The brain is a complex organ and neuroscientists are using many different methods to try to understand – and perhaps even change – how the human brain works. Before this research can take place; however, researchers must ensure that their work is ethical. In this review article, we introduce the exciting field of neuroethics and describe the three key ethical principles by which all human research studies must abide. We also describe four research studies that neuroethicists at the National Core for neuroethics have carried out to give you an idea of the range of work that is being done by those who are interested in the ethics of neuroscience and the neuroscience of ethics.
The Three Key Ethics Principles
Three of the most common ethical principles that are used to guide research around the world are respect for persons, concerns for welfare, and justice (described more fully in Table 1) [1].
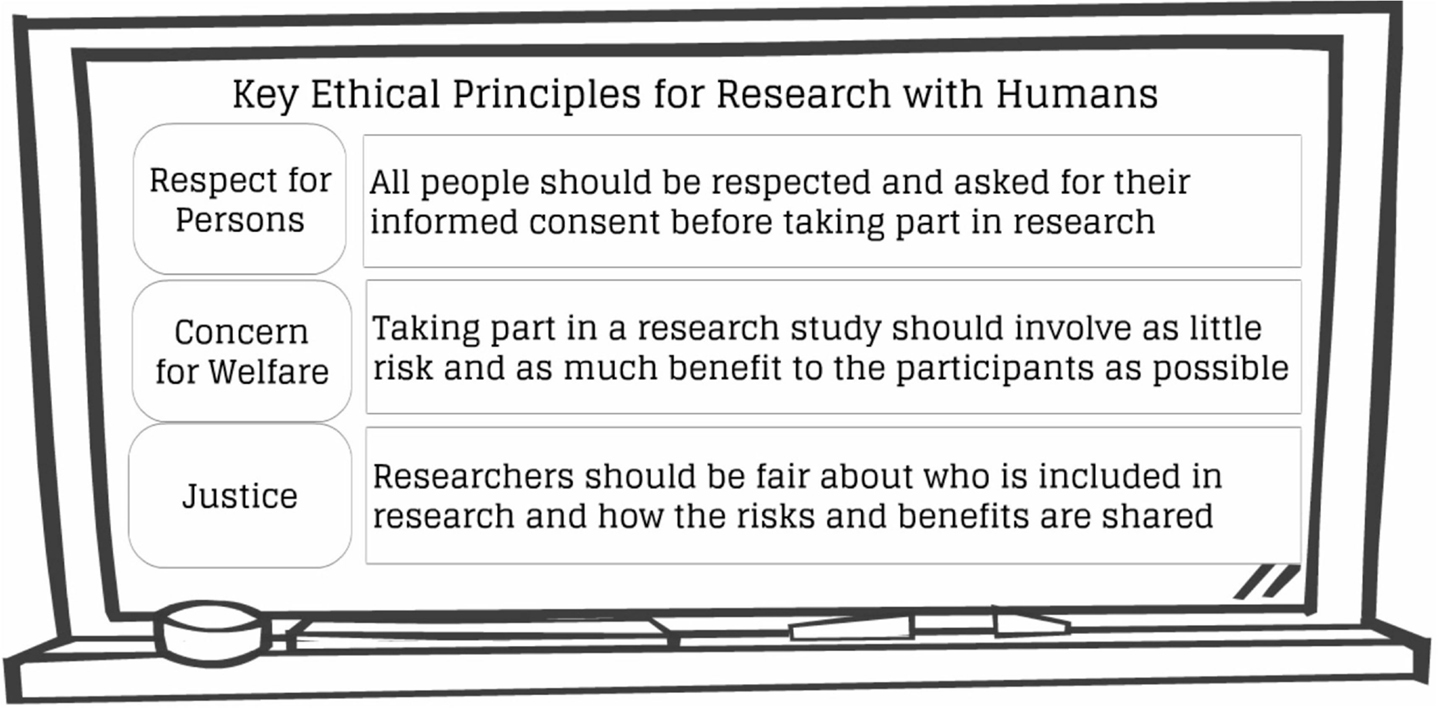
- Table 1
- Key ethical principles for research with humans.
Respect for Persons
Under the first principle, researchers must ensure that participants understand the goals of the research project and the process for data collection: what the research is for, what will be done to them, and what possible risks or benefits may be experienced during or after the study. Once all this information is provided, participants are then asked to provide informed consent. In order to respect a person’s autonomy – or their right to make decisions for themselves – it is important that research participants are aware of their rights and are free to join or leave a study without feeling under pressure.
If a person thinks they do not have a choice about participating in a research study or fear that there will be negative consequences if they refuse to take part, they might feel pressured. This can be an issue for children and youth, in particular, because they are naturally dependent on the adults around them for shelter, food, and education. Think about how you would react if your teacher or doctor asked you to take part in a study. This imbalance of power might make you feel like you have to participate, because they have authority over you.
Moreover, young children may not be able to fully understand what the research is about or what will happen to them if they participate. That is why a parent or guardian is usually asked to give informed consent on behalf of a child or young person. It is assumed that parents or guardians should act in the best interests of their child. Most studies involving youth include the additional step of informed assent. This involves telling young people (if they are old enough) about the study and asking if they would be willing to participate. If the young person and their parent or guardian both say yes, then the young person can take part.
Concern for Welfare
Under the second principle, researchers must ensure that their studies do not lead to excessive risk or harm for the participants. This is especially true for younger children, because they are often unable to express their needs or defend their interests. Young participants are also more likely to experience long-lasting benefits or potential harm to their development or education. Research on children that involves high-risk procedures, such as surgery, can only be carried out if the research is intended to provide a diagnosis or medical treatment and therefore benefit the child. Conducting research that involves risk but no benefit to children is considered unethical.
Justice
The third principle states that particular groups of people should not be unfairly targeted by or excluded from research. This could include young people, people of a minority group, or people with disabilities. In the past, children were often excluded from research in order to protect them, due to fears of unforeseen negative consequences. However, the more we learn about the unique needs and physiology of children, the more research involving children is recognized as essential, and ethical, to discover medications specifically for children.
To ensure that research is conducted in an ethical manner, researchers are required to submit a detailed description of their research project to a group of specialists known collectively as the “Research Ethics Board” (or REB). Members of the REB can prevent a research study from taking place if they believe that any of the ethics principles outlined above are not being followed. Because of this kind of ethical oversight, many more research studies are now being conducted with children and researchers can feel confident that they are doing so in the safest possible manner.
Neuroethics
Neuroethics is a field of study dedicated to understanding the ethical, legal, and social impact of research on and about the brain (i.e., neuro). Neuroethics also aims to better understand the brain processes that are involved in making decisions about what is right or wrong. Ultimately, research in neuroethics seeks to identify solutions to help neuroscience and society come together safely and with the best results.
Research in neuroethics breaks down into four main areas of study, described in Table 2 below. To provide a better understanding of each of these areas, we highlight four examples of neuroethics research from each of the four categories.
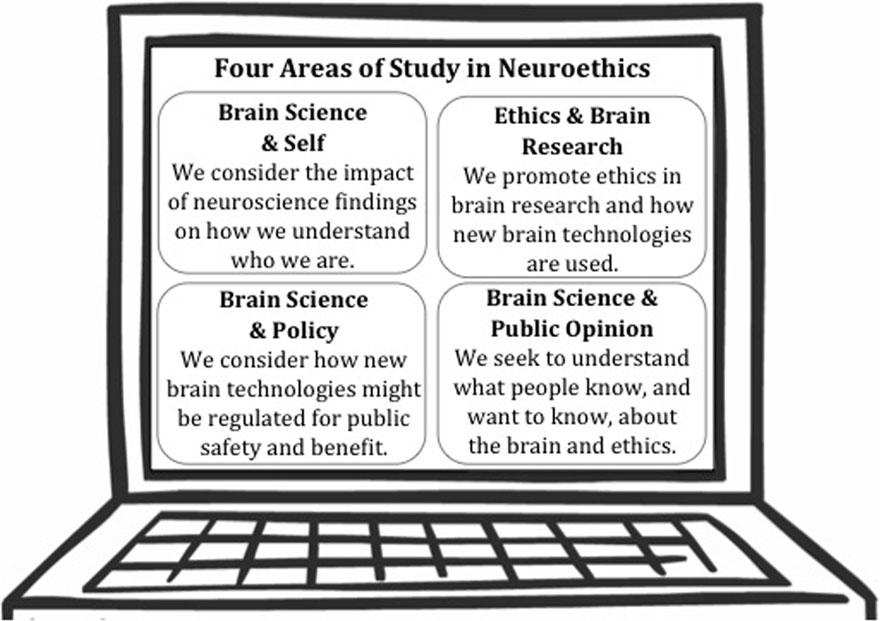
- Table 2
- Four areas of study in neuroethics.
1. Brain Science and Self
Research highlight: cognitive enhancement
The term cognitive enhancement refers to the improvement of thinking skills when there is not an inherent problem with thinking. Several medications have been created to help people with thinking problems improve their ability to concentrate and do better in school. Sometimes, however, healthy people also use these medications because they want to improve their memory or ability to learn as well. This is called cognitive enhancement, and neuroethicists have raised four concerns related to this practice [2].
First, there are concerns about safety. Medications are often associated with unwanted side effects. For people with thinking problems, it may be worth the risk to become well again. For healthy people, however, taking this medication could expose them to unnecessary risk. A second concern is that even if a medicine could be safely used to improve the brain, it would be unfair to people who cannot afford to do it too. Third, there are concerns that if some people do it, others will feel pressure to take the medications too, just to keep up. Finally, neuroethicists consider the impact that cognitive enhancement might have on the worthiness of achievements, and whether the public will judge people who use cognitive enhancement unworthy of their success. Neuroethicists want to understand issues like this better, to find out what the public thinks and come up with strategies to help people to be safe.
2. Brain Science and Social Policy
Research highlight: clinical trials on antipsychotic medications for use in children
Clinical trials are used in medical research to determine if a medication can be used safely and effectively in patients. For this kind of research, a drug is compared to either a placebo (a “dummy pill” that has no active drug chemicals) or another similar drug to see if the drug works better.
As described earlier under the principle of justice, children have traditionally been excluded from participating in clinical trial research. Today, however, ethicists agree that the risks and benefits of research should be fairly shared by everyone. As a result, researchers have started testing medications to see if they work for children as well as for adults. This is especially important for drugs that affect the brain, as children and young people’s brains are still developing and might react differently to such medications.
Antipsychotic drugs include chemicals that affect how the brain works and are often prescribed for conditions such as mood or attention problems. Despite government policies to increase the number of clinical trials involving children, neuroethics research has shown that there are few high-quality studies to indicate whether antipsychotics are safe for children to use and whether they improve the lives of children with different developmental and psychiatric disorders [3]. More evidence is needed to help doctors and families make informed decisions about these drugs that are already being prescribed to children.
3. Ethics and Practice of Brain Science
Research highlight: incidental findings
Brain scans are often used in neuroscience research, because they cause little harm to the participants and provide useful images of the brain. Taking pictures of the brain, however, sometimes leads to unexpected findings. For example, when looking at the brain for one purpose, a researcher might notice an unusual growth in that person’s brain. Researchers refer to this as an incidental finding.
The example of a brain tumor is rare, however. Most often, the discovery of an incidental finding involves something minor (like a slightly enlarged ventricle in the brain) that does not pose any threat. In other cases, brain scan images might reveal something that looks a little odd but that has unclear significance. There has been much debate in the field of neuroethics about the roles and duties of researchers to notify participants about these incidental findings.
If the finding poses a significant threat to the health of the participant, like a brain tumor, neuroethicists agree that the participant should be told right away. However, if the incidental finding does not require medical care or is unclear, some have argued that the participant should be given the choice to be told about it or not. This is because being told that you might have something wrong can cause a person to worry, even though there might not be anything serious to worry about. With older youth, the decision to disclose a minor incidental finding is more complicated because both the parent and child must be involved in the decision. Some neuroethicists argue that if the young participant has the ability to understand the consequences of being told this kind of information, then they should be the one to decide [4].
4. Brain Science and Public Discourse
Research highlight: quality of online health information for neurodevelopmental disorders
After receiving a diagnosis from a doctor, most people look on the Internet for information about treatments, possible cures, or just to learn about the condition. Neuroethics researchers are interested in the quality and accuracy of online brain health information, because a lack of high-quality information could cause people to make bad decisions about health care.
For instance, neuroethics research on the quality of online information for common neurodevelopmental disorders (such as autism and cerebral palsy) has shown that the information is often of poor quality [5]. Most of the websites studied listed different treatments and indicated that they worked, even though there was little scientific evidence to support these claims. Some websites also had unscientific and inaccurate explanations of how autism is caused. Such results raise many ethical concerns, because families may use this misleading information to make treatment decisions. We encourage you to be critical of websites, and bring any questions to your doctor so that you can get the most benefit from information online.
Conclusion
We have highlighted only a small fraction of the issues being addressed in neuroethics research. Now that you know a bit about what neuroethics is concerned with today, we invite you to find out more on our website (neuroethicscanada.ca) and think about what is important to you and the future of ethics in Neuroscience.
References
[1] ↑ Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council of Canada. 2010. Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. Available at: http://www.pre.ethics.gc.ca/pdf/eng/tcps2/TCPS_2_FINAL_Web.pdf
[2] ↑ Fitz, N. S., Nadler, R., Manogaran, P., Chong, E. W., and Reiner, P. B. 2013. Public attitudes toward cognitive enhancement. Neuroethics. 7(2):173–88.
[3] ↑ Mc Glanaghy, E., Di Pietro, N. C., and Wilfond, B. 2015. Pediatric clinical trial activity for antipsychotics and the sharing of results – a complex ethical landscape. In The Science and Ethics of Antipsychotic Use in Children. eds. N. C. Di Pietro and J. Illes, Academic Press.
[4] ↑ Di Pietro, N. C., and Illes, J. 2013. Disclosing incidental findings in brain research: the rights of minors in decision-making. J. Magn. Reson. Imaging 38(5):1009–13. doi: 10.1002/jmri.24230
[5] ↑ Di Pietro, N. C., Whiteley, L., and Illes, J. 2012. Treatments and services for neurodevelopmental disorders on advocacy websites: information or evaluation? Neuroethics 5:197–209. doi: 10.1007/s12152-011-9102-z