Abstract
Everyone catches the flu or a cold from time to time. We designed an experiment to study how being sick more often affects the brain. To do this, we used a piece of a bacteria to make adult male mice experience symptoms of sickness. We gave mice this substance five total times. Mice got better in a few days and had 2-week breaks between exposures. We then measured how the mice learned and remembered new information, and how well their brain cells were working to help them learn. Our experiments indicate that being sick often interferes with communication between brain cells, causing mice to have trouble learning and remembering. Our data can help doctors predict which patients may have memory problems as they grow older. Our study also shows the importance of staying as healthy as possible and taking steps to protect ourselves and others when we do get sick.
Infections and the Brain
The itch in the throat, the sniffly nose, the upset stomach, the throbbing head, the chills… we all know the feeling of catching a cold or the flu. It is not fun. Being sick not only affects the way the body works—it also affects the brain. Being tired, having trouble concentrating, and feeling unmotivated, withdrawn, or grumpy are a few of the common, mild, brain-affecting symptoms people experience while feeling sick [1, 2]. Luckily, most people feel unwell for only a few days. As the immune system fights off the infection, people usually feel better and can return to normal activities, like going to school or seeing friends.
Getting sick is a common experience in life, yet some people get sick more often than others. Studies in humans suggest that elderly people who have had more infections across their lifetimes show a greater decline in brain abilities known as cognitive functions [3, 4]. This could pose a problem for people facing memory changes as they get older, a common problem in this group.
Our research question was: “What happens to the brain and how it works if a person has more experiences with infections?”. We hypothesized that, if more experiences with infection negatively affect the brain, we would see problems with the way brain cells (called neurons) communicate and with the way information is learned and remembered.
How Did We Make Animals Sick?
It is not ethical to do experiments in which we make people sick on purpose. So, we used adult male mice [5]. Mice are commonly used in biological experiments and they age very quickly, allowing us to easily study changes across time. All of our procedures were reviewed and approved in advance by a panel of other scientists, to ensure the welfare of our mice. We selected procedures that would minimize any pain or distress the mice might experience. Additionally, all experimenters were trained in the ethical use of animals in research.
We made some mice in our study “sick” by giving them an injection of a substance called lipopolysaccharide (LPS). LPS comes from the outer layer of a certain type of bacteria. Many scientists have used LPS to learn about how both bacterial infections and the immune system work [6]. When we give a moderate amount of LPS to mice, it triggers the immune system to produce temporary inflammation, just like what would happen if the mice were infected by actual bacteria. Importantly, because LPS is only a part of the bacteria, the infection cannot spread from cell to cell within an animal or from animal to animal.
We gave some of the mice LPS five times over about 3 months (Figure 1A). We waited 2 weeks between “infections” with LPS before making mice “sick” again. Each time these mice were given LPS, other mice were given a control substance, which should have very little effect on the body on its own. In our case, this control was saline (salt water), like what you would get at the hospital if you were dehydrated. Our control group contained normal mice that had never experienced infections. We compared how the brains of control group mice worked to the brains of mice that experienced several LPS exposures. After the mice recovered from all five injections, we measured their learning and memory, as well as how their neurons communicated.
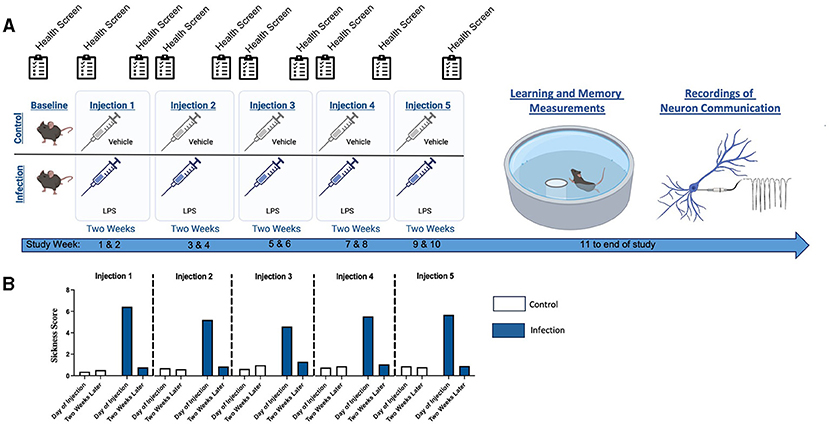
- Figure 1 - (A) We gave mice saline control or LPS every 2 weeks.
- We measured how sick mice looked and behaved right after each LPS injection and just before the next. After five injections, mice were tested for learning and memory using the Morris water maze. Communication of hippocampus neurons was also studied from mice in both groups. (B) The higher the score on our scale, the more sickness behavior mice showed. We found that each exposure to LPS made mice moderately but briefly “sick”. Within 2 weeks, the sick mice made a full recovery. Control mice never showed signs of sickness. Average values are shown.
“Infected” Mice Got Moderately Sick For a Short Time
First, we measured how “sick” the mice were at several time points during the study. We used a health screening we developed that is similar to a physical exam a doctor might complete when you are sick. We looked at the appearance, posture, breathing rate, and movements of the mice. We also checked to see if they had lost any weight and took their temperatures to see if they had a fever. Each item we measured was assigned points and the more points an animal had, the sicker it behaved (Figure 1B). We did these measurements the same day as the injections. Two weeks later, we also measured all these characteristics again, to make sure the mice were not still sick before the next LPS injection was given.
No mice showed signs of sickness before injections began. As we expected, we generally did not see any signs of sickness in mice that were given the saline control. But each time the mice were given LPS, they showed moderate sickness behaviors. The sickness behaviors did not last long. Just before the next exposure, all LPS-treated mice had sickness scores similar to control mice, meaning that they had recovered from the effects of LPS. These data meant that we could test our hypothesis about the effects of multiple infections on the brain!
Experiencing Sickness Several Times Impairs Memory and Learning
We next measured how our mice learned and remembered (Figure 1A). Since mice cannot use words to tell us what they know, we did this using a water maze. Mice are natural swimmers. Dr. Richard Morris created this test about 40 years ago. Mice were placed in a large tub of room-temperature water (Figure 2). The water was dyed to hide an exit platform just below the surface. Mice swam around the maze looking for the platform so that they could get out of the water and go to a warm cage to dry off. The room with the maze in it contained landmarks (for example: images of different geometric shapes) that helped the mice navigate. Mice swam from the starting point to the hidden exit platform, the location of which stayed the same for the entire experiment. Once they found the hidden platform, the experimenter took the mouse back to their warm cage to dry off. As they learned the location of the exit platform over several trials, the mice swam in a more efficient path to the platform, which took less distance. Swim distance was our dependent variable. This behavior is very similar to how a person learns the route from various places in town (school, the mall, or a restaurant) back to their home. To make sure mice stayed safe while swimming, there was always a “lifeguard” scientist on duty. All mice were given six swims each day for 8 days, for a total of 48 swims in the maze.
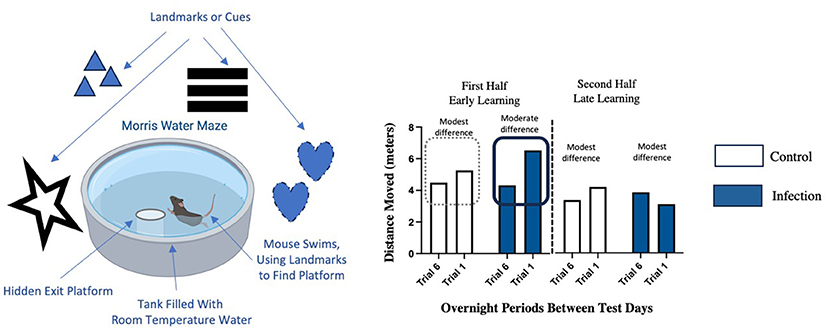
- Figure 2 - We measured how well mice learned and remembered using the Morris water maze.
- Mice that previously experienced several LPS exposures had difficulty remembering the location of the platform between test days during the first half of training (early learning phase). A larger difference means more forgetting of the platform location between test days. There were no differences in remembering in the second half of testing (late learning phase) for either group of mice.
Before the start of this memory test, all mice showed similarly good health scores. However, we found subtle differences in how the mice remembered the things we taught them (Figure 2). To determine how well mice remembered information that they learned each day, we compared the distance the mice swam to the exit platform on the last trial of each day (Trial 6) to the swim distance in the first trial the next day (Trial 1). Mice that were given control injections were mostly able to remember the exit platform location between test days. We know this because mice in this group show similar distances on Trial 6 and Trial 1 for those test days. However, the mice that repeatedly experienced and recovered from LPS “infections” had more trouble remembering this information between test days. We know this because these mice swam further on the first trial of each day (Trial 1) compared to the last trial the day before (Trial 6). This is a bit like how you might forget the details of the route to a friend’s house if some time has passed since you last visited, causing you to make a few wrong turns along the way. Fortunately, this memory problem was brief and went away during the second half of the testing period as mice had more swims and learned the location of the hidden platform better. This suggests that mice with a history of LPS “infections” have a little bit more trouble remembering information as they are first learning it but, with additional practice to reinforce what they learned, they can catch up to mice that had not experienced repeated sickness.
Experiencing Sickness Several Times Changes Neuron Communication
Next, we studied how experience with infections affected neurons in a part of the brain called the hippocampus, which is important for learning and memory (Figure 3). Neurons in the hippocampus control how we learn and remember things by communicating with each other. Neurons communicate very quickly, on the scale of milliseconds (1 millisecond equals 0.001 s). When neurons function properly, we can learn and remember things well.
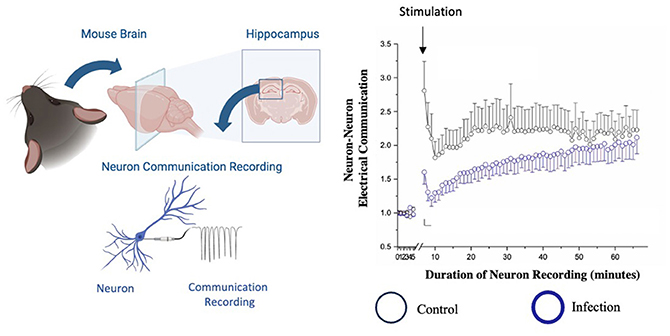
- Figure 3 - We measured how neurons communication in the hippocampus by recording electrical signals.
- Before stimulation (1–5 min), neurons from both groups had similar electrical signals. We then stimulated a neighboring neuron and measured the electrical signals produced by the receiving neuron. Neurons from mice that experienced several LPS exposures showed reduced communication at early timepoints. The dots represent the average signal. Not all neurons receive or produce the same signal, so the range of communication is indicated by the bars around the dots.
Neurons receive information from some of their neighboring neurons and send messages to others using electrical signals. Scientists can understand how well neurons are communicating by using special tools to measure these electrical communications. First, we looked at the signals from a neuron in the hippocampus to determine its normal level of electrical activity. Then, we stimulated another neuron, one that communicates with the hippocampus neuron we were interested in, and measured how well that communication signal was received by the hippocampus neuron by measuring its electrical activity in response. We expected that neurons would increase their electrical activity as they received signals from the neighbor neuron that we stimulated. We did this for neurons from mice exposed to several LPS injections as well as for neurons from mice given control injections. We recorded neuron signals for 1 h.
Neurons from mice that experienced repeated LPS or control injections could receive the signals from their neighboring neurons. Both groups also showed more communication following the stimulation, as we expected. Interestingly, the electrical signals of neurons from control-treated mice were stronger than those of neurons from mice that had experienced LPS, especially early in the recording period (Figure 3). This means that in mice with a history of recurrent LPS exposure, hippocampus neurons were less able to receive the communication signals from other neurons compared to control mice. This impairment appears to recover during the hour-long recording period, however the early disruption of communication still negatively impacts learning. Imagine you are in class, listening to your teacher explain an assignment. If you only receive a portion of the instructions the teacher is giving, you will have more trouble doing the assignment correctly and earning a good grade. Overall, being sick frequently can negatively impact learning and memory, as we saw in our water maze.
What Did We Learn Overall?
Infections are a normal part of life. They happen to nearly all people and animals. However, infections can happen to some organisms more than others. We learned that some of the neurons in the hippocampi of mice that had several recurrent LPS experiences did not communicate as well as they normally would. This corresponded to slight difficulties with remembering information the mice were learning, at least at first. These learning and memory effects happened a while after the last LPS treatment, when the mice were healthy and showed no signs of sickness behavior.
This information is helpful because it gives scientists and doctors important knowledge about how infections may affect people in the long run. This is especially important for older people whose cognitive functions might be declining as they age. Our data could reveal new ways to reduce the brain and memory changes that tend to happen as people age. For example, maybe researchers will discover new ways to treat infections that help to avoid these learning and memory problems.
Our study has some limitations. First, we only used male mice, so our future work will include female mice. Secondly, LPS is a model of bacterial infections, but other microbes, such as viruses, fungi, and parasites, can also infect people and impact how the brain works. We have recently completed an experiment using viral infections to learn how other microbes affect the brain [7]. Finally, we must test potential ways to prevent the brain and behavior effects that come with a greater number of infections.
A key take-away from this work is that minimizing infections may protect our brains and maintain how well we think and remember as we age (Figure 4). Staying healthy, for example by getting annual flu vaccines, can reduce our chances of getting serious infections. We can also limit the spread of infection to family and friends by practicing good hygiene such as proper handwashing. If we are sick, we can use social distancing and wear masks in crowded indoor areas like grocery stores or classrooms. In summary, experiencing occasional infections is a normal part of life for nearly everyone, but staying as healthy as possible could keep our brains functioning at their best as we grow older.
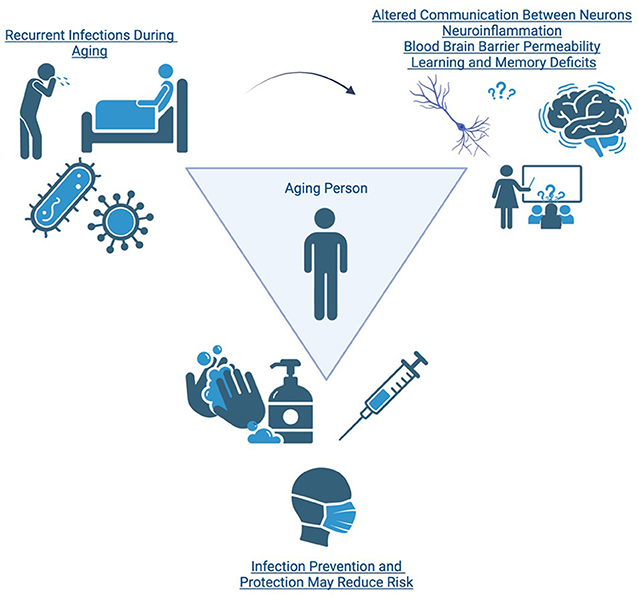
- Figure 4 - This schema summarizes the findings and implications of our study.
- Getting sick occasionally is normal but some people get sick more often than others (top left). This can result in detrimental effects for our brain and the way we learn and remember (top right). We need to understand what kinds of effects those might be, who might be at most risk for these consequences, and what we can do about it. We can reduce our risk of infection by practicing good hygiene (like washing our hands), by getting our yearly flu vaccines, and by social distancing or masking (bottom middle).
Glossary
Immune System: ↑ The group of organs and cells that controls how we respond to infections or injuries.
Cognitive Function: ↑ Mental processes, including thinking, knowing, remembering, judging, problem-solving, and decision-making, that enable us to understand and interact with the world.
Neurons: ↑ Cells in the brain that receive information from the body or other parts of the brain, communicate with each other through electrical and chemical signals, and control our thoughts, feelings, and responses.
Lipopolysaccharide (LPS): ↑ A fragment of the cell wall from a type of bacteria. It can trigger strong immune responses and is often used in research to study inflammation.
Control: ↑ A group in a study that are considered normal. Scientists compare values on a dependent variable in the control group to any changes in this variable that are observed in the experimental group.
Dependent Variable: ↑ A variable that is used to determine the effects of experimental manipulations because it changes under different conditions.
Hippocampus: ↑ A small, curved region in the brain crucial for memory formation and spatial navigation, helping us remember information and understand our physical location.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by: K01MH117343, U54GM104942, P20GM109098, P20GM103629, T32AG052375, R01AG082899, and pilot grants from the Infectious Disease Society of America (IDSA) and the Tulane Brain Institute. We acknowledge the support of the West Virginia University Rodent Behavior Core. The figures are reproduced with permission from Engler-Chiurazzi EB, Russell AE, Povroznik JM, McDonald KO, Porter KN, Wang DS, Hammock J, Billig BK, Felton CC, Yilmaz A, Schreurs BG, O’Callaghan JD, Zwezdaryk KJ, Simpkins JW. Intermittent systemic exposure to lipopolysaccharide-induced inflammation disrupts hippocampal long-term potentiation and impairs cognition in aging male mice. Brain Behav Immun. 2023 Feb;108:279–291. doi: 10.1016/j.bbi.2022.12.013. Epub 2022 Dec 19. PMID: 36549577; PMCID: PMC10019559.
Original Source Article
↑Engler-Chiurazzi, E. B., Russell, A. E., Povroznik, J. M., McDonald, K. O., Porter, K. N., Wang, D. S., et al. 2023. Intermittent systemic exposure to lipopolysaccharide-induced inflammation disrupts hippocampal long-term potentiation and impairs cognition in aging male mice. Brain Behav. Immun. 108:279–91. doi: 10.1016/j.bbi.2022.12.013
References
[1] ↑ Batista, C. R. A., Gomes, G. F., Candelario-Jalil, E., Fiebich, B. L., and de Oliveira, A. C. P. 2019. Lipopolysaccharide-induced neuroinflammation as a bridge to understand neurodegeneration. Int. J. Mol. Sci. 20:92293. doi: 10.3390/ijms20092293
[2] ↑ Harris, S. A., and Harris, E. A. 2015. Herpes simplex virus type 1 and other pathogens are key causative factors in sporadic Alzheimer’s disease. J. Alzheimer’s Dis. 48:319–53. doi: 10.3233/JAD-142853
[3] ↑ Katan, M., Moon, Y. P., Paik, M. C., Sacco, R. L., Wright, C. B., and Elkind, M. S. 2013. Infectious burden and cognitive function: the Northern Manhattan Study. Neurology 80:1209–15. doi: 10.1212/WNL.0b013e3182896e79
[4] ↑ Strandberg, T. E., Pitkala, K. H., Linnavuori, K., and Tilvis, R. S. 2004. Cognitive impairment and infectious burden in the elderly. Arch. Gerontol. Geriatr. Suppl. 9:419–23. doi: 10.1016/j.archger.2004.04.053
[5] ↑ Engler-Chiurazzi, E. B., Russell, A. E., Povroznik, J. M., McDonald, K. O., Porter, K. N., Wang, D. S., et al. 2023. Simpkins: intermittent systemic exposure to lipopolysaccharide-induced inflammation disrupts hippocampal long-term potentiation and impairs cognition in aging male mice. Brain Behav. Immun. 108:279–91. doi: 10.1016/j.bbi.2022.12.013
[6] ↑ Catorce, M. N., and Gevorkian, G. 2016. LPS-induced murine neuroinflammation model: main features and suitability for pre-clinical assessment of nutraceuticals. Curr. Neuropharmacol. 14:155–64. doi: 10.2174/1570159x14666151204122017
[7] ↑ Harrison, M. A. A., Morris, S. L., Rudman, G. A., Rittenhouse, D. J., Monk, C. H., Sakamuri, S. S. V. P., et al. 2024. Intermittent cytomegalovirus infection alters neurobiological metabolism and induces cognitive deficits in mice. Brain Behav. Immun. 117:36–50. doi: 10.1016/j.bbi.2023.12.033