Abstract
AIDS (acquired immune deficiency syndrome) is the name used to describe a number of potentially life-threatening infections and illnesses that happen when the immune system has been severely damaged by the human immunodeficiency virus (HIV). HIV/AIDS is considered a pandemic, affecting almost 38 million people throughout the world in 2020 alone. There is no cure for this disease and no vaccine to prevent it. Although people can not be cured, they can live for years with appropriate treatment. In addition to the difficulty of living with a chronic and aggressive disease, people living with HIV/AIDS also suffer frequently from many forms of social stigma and discriminations. In this article, I will tell you about AIDS, the discovery of its viral cause, current available treatments, and future possibilities for decreasing the number of people living with HIV/AIDS. I hope that, by the end of this article, you will understand the global importance of dealing with HIV/AIDS—both scientifically and socially.
Professor Françoise Barré-Sinoussi won the Nobel Prize in Physiology or Medicine in 2008 (jointly with Luc Montagnier) for the discovery of human immunodeficiency virus (HIV).
What is HIV/AIDS?
HIV (human immunodeficiency virus) is a virus that attacks the cells that help the body fight infection, making a person more vulnerable to other infections and diseases. It specifically targets a type of white blood cell called CD4 cells (Figure 1) [1]. CD4 cells are “helper” cells—they help the immune system by activating other immune cells when a foreign invader, like a virus, enters the body.
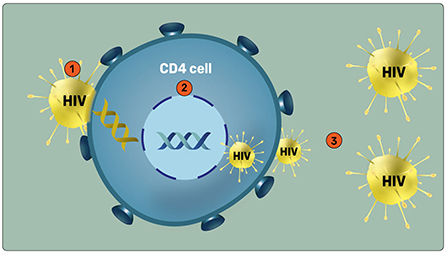
- Figure 1 - Infection by HIV.
- (1) HIV attaches to a CD4 immune cell before entering it. (2) Viral genetic material (yellow spiral) combines with the DNA of the CD4 cell (blue), and takes over the reproduction system of the cell so that the virus makes additional copies of itself. (3) New HIV particles leave the CD4 cell and go into the blood to infect additional CD4 cells. In this way, HIV continues to multiply and spread throughout the body. Over time, CD4 cells are killed by HIV and the body’s ability to recognize and fight various infections declines.
The human body cannot get rid of HIV by itself and no effective cure for HIV exists presently. Once someone has HIV, they have it for life. If it is left untreated, the body’s immune system becomes so badly damaged that any infections, such as pneumonia, are much more dangerous and life-threatening [2].
The first cases of AIDS were reported in the early 1980s [2] and, soon after, it was declared a global pandemic. It is currently believed that the HIV infection in humans originated from contact with non-human primates (such as chimpanzees and gorillas) in Africa—this is referred to as cross-species transmission [3]. According to the World Health Organization1, almost 80 million people have been infected with HIV since the beginning of the pandemic, and about 45% of them have died2. In 2020, 37.7 million people were living with HIV, 1.5 million people were newly infected with HIV, and 680,000 people died of illnesses related to HIV.
AIDS is found throughout the world, with about two-thirds (69%) of the cases in Africa, about 15.5% in Asia and the Pacific, about 6% in North America and in Central Europe, about 5.5% in Latin America, and about 4% in Eastern Europe and Central Asia (Figure 2).
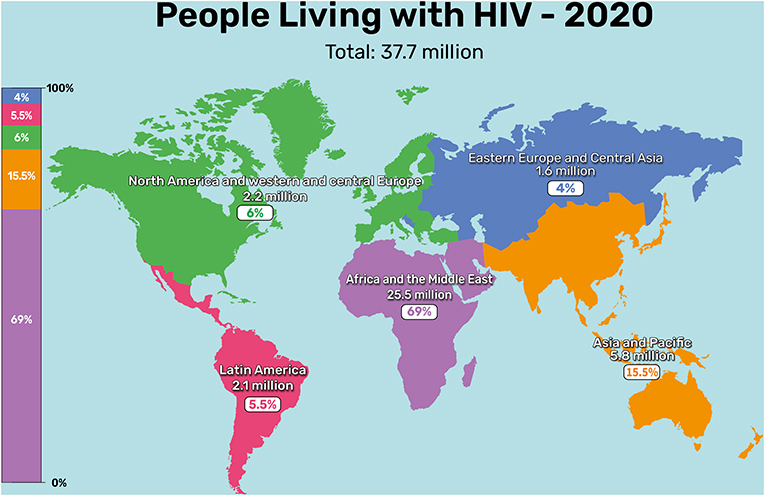
- Figure 2 - Worldwide distribution of HIV in 2020.
- (Image adapted from: UNAIDS 2021 epidemiological estimates).
How is HIV Spread and What are Its Symptoms?
There are three ways to become infected with HIV: unprotected sexual activity, direct contact with infected blood (for example, through blood transfusions), and transmission from infected mothers to their babies [5]. After HIV is contracted, there are three stages to the disease (Figure 3). The first stage is called acute HIV, which starts after the initial infection and lasts until the body makes an immune response and begins to produce HIV-specific antibodies. At this stage, HIV viruses are seen in the blood [6] and the virus reproduces rapidly, spreading throughout the body. Some people develop flu-like symptoms in the acute stage, such as fever, sore throat, muscle aches, diarrhea, rash, and fatigue. These symptoms usually appear about two to four weeks after the initial infection.
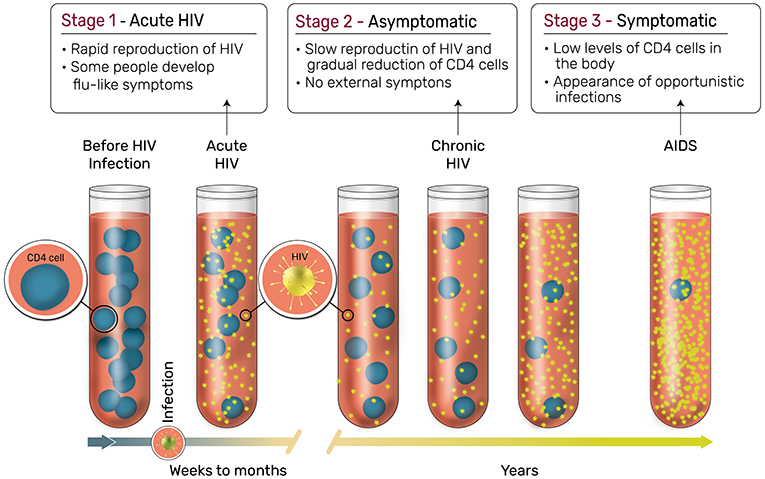
- Figure 3 - Stages of HIV infection.
- If we take blood from patients at the three stages of the disease, we find that in the first stage of the disease (Acute HIV), occurring in the first couple of weeks or months after the infection, the HIV virus spreads quickly. Some, but not all, patients develop flu-like symptoms in this stage. In the second stage (Asymptomatic), which could last for many years, the virus spreads slowly and patients show no symptoms. In the third and final stage (Symptomatic), patients are left with low levels of CD4 cells and show severe symptoms (Image adapted from: https://hivinfo.nih.gov/understanding-hiv/fact-sheets/stages-hiv-infection).
The second stage of an HIV infection is called chronic HIV. At this stage, the virus is still active, however, it is not producing any visible symptoms. Therefore, this stage is also called an asymptomatic (without symptoms) infection. If not treated, the asymptomatic stage can last for years before the third, symptomatic, stage of the disease develops. Although people can not be cured, they can live in the asymptomatic stage for years with appropriate treatment. If not treated, people living with HIV can pass on the virus even though they show no symptoms of the HIV infection. The final and most severe stage of HIV infection is called acquired immunodeficiency syndrome, or AIDS. People are diagnosed with AIDS when their numbers of CD4 cells drop to very low levels, or if they develop other infections that are related to AIDS, which are called opportunistic infections. Opportunistic infections take advantage of the weakened immune system and may eventually cause death if they are left untreated.
HIV/AIDS and Stigma
In the beginning of the 1980s, early studies found that AIDS was especially prevalent among people who used drugs people who received blood transfusions, and men who had sexual contact with men [3]. The stigma of having HIV/AIDS has become widespread and deeply rooted within societies all over the world. This means that people living with HIV are sometimes made to feel ashamed by the societies they live in, so they do not seek out the medical treatment they need. Negative attitudes and false beliefs about HIV and people living with HIV often lead to discrimination and can seriously impact the mental health and wellbeing of these individuals [7, 8].
In addition to the negative psychological effects of the stigma faced by people living with HIV/AIDS, such stigma also reduces the effectiveness of prevention and treatment strategies [9] that could otherwise slow down the spread of the disease. For example, due to HIV/AIDS stigma and discrimination, people living with HIV are less likely to tell their sexual partners about their HIV status and are more likely to take part in unsafe sexual activity3, both of which increase the chances of HIV transmission [9]. Additionally, some people living with HIV/AIDS hesitate to get treatments, since they are afraid of being stigmatized when others know that they are being treated [9]. Furthermore, stigma can lead to a lack of support networks for people living with HIV/AIDS [8]. For more information on young people and HIV, see this Frontiers for Young Minds article [10].
These are only a few of the many examples of how HIV/AIDS related stigma can negatively affect people living with HIV/AIDS—and all of society. I believe that it is very important to address stigma by providing accurate information to people like you—the younger generation—who are the future of society. Diminishing stigma associated with HIV/AIDS, along with scientific and medical advances in HIV/AIDS prevention and treatments, can help us to achieve the goal of an AIDS-free generation [11].
The Discovery of HIV
I will now outline the discovery of HIV, for which I received a Nobel Prize in Physiology or Medicine in 2008, with Luc Montagnier. In my Ph.D. studies, I worked on the relationship between cancer and a family of viruses called retroviruses. Retroviruses are particularly nasty viruses that cause serious illnesses. They have RNA as genetic material that must be transformed in DNA by a special enzyme of the virus, named reverse transcriptase. This transformation allows the integration of the genetic material of the retrovirus into the DNA of host cells that then reproduce viral RNA and viral proteins, resulting in the release of new retroviral particles capable to infect other healthy cells.
When AIDS appeared in 1981, most researchers were looking for viruses that could be responsible for it, but they were not having much luck. One group of doctors in France, who knew that we were experts in the study of retroviruses, came to our laboratory at the Institut Pasteur in Paris. They asked us a very simple question—did we think that a retrovirus, rather than a regular virus, could be responsible for AIDS?
Their own hypothesis was that the only known human retrovirus at that time, the human leukemia T-cell virus (HTLV), could be the cause of AIDS. However, we thought that this hypothesis was incorrect because HTLV is a virus that causes a type of blood cancer called leukemia, where cells become immortal, replicate themselves and spread quickly in the body. In contrast, physicians found in their clinical observations that AIDS patients lost their white blood cells—meaning that, unlike in leukemia, in HIV/AIDS the cells die and reproduce less than normal. Therefore, HTLV was unlikely the virus that caused AIDS.
We wondered whether we should look for a different retrovirus that could cause the disease, and this is how the story began. Knowing that HIV attacks the CD4 immune cells, we looked for a retrovirus virus in these cells. By then, I already knew how to detect retroviruses produced by cells, by looking for a reverse transcriptase activity, the retroviral enzyme used to generate DNA from viral RNA. If this enzyme is present in cell supernatants, it suggests that cells are producing retroviruses. In January 1983, after few days of culturing T cells from a lymph node biopsy of a patient with pre-AIDS syndrome, we eventually detected a reverse transcriptase activity in the culture. Later, on retroviral particles were observed by electron microscopy which turned out to be a novel retrovirus later named HIV (which was called lymphadenopathy-associated virus, or LAV, at that time) [12].
This success story demonstrates why discussion and interaction between researchers and physicians is crucial. In our case, based on the physicians’ observations, we could together identify an efficient strategy to search for the virus. Contact with physicians was important at all stages—from identifying the symptoms of the disease, its cause, its method of attack, and the development of the best possible prevention strategies and treatments.
Treating HIV/AIDS—Current and Future Directions
Now, in 2022, there is still no cure for HIV/AIDS, and there is also no vaccine that prevents HIV infection. Therefore, people living with HIV are chronic carriers of the virus and they need to take medications every day of their lives. The medical treatment for HIV is called antiretroviral therapy (ART), which consists of a mix of chemicals that limits the ability of HIV to reproduce, therefore maintaining low amounts of the virus in the body4. When relatively small amounts of HIV are present in the body, the immune system can recover from the damage to CD4 cells that the virus causes. The lifespan of infected people on ART is similar to that of non-infected people, especially if they are treated early after infection. In addition, infected people on ART with no detectable virus do not transmit the virus to others. Indeed, ART can also be used as pre-exposure prophylaxis to efficiently prevent HIV infection in people at risk for HIV infection. Also, reducing the amount of HIV in the body reduces the risk of transmission of the virus to other people, when the virus is not detected in the blood it cannot be transmitted. Additionally, it prevents infected people from contracting other harmful infections that might lead to death.
ART therapies have contributed to the significant decrease in AIDS-related deaths, though the numbers are still high. It is believed that these high numbers result mainly from delayed diagnosis of HIV infections (i.e., when the infection is diagnosed the immunological system is already severely damaged), limited access to the therapies (especially in developing countries), refusal of some HIV-infected subjects to receive ART therapies, and low adherence to these treatments (i.e., patients not following the medical advice) [13, 14]. Additionally, lifelong ART therapy has several limitations such as the possibility of developing drug resistance (meaning the therapy becomes less effective with time), side effects that can accumulate with time, and a high cost that places an impossible financial burden on patients with limited resources [15].
Apart from the ART therapies that are used worldwide, there are other new treatments that have great potential to become cures in the future. One promising direction is called stem-cell transplant, in which stem cells are injected into the patient’s body to help re-grow their immune cells5. I believe that we still need more scientific research to develop a reliable and widely applicable cure for HIV/AIDS, and to develop vaccines that will help prevent HIV infections [16]. It is important to note that, while concentrating our efforts on scientific solutions is important, we must also try to make wider changes [7]. By providing reliable information to individuals living with HIV/AIDS and educating all of society about the virus, we will succeed in reducing further its prevalence and mortality worldwide.
Recommendation for Young Minds
It seems to me that, in today’s world, people are too self-centered. My main recommendation for you, the younger generation, is to think about what is most important in life—is it yourselves, or is it helping others? In my opinion, the most important thing in life is to give to others, no matter what field you are in, and to help in whatever way possible. From my experience, if you give to others, you will receive back from others—and that will lead to a happy life. Otherwise, if your life is only for yourself, I believe you will never be entirely happy.
I would also like to share my perspective on challenges. What I have enjoyed most in my scientific career are the challenges that I have faced. Challenges always cause you to question yourself. In research, you can never be certain about the validity of the data you obtain, so you must try to verify your data and replicate it, making sure that you obtain the same results again and again. Additionally, if you obtain results that you were not expecting, you might need to change your research strategy, and sometimes also change your hypothesis. I think that science is like a game with yourself, where you repeatedly challenge yourself and change your ideas. If you choose the scientific path, I recommend that you learn to appreciate the unexpected, since it is a natural part of the process of scientific discovery. Additionally, for anyone who may be interested in the life sciences and clinical research, I would emphasize that it is very important to be in contact with both physicians and people affected by the disease, so that you remain in touch with real-world challenges, as well as with the research work in the laboratory. This was certainly a determining factor in my career working on HIV/AIDS.
Last, for all future women scientists, I will end on an optimistic note. When I started my career in the 1970s, it was much harder for women scientists than it is today. As a female student, I was told that I had no chance of getting a research position at the Institut Pasteur. Eventually, I did get a position at the National Institute of Health and Medical Research (INSERM) and worked at the Institut Pasteur for about 40 years, until I retired a few years ago. Today, there are about 50 women professors at the Institut Pasteur, compared to only about 5 when I joined. So, you can see that a lot of progress has been made in the last 50 years. Nonetheless, there is still much to do to further advance women in science. As female scientists, we should be particularly supportive of each other and work together toward the goal of complete equality in science. I believe we will keep seeing positive changes in that direction in the coming years.
Additional Materials
- Global HIV Statistics—World AIDS Day 2021 (UNAIDS).
- Why Is It Difficult for Young People With HIV to Share Their Diagnosis? Frontiers for Young Minds (frontiersin.org).
- How the Innate Immune System Fights for Your Health.
- Flu, Flu Vaccines, and Why We Need to Do Better.
Glossary
Immune System: ↑ A system in the body that protects it from organisms that cause disease, such as bacteria and viruses.
Pandemic: ↑ A pandemic is said to occur when a disease spreads over more than one continent and affects a very large number of people.
Opportunistic Infections: ↑ These are infections that “take advantage” of the weakened immune system of people infected with HIV virus. These infections are usually the cause of mortality of people having AIDS.
Discrimination: ↑ Treating people unfairly due to their belonging to different groups or categories from the majority.
Retrovirus: ↑ A virus that produces a DNA copy from its RNA, and inserts it into the DNA of a host cell. This is the reverse of the usual genetic pattern, where RNA is produced from DNA; thus retro (backwards).
Reverse Transcriptase: ↑ An enzyme used by retroviruses to generate DNA from RNA. Measurements of reverse transcriptase in cells are used to check whether cells are infected with a retrovirus.
Antiretroviral Therapy: ↑ A medical treatment for HIV, consisting of chemicals that limit the ability of HIV to reproduce.
Stem Cells: ↑ Immature cells that can become most other cell types, like muscle cells, brain cells, liver cells, etc.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I wish to thank Noa Segev for conducting the interview which served as the basis for this paper, and for co-authoring the paper. Thanks to Sharon Amlani for the figures.
Footnotes
1. ↑For more information, see: https://www.who.int/data/gho/data/themes/hiv-aids#:~:text=Globally%2C_37.7_million_[30.2~,considerably_between_countries_and_regions.
2. ↑The global mortality rate for COVID-19 is estimated to be <6% [4]. This means that the mortality rates of HIV/AIDS is seven times larger than that of COVID-19.
3. ↑Research shows that psychological distress and lack of social support, which often result from HIV/AIDS stigma, increase engagement in sexual risk behavior. To learn more about it, see here.
4. ↑For more information about HIV treatment, see here: https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-treatment-basics
5. ↑To learn more about stem-cell transplant, see here to learn about the procedure with HIV-infected patients and read here about a case of a patient who recovered from HIV infection by special stem-cell transplant.
References
[1] ↑ Doitsh, G., and Greene, W. C. 2016. Dissecting how CD4 T cells are lost during HIV infection. Cell Host Microbe. 19:280–91. doi: 10.1016/j.chom.2016.02.012
[2] ↑ Gottlieb, M. S., Schroff, R., Schanker, H. M., Weisman, J. D., Fan, P. T., Wolf, R. A., et al. 1981. Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. N. Engl. J. Med. 305:1425–31. doi: 10.1056/NEJM198112103052401
[3] ↑ Barré-Sinoussi, F., Ross, A. L., and Delfraissy, J. F. 2013. Past, present and future: 30 years of HIV research. Nat. Rev. Microbiol. 11:877–83. doi: 10.1038/nrmicro3132
[4] ↑ Baud, D., Qi, X., Nielsen-Saines, K., Musso, D., Pomar, L., and Favre, G. 2020. Real estimates of mortality following COVID-19 infection. Lancet Infect. Dis. 20:773. doi: 10.1016/S1473-3099(20)30195-X
[5] ↑ Becker, M. H., and Joseph, J. G. 1988. AIDS and behavioral change to reduce risk: a review. Am. J. Public Health. 78:394–410. doi: 10.2105/AJPH.78.4.394
[6] ↑ Rubinstein, P. G., Aboulafia, D. M., and Zloza, A. 2014. Malignancies in HIV/AIDS: from epidemiology to therapeutic challenges. AIDS. 28:453–65. doi: 10.1097/QAD.0000000000000071
[7] ↑ Remien, R. H., Stirratt, M. J., Nguyen, N., Robbins, R. N., Pala, A. N., and Mellins, C. A. (2019). Mental health and HIV/AIDS: the need for an integrated response. AIDS. 33:1411–20. doi: 10.1097/QAD.0000000000002227
[8] ↑ Baingana, F., Thomas, R., and Comblain, C. 2005. HIV/AIDS and Mental Health.. World Bank. Available online at: https://openknowledge.worldbank.org/handle/10986/13741
[9] ↑ Mahajan, A. P., Sayles, J. N., Patel, V. A., Remien, R. H., Ortiz, D., Szekeres, G., et al. 2008. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 22 (Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62
[10] ↑ Evangeli, M. 2020. Why is it difficult for young people with HIV to share their diagnosis? Front. Young Minds. 8:163. doi: 10.3389/frym.2019.00163
[11] ↑ Havlir, D., and Beyrer, C. 2012. The beginning of the end of AIDS? N. Engl. J. Med. 367:685–7. doi: 10.1056/NEJMp1207138
[12] ↑ Barré-Sinoussi, F., Chermann, J. C., Rey, F., Nugeyre, M. T., Chamaret, S., Gruest, J., et al. 1983. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science. 220:868–71. doi: 10.1126/science.6189183
[13] ↑ Smith, C. J., Ryom, L., Weber, R., Morlat, P., Pradier, C., Reiss, P., et al. 2014. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D: A: D): a multicohort collaboration. Lancet. 384:241–8. doi: 10.1016/S0140-6736(14)60604-8
[14] ↑ Aldaz, P., Moreno-Iribas, C., Egüés, N., Irisarri, F., Floristan, Y., Sola-Boneta, J., et al. 2011. Mortality by causes in HIV-infected adults: comparison with the general population. BMC Public Health. 11:300. doi: 10.1186/1471-2458-11-300
[15] ↑ Trono, D., Van Lint, C., Rouzioux, C., Verdin, E., Barré-Sinoussi, F., Chun, T. W., et al. 2010. HIV persistence and the prospect of long-term drug-free remissions for HIV-infected individuals. Science. 329:174–80. doi: 10.1126/science.1191047
[16] ↑ Deeks, S. G., Lewin, S. R., Ross, A. L., Ananworanich, J., Benkirane, M., Cannon, P., et al. 2016. International AIDS Society global scientific strategy: towards an HIV cure 2016. Nat. Med. 22:839–50. doi: 10.1038/nm.4108