Abstract
Painful periods are unfortunately very common. Between 5 and 10% of all people who menstruate have endometriosis. Endometriosis is a chronic condition which causes severe period pain. It usually starts when a person begins to menstruate and keeps causing problems until menopause, the time of life when periods stop. Endometriosis can also affect the possibility of having children. On average, it takes 7 years before people with endometriosis find out what is causing their painful periods. Scientists and doctors do not know for sure why or how some people get endometriosis, and there is no cure for this difficult condition, but there are ways of managing it. In this article, we will describe what endometriosis is and how it can be recognized and managed.
The Menstrual Cycle
The menstrual cycle is much more than just “a period”, or a week of bleeding. It is a month-long process with many hormones involved. Some people like to think of the menstrual cycle as an orchestra (you can read more about the menstrual cycle in this article). In this orchestra, the hormones are like the various instruments—each plays its own part but also interacts with others. Sometimes they play loudly, other times they are quieter, but the instruments are always there. One of the most important hormones whose levels change dramatically over the course of the menstrual cycle is estrogen. Estrogen levels start low at the beginning of the cycle, peak after about two weeks, and then drop again. After estrogen levels drop, menstrual bleeding occurs, which most people call a “period” or menstruation. A period happens every cycle, which is about once every month.
Endometriosis
Every month, estrogen peaks and drops, so what? Well, the monthly peaks and drops in estrogen levels have other consequences besides menstruation. Menstrual bleeding is a normal process, but the fluctuations in estrogen levels can also cause spots called endometriosis lesions to grow. These lesions can grow throughout the body, but 99% of them are inside the abdomen. The problem with endometriosis lesions is that during menstruation, about 1 week every month, the lesions get irritated, which can cause severe pain. This pain is more than just a typical menstrual cramp, because it keeps coming back and can be so severe that it affects what a person can or cannot do.
Endometriosis is surprisingly common. Large studies have found that between 5 and 10% of all people with a uterus (womb) probably have endometriosis [1]. Think about it this way: if there are 20 people in your class, and 10 of them have periods, at least one person in your class probably has endometriosis (Figure 1). That is a lot of people, right?

- Figure 1 - It is estimated that 5%-10% of all people with a uterus have endometriosis.
- If your class contains 20 people, and 10 of them have a uterus, one will probably have endometriosis.
Where Does Endometriosis Come From?
Scientists have not yet completely figured how endometriosis develops, but they have some ideas. Many factors play a role, such as genes, lifestyle, inflammation, and environmental factors [2]. Stress probably also contributes to endometriosis, because being stressed for a long time can make the body more inflamed.
What are endometriosis lesions made of? Well, let’s take a step back. Remember the orchestra of hormones that “plays” every month during the menstrual cycle? These hormones affect the inner layer of the uterus, called the endometrium (Figure 2). After the bleeding part of the cycle, the endometrium grows to allow a potential pregnancy to nest there. If no pregnancy nests there (like in most cases), the endometrium breaks down, which results in menstrual bleeding. Endometriosis lesions are made of the same type of cells as the endometrium. This means they are affected by the hormonal changes of the menstrual orchestra. Just like the endometrium, they grow every cycle, but they cannot break down the same way. Instead, they get irritated, causing painful periods every month.
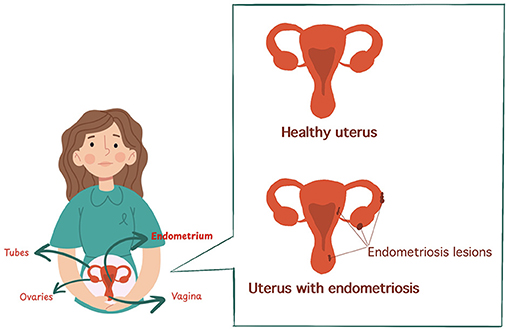
- Figure 2 - The uterus is a reproductive organ located in the abdomen of people assigned female at birth.
- The endometrium is the inner layer of the uterus, which grows and breaks down with the monthly hormonal fluctuations. Endometriosis lesions are made of tissue similar to the endometrium.
Diagnosing Endometriosis
If a person is having painful periods, it is good to get checked out by a doctor. Unfortunately, many people, including parents, other family members, and doctors, may think that pain during menstruation is normal and may not take young people seriously when they say they have pain. This is part of the reason why it often takes many years for a person with menstrual pain to get diagnosed with endometriosis. The exact length of time depends on the country the person lives in, but it is estimated to be around seven years [3]. Seven years is a long time to not know where the pain comes from or whether it will get better!
A Chronic Condition
One of the most difficult things about endometriosis is that it is chronic, which means that it does not go away by itself and it keeps causing problems for many years. The first symptoms usually show up around a person’s first period (on average around 12 years old). If endometriosis is not managed well, symptoms will get worse until their last period, which happens at menopause, which is usually around 50 years old. If you do the math, that is about 38 years!
As if having menstrual pain every month for 38 years is not enough, endometriosis can also cause other problems [4]. Over time, pain can start to happen during peeing or pooping, and even during sex. Endometriosis can also affect the possibility of having children (read this article to find out more about why some couples cannot have children). The problems caused by endometriosis build up over time. When symptoms first start, they usually show up only a couple of days each month. As the years pass, they can happen for a week every month, and eventually even every day, all month long. Many people with endometriosis start to miss out on school because of their symptoms and, later in their lives, might miss days of work too. While it may be fine to miss out on a couple of days of school or work due to sickness, skipping a week every month quickly piles up. This can make it difficult to get an education or keep a job.
Treating Endometriosis
You may now be wondering, “If endometriosis causes such problems for so many people, can it be treated”? The bad news is that endometriosis does not go away by itself and there is no cure for the condition. The good news is that there are ways to manage endometriosis symptoms [5]. Endometriosis is complex and looks a bit different for every person, so management is also different for every person. You can think of endometriosis management like a wall with four main blocks holding back symptoms (Figure 3):
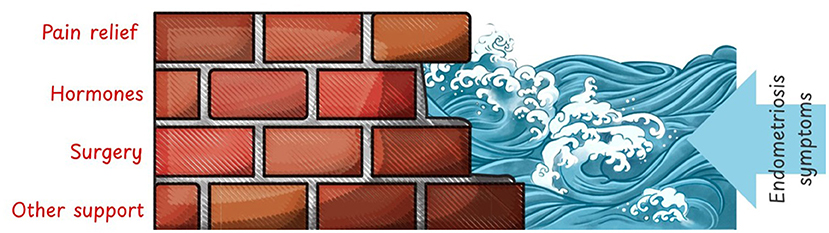
- Figure 3 - Endometriosis currently has no cure, but there are four main building blocks for managing the symptoms: pain relief, hormones, surgery, and other kinds of support, like help provided by nutritionists and mental health professionals.
Pain Relief
If someone is in pain, medicines called painkillers can help. While painkillers reduce the pain, they do not cure the underlying problem. Paracetamol is a common painkiller used to treat endometriosis symptoms.
Hormonal Suppression
As you have learned, endometriosis grows with the fluctuations in hormones during the menstrual cycle. A smaller number of fluctuations can slow that growth. One way to limit hormonal fluctuations is to use a contraceptive pill during the whole month, without stopping for a week to have a period. This can be done safely, even for years, and helps to keep the hormones in check.
Surgery
When endometriosis is so advanced that painkillers and hormonal suppression are not enough, surgery may be needed. If a person cannot get pregnant, sometimes surgery can also be helpful. The goal of surgery is usually to remove endometriosis lesions and keep the healthy organs, such as the uterus, in place. With no lesions to get irritated after surgery, the symptoms should be less. However, it is important to know that endometriosis often grows back. This is why hormonal suppression is needed even after surgery.
Supportive Measures
Many professionals besides gynecologists can help with endometriosis symptoms. For example, if what a person eats impacts the pain in their abdomen, a nutritionist can help figure out what is best for them to eat or not eat. Schools can help by giving students more information about endometriosis and by being flexible with schedules, for example, not making a student take exams on the most painful days of their cycle. People with endometriosis are often emotionally affected by it. Finding a group of people with similar experiences, such as an endometriosis patient organization, can offer important support. A psychologist can also help people to learn to deal with difficult emotions and take care of themselves.
Conclusion
Endometriosis is very common, and it causes serious pain and other severe problems. Unfortunately, not a lot of scientists study endometriosis, and we need more research to understand how and why endometriosis happens. It is also important to recognize endometriosis as early as possible, and to take people seriously if they say they have menstrual pain. Unfortunately, there is no cure for endometriosis, but there are ways of managing it. The best way to manage endometriosis is with a combination of pain relief, hormones, surgery, and other kinds of support like professional advice from nutritionists and psychologists. Hopefully, scientists will keep studying endometriosis and will find more and better treatments for it—improving the lives of many menstruating people all around the world.
Glossary
Hormones: ↑ Substances that travel through the body and have many different tasks, such as making a person grow, have periods, or feel hunger or thirst.
Estrogen: ↑ A hormone that helps control how a person grows and develops, especially during puberty. Everyone has estrogen, but it plays a bigger role in people assigned female at birth.
Endometriosis: ↑ A chronic condition that causes painful periods.
Lesions: ↑ Spots or areas on the body, inside or outside, that are hurt or not healthy. Lesions can be like small wounds or bumps.
Inflammation: ↑ A process that happens in the body in response to injury or when a person is stressed. Inflammation may cause tissue damage due to irritation of the inflamed cells.
Menopause: ↑ The time of life when periods stop, usually around 50 years.
Contraceptive Pill: ↑ Medication that is used to prevent a person from getting pregnant.
Gynecologist: ↑ A doctor specialized in taking care of people with a womb.
Conflict of Interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AI Tool Statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
[1] ↑ Moradi, Y., Shams-Beyranvand, M., Khateri, S., Gharahjeh, S., Tehrani, S., Varse, F., et al. 2021. A systematic review on the prevalence of endometriosis in women. Indian J. Med. Res. 154:446–54. doi: 10.4103/ijmr.IJMR_817_18
[2] ↑ Giudice, L. C., and Kao, L. C. 2004. Endometriosis. Lancet 364:1789–99. doi: 10.1016/S0140-6736(04)17403-5
[3] ↑ Staal, A. H. J., van der Zanden, M., and Nap, A. W. 2016. Diagnostic delay of endometriosis in the Netherlands. Gynecol. Obstetr. Investig. 81:321–4. doi: 10.1159/000441911
[4] ↑ Della Corte, L., Di Filippo, C., Gabrielli, O., Reppuccia, S., La Rosa, V. L., Ragusa, R., et al. 2020. The burden of endometriosis on women’s lifespan: a narrative overview on quality of life and psychosocial wellbeing. Int. J. Environ. Res. Public Health 17:4683. doi: 10.3390/ijerph17134683
[5] ↑ Becker, C. M., Bokor, A., Heikinheimo, O., Horne, A., Jansen, F., Kiesel, L., et al. 2022. ESHRE guideline: endometriosis. Hum. Reprod. Open. 2022:hoac009. doi: 10.1093/hropen/hoac009