Abstract
The menstrual cycle is more than just a period—it is a series of events that lasts the whole month. Across the menstrual cycle, sex hormones coordinate changes throughout the body, preparing it for a potential pregnancy. Like body temperature or pulse rate, the menstrual cycle is one measurement of the body’s basic functioning. When the cycle is not functioning as it should be, that might signal that something is wrong. There are several common disorders that cause irregular menstrual cycles. Although they are common, scientists, and doctors still do not know that much about them. We need more research to understand what causes menstrual cycle disorders and how to cure them. In this article, you will learn about hormones, the menstrual cycle, what happens when the menstrual cycle does not function as planned, and how we can learn more about the fascinating female body.
What is Puberty?
Have you noticed any changes in your body over the past few years? Maybe you are experiencing a growth spurt, or your voice is changing. During puberty, your body goes through many changes as it transitions from adolescence to adulthood. For people with a uterus, one of these changes is the start of the menstrual cycle. This is a sequence of events that happen each month to help the female body get ready for a possible pregnancy. How does the body “know” how to do this every month? This is hormones doing their job! In this article, you will learn about hormones, the menstrual cycle, what might cause irregular menstrual cycles, and how we can learn more about one of the superpowers of the female body.
What are Hormones?
Hormones are powerful chemical messengers that travel in the blood to various organs throughout the body. The job of hormones is to guide how the body works. We have hormones to thank for our ability to digest food, sleep, and grow. Sex hormones are a class of hormones that are responsible for sexual development and fertility. They direct the body through major transformations, such as puberty and pregnancy. Think about the growth of facial hair or the start of the menstrual cycle—sex hormones are responsible for these processes.
Estrogen, progesterone, and testosterone are three examples of sex hormones. Estrogen and progesterone are the main hormones produced by the ovaries, and testosterone is the main hormone produced by the testes. The production of these sex hormones is guided by another type of hormones called gonadotropins. Gonadotropins are very important for guiding the changes that happen across the menstrual cycle. Gonadotropins include follicle-stimulating hormone and luteinizing hormone. Follicle-stimulating hormone helps coordinate the growth of fluid-filled sacs in the ovary and luteinizing hormone triggers the release of the egg from the ovary in a process called ovulation.
What is the Menstrual Cycle?
When you think of the menstrual cycle, you probably think of someone getting their period. You may think of blood, cramps, and bloating. But the menstrual cycle is so much more than that! Across the month, the entire female body coordinates massive changes to prepare for potential pregnancy. These cyclical changes are guided by hormones estrogen, progesterone, follicle-stimulating hormone, and luteinizing hormone (Figure 1). The cycle can be broken down into two parts: the follicular phase is responsible for egg development, while the luteal phase prepares the uterus for pregnancy.
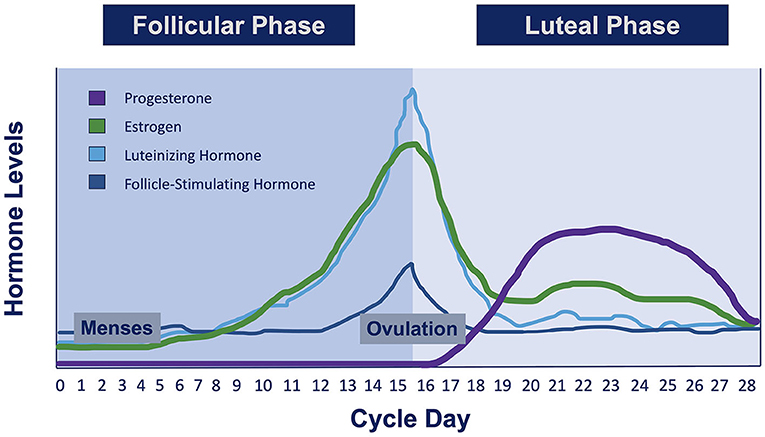
- Figure 1 - There are four main hormones that change across a typical 28-day menstrual cycle: estrogen, progesterone, luteinizing hormone, and follicle-stimulating hormone.
- During menses (when an individual gets their period), all of these hormones are relatively low. Around ovulation (when the egg is released from the ovary about halfway through the cycle), estrogen, luteinizing hormone, and follicle-stimulating hormone reach their highest levels.
The cycle begins on the 1st day of menses, when the inner lining of the uterus sheds, resulting in a few days of bleeding (Figure 2). This is what we may typically think of when we think about the menstrual cycle, but it is just the beginning! After menses, levels of estrogen and follicle-stimulating hormone begin to increase. This causes the inner lining of the uterus to thicken, and fluid-filled sacs in the ovary to form a mature egg. About halfway through this cycle, rising luteinizing hormone levels cause the ovary to release the mature egg. Increases in progesterone during the second half of the cycle help prepare the lining of the uterus for potential pregnancy. If the egg is not fertilized, estrogen and progesterone levels decrease. Decreases in these hormones cause the lining of the uterus to shed, starting the cycle all over again. So every month, the female body is able to regrow the lining of the uterus and shed it again if it is not needed. If regular, this coordinated process occurs without harming the body about 500 times throughout an individual’s life. Biologists think this process—the cyclic growth and shedding of the uterine lining—may hold answers to some of the greatest mysteries of biology, like how the body heals itself. Now that is a superpower!
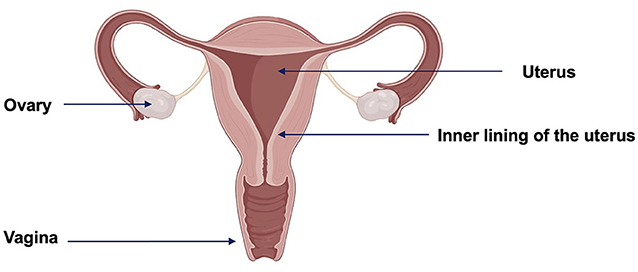
- Figure 2 - Female reproductive system.
- Menses occurs when the inner lining of the uterus sheds and exits the body through the vagina. This is considered the start of the menstrual cycle each month. About halfway through the cycle, an egg is released from one of the ovaries. Created with BioRender.com.
What Else Happens Across the Menstrual Cycle?
Hormones can travel to every part of the body and communicate with many types of cells. One of the most powerful organs, the brain, guides the creation of sex hormones and also responds to sex hormones. Research shows that brain structure and function change alongside changing estrogen and progesterone levels across the menstrual cycle [1, 2]. Hormone changes, particularly before menses, may also drive other changes throughout the body. Individuals who menstruate may have noticed feeling especially bloated, hungry, or sad during this part of the cycle.
What Might Cause an Irregular Menstrual Cycle?
It is very common for people who menstruate to have irregular cycles. They may go a few months without having a period or they may have cycles of very different lengths from month to month. Irregular cycles are especially frequent at the beginning of puberty when the body is adapting to this transition to adulthood. But sometimes changes in the menstrual cycle, or absence of a regular menstrual cycle, can mean something else is going on. The menstrual cycle is a vital sign, like temperature or pulse rate. This means that it can tell people if their bodies are functioning as they should be. When a vital sign is not as we expect, we should pay attention.
Some reasons for irregular or non-existent menstrual cycles include diet, exercise, and stress. When the body does not receive enough calories, this can mess with the normal production of gonadotropin and sex hormones, which can result in missed periods. Intense exercise or lots of stress can also interrupt natural fluctuations in hormones, leading to irregular menstrual cycles.
Sometimes, uncomfortable symptoms tied to the cycle are the result of serious disorders. Individuals with premenstrual dysphoric disorder may experience heightened depression, anxiety, and mood swings during the week or two before menses. Endometriosis is a chronic condition in which tissue that usually grows inside the uterus grows in other parts of the body, such as the bladder or the lining of the pelvic area (Figure 3A). Excessive pain during menstruation, heavy periods, chronic pelvic pain, fatigue, digestive issues, and depression are some of the symptoms of endometriosis [3]. Polycystic ovary syndrome is a chronic condition associated with the formation of many fluid-filled sacs in the ovaries, increased levels of androgen hormones, and missed periods (Figure 3B). Not getting a period for months could be a sign of polycystic ovary syndrome, and other symptoms include weight gain, male-pattern baldness, body hair growth, and depression [4]. Finally, fibroids are growths in the uterus that can cause longer periods and heavy menstrual bleeding (Figure 3C).
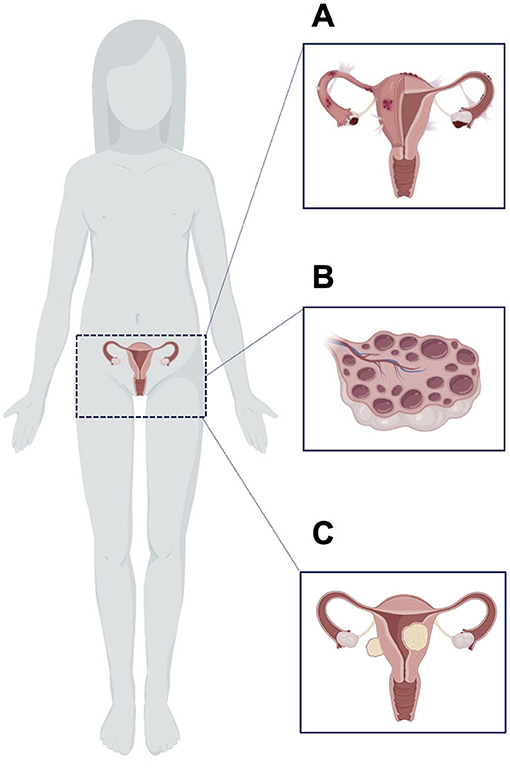
- Figure 3 - Three common causes of irregularities in the menstrual cycle.
- (A) In endometriosis, tissue that usually grows inside the uterus to be shed every month instead grows in other places, such as the fallopian tubes or ovaries. (B) Polycystic ovary syndrome is often characterized by fluid-filled sacs in the ovaries. (C) Fibroids are growths of muscle or tissue that can develop in or on the uterus. Created with BioRender.com.
We Still have a Lot to Learn!
Premenstrual dysphoric disorder impacts 5% of women, while endometriosis and polycystic ovary syndrome each affect 10% of women. Even though they are so common, we really do not know much about them! None of these disorders has a known cause or cure. Endometriosis and polycystic ovary syndrome are also leading causes of infertility in women. Endometriosis can take up to 10 years to correctly diagnose, and polycystic ovary syndrome can take up to 5 years! This means we still have a lot to learn. We know that both conditions are at least partially related to genetics. If you have a uterus, and your mom, sister, or grandmother had endometriosis or polycystic ovary syndrome, you are more likely to have it, too.
One thing these conditions have in common is that their symptoms can look very different in every individual. We need more research to understand what causes these extremely common, but understudied disorders. Fortunately, there are several ways we can work to improve our understanding of menstrual cycle irregularities. Menstrual cycles are not shameful. They are the engine by which humanity was born! They can also communicate that everything is working as it should be, just like temperature or heart rate. Menstrual cycles are processes to be proud of and things to pay attention to.
So do not be afraid to talk about the menstrual cycle and cycle irregularities with your friends, to spread your knowledge. We need to educate everyone—not just people who get a period—about what the menstrual cycle is and why sometimes it does not function as planned. This education needs to start in elementary school healthcare classes and continue into medical school education.
Finally, increasing gender diversity in science will improve our understanding of understudied topics, such as the menstrual cycle. Increasing gender diversity in sciences means making sure that all genders are studied in science and all genders are represented as the scientists asking the questions. Studying the biology of the menstrual cycle might hold important clues for the fields of biology and medicine. For example, a study done in 2019 found that substances from period blood can heal wounds [5]. Researchers are now looking at substances in menstrual blood to test for markers of endometriosis and fibroids. Imagine what else we could learn if we continue to study the menstrual cycle! For more information on the importance of diversity in science, see this Frontiers for Young Minds article: “Why neuroscience needs girls: Gender diversity drives scientific discovery”.
The menstrual cycle is a beautifully orchestrated series of events that occurs over the course of a month, preparing the body for a potential pregnancy. It should not be seen as a nuisance, but as a superpower!
Note
Though the article sometimes refers to women when discussing the menstrual cycle and related disorders, it should be noted that not all people who menstruate are women.
Glossary
Fertility: ↑ Ability to reproduce.
Gonadotropins: ↑ Hormones made in the brain that stimulate sex hormone production from the ovaries and testes.
Ovulation: ↑ Phase of the menstrual cycle when an egg is released from an ovary.
Follicular Phase: ↑ This is the first part of the menstrual cycle, when the egg is developed.
Luteal Phase: ↑ This is the second part of the menstrual cycle, when the uterus is prepared for a potential pregnancy.
Menses: ↑ Part of the menstrual cycle when the inner lining of the uterus is shed, resulting in a few days of bleeding.
Androgen Hormones: ↑ A group of hormones that guides reproductive development in males and guides muscle and bone development in both sexes.
Infertility: ↑ When an individual cannot get pregnant.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Pritschet, L., Santander, T., Taylor, C. M., Layher, E., Yu, S., Miller, M. B., et al. 2020. Functional reorganization of brain networks across the human menstrual cycle. NeuroImage 220:117091. doi: 10.1016/j.neuroimage.2020.117091
[2] ↑ Taylor, C. M., Pritschet, L., Olsen, R. K., Layher, E., Santander, T., Grafton, S. T., et al. 2020. Progesterone shapes medial temporal lobe volume across the human menstrual cycle. NeuroImage 220:117125. doi: 10.1016/j.neuroimage.2020.117125
[3] ↑ Saunders, P. T. K., and Horne, A. W. 2021. Endometriosis: etiology, pathobiology, and therapeutic prospects. Cell 184:2807–2824. doi: 10.1016/j.cell.2021.04.041
[4] ↑ Escobar-Morreale, H. F. 2018. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 14:270–284. doi: 10.1038/nrendo.2018.24
[5] ↑ Evans, J., Infusini, G., McGovern, J., Cuttle, L., Webb, A., Nebl, T., et al. 2019. Menstrual fluid factors facilitate tissue repair: identification and functional action in endometrial and skin repair. FASEB J. 33:584–605. doi: 10.1096/fj.201800086R
