually found on the elbows, scalp, knees, back, or even the palms of the hands and soles of the feet (Figure 3). Plaque psoriasis often appears on both sides of the body in the same spot—so if it is on one elbow, it is likely on the other side, too. In small babies, it can show up in the diaper area.
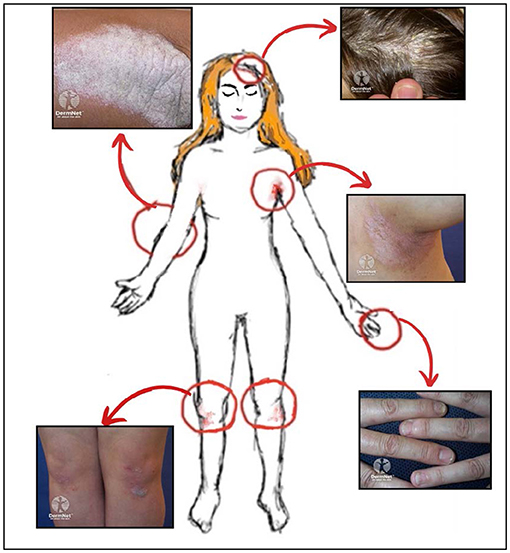
- Figure 3 - Common locations for plaque psoriasis on the body include the surfaces of the knees and elbows, the armpits, as well as the scalp and the nails.
- Images sourced from DermNet NZ under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 (New Zealand) license. See images at: DermNet NZ—Psoriasis.
Psoriasis can sometimes show up as small, round, red spots called guttate psoriasis, which might happen after a person has a sore throat. Other times, it appears in warm, moist areas of the body like the armpits or under the breasts. This is called inverse psoriasis.
In rare cases, psoriasis can look like small, pus-filled bumps or can even affect the whole body, making the skin very red and scaly. Psoriasis does not just affect the skin, it can also change how the nails look, making them rough, thick, crumbly, and yellow or brown in color.
Things like stress, cold weather, certain medicines, or getting sick can cause flare-ups, which are times when psoriasis gets worse. These flare-ups can last for a few weeks or months, but they eventually calm down [3].
Although psoriasis is a life-long condition, many treatments can help improve the appearance of the plaques and make living with psoriasis a lot easier. Psoriasis can be treated step by step, depending on how the patient’s body is affected.
The first step is usually special creams or ointments patients put on their skin. These are called topical treatments. They help reduce the red, itchy patches and make the skin look and feel better. Some creams work by calming the skin, while others help keep the skin soft and remove dry, flaky skin. If psoriasis affects the scalp, there are special shampoos that can help, too [5].
If creams do not work well enough, doctors might use light therapy. This treatment uses a type of light called UVB light, which is a part of sunlight that is not visible to humans, to reduce redness and itching. Light therapy helps slow down how quickly skin cells grow, making the patches smaller and less itchy. Doctors make sure that this special light is used safely during therapy [6].
For more serious psoriasis, doctors might use medicines that work throughout the whole body, not just on the skin. These medicines can be taken as pills or given as injections. They help by calming down the immune system, which is what causes the red, itchy patches in the first place. Some newer medicines, called biologics, are especially good at reducing inflammation and can make a big difference to those red, itchy patches. If one treatment is not enough, doctors might combine treatments to help the skin get better [4].
General Skin Care
It is important for everyone—not just psoriasis patients—to keep their skin healthy. For example, you can use moisturizer to keep your skin soft and avoid harsh soaps or products that can irritate the skin and make psoriasis worse. Everyone should wear sunscreen (at least SPF 30) when they go outside. Finally, for psoriasis patients, it is important to avoid triggers that can make psoriasis worse, like stress or certain medicines.
What is the Impact of Psoriasis?
Living with psoriasis can be tough, especially for kids. Those itchy and bothersome patches can make it hard to get a good night’s sleep, go to school, or join in on sports and fun activities. It is normal for kids with psoriasis to feel a little different from their friends and to feel upset or embarrassed sometimes. But if you develop psoriasis, do not worry! Thanks to the fantastic treatments available, psoriasis does not have to negatively affect a kid’s daily life. With the right care and support, kids with psoriasis can feel confident and keep enjoying all the things they love to do!
Glossary
Plaques: ↑ Thick, red, raised patches of skin covered with silvery scales, commonly found in psoriasis.
Immune System: ↑ The body’s defense system (superhero team) that fights off germs and keeps you healthy.
Langerhans Cells: ↑ Immune cells in the skin (spies) that help detect infections and tell T-cells (guards) to fight them. In psoriasis they become confused, causing skin cells to grow too quickly.
Cytokines: ↑ Tiny proteins released by T-cells that act like messengers. They tell other cells how to respond to danger and, in psoriasis, they can cause skin cells to grow too quickly, causing inflammation.
Inflammation: ↑ The body’s response to injury or infection, often characterized by redness, swelling, and warmth in affected areas, like the skin.
Triggers: ↑ Things like stress, sickness, or certain medicines that can make psoriasis worse or start it.
UVB Light: ↑ A special invisible light from the sun that helps slow down the growth of skin cells and makes red, itchy psoriasis spots feel better and look calmer.
Biologics: ↑ Medicines that work throughout the whole body, blocking immune system signals that cause inflammation, helping to reduce psoriasis symptoms like redness and itching.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Cohen, M., and Deckel, B. 2023. “An overview of pediatric psoriasis”, in Dermatology Times. Available at: https://www.dermatologytimes.com/view/an-overview-of-pediatric-psoriasis (accessed April 14, 2024).
[2] ↑ Tortora, G. J., and Derrickson, B. 2017. Principles of Anatomy and Physiology (15th ed.). Hoboken, NJ: John Wiley.
[3] ↑ Mahé, E. 2016. Childhood psoriasis. Eur. J. Dermatol. 26:537–548. doi: 10.1684/ejd.2016.2932
[4] ↑ Branisteanu, D. E., Georgescu, S., Serban, I. L., Pinzariu, A. C., Boda, D., Maranduca, M. A., et al. 2021. Management of psoriasis in children (Review). Exp. Therapeut. Med. 22:1429. doi: 10.3892/etm.2021.10864
[5] ↑ Fluhr, J. W., Cavallotti, C., and Berardesca, E. 2008. Emollients, moisturizers, and keratolytic agents in psoriasis. Clini. Dermatol. 26:380–386. doi: 10.1016/j.clindermatol.2008.01.015
[6] ↑ Institute for Quality and Efficiency in Health Care (IQWiG). 2021. “Psoriasis: Learn more – Does light therapy (phototherapy) help reduce psoriasis symptoms?”, in InformedHealth.org. Cologne: Institute for Quality and Efficiency in Health Care (IQWiG). Available at: https://www.ncbi.nlm.nih.gov/books/NBK435696/ (accessed May 6, 2024).
