Abstract
While many of the organs in our bodies are similar in men and women, the reproductive organs differ. The male and female sex cells, called gametes, differ too: sperm in the male and oocytes in the female. Male and female gametes must come together to make a baby. This amazing capacity to create a new life is called reproduction. The process of reproduction is quite complicated, and sometimes things can go wrong, preventing a couple from having a child—a condition called infertility. In this article, we explain how the reproductive cells normally meet and some of the problems that can happen along the way, resulting in infertility. We will also explain how some causes of infertility are treatable and we will describe several medical techniques that have been developed to help infertile couples to have babies.
How are Babies Made?
Making a baby is complicated. It all starts with a man and a woman, who make different sex cells, called gametes. Men produce sperm in organs called testes, by a process called spermatogenesis. Women make oocytes in organs called ovaries, by a process called oogenesis (Figure 1). Curiously, the testes are located outside the body, while the ovaries are inside. This is because it is too warm inside the body for healthy sperm production.
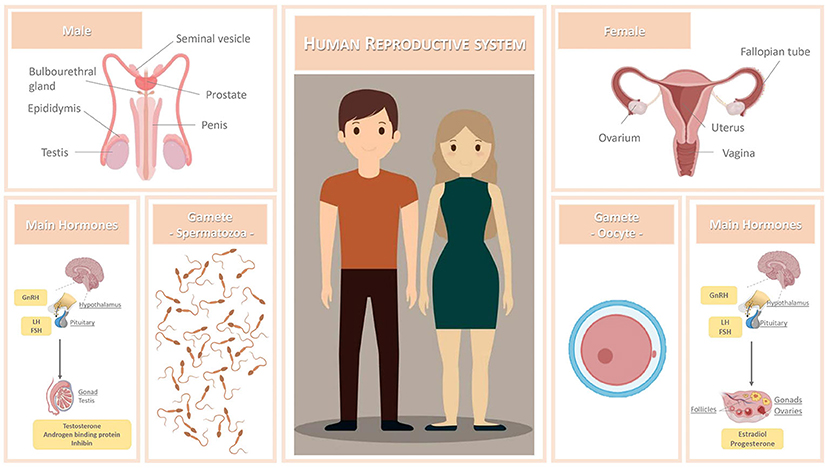
- Figure 1 - Human reproductive system.
- The main reproductive organs, the most important reproductive hormones (for more information on hormones see this website), and the male and female gametes are shown.
To create a baby, a sperm cell and an oocyte need to meet and join together, in a process called fertilization [1, 2]. Sperm have a special shape that allows them to swim fast in the reproductive fluids. In fact, these are the only cells in the body that can swim. The oocyte is much bigger than the sperm, and it serves as the main source of energy for the future baby. The sperm and the oocyte join in the female reproductive tract. Then, after several stages of development, an embryo is formed. The embryo grows inside the woman’s uterus (or womb). The uterus is a unique organ that can increase from the size of a pear to that of a watermelon during pregnancy.
Both the male and female reproductive systems have ducts, that are passages through which the gametes must travel to meet each other. Additionally, several substances, including hormones, must be produced to help gametes mature and survive.
What if Something Goes Wrong?
Reproduction is a complex process, and many things can go wrong. Sometimes when something goes wrong, it is not possible for a couple to have a child. If this situation persists for more than a year, these couples may be diagnosed with a condition called infertility [3, 4]. Infertility can also appear in couples that have already had a pregnancy. In that case, it is called secondary infertility [1, 3, 4]. Infertility affects nearly 50 million couples worldwide, and it is expected to get worse in the upcoming years.
What Causes Infertility?
For a doctor to understand the causes of infertility, both the man and the woman need to undergo tests because the problem could be with either partner. In some cases, both partners can contribute to infertility. Unfortunately, in around one-third of infertility cases, no cause can be identified [1, 3, 4].
Many factors can contribute to infertility. Sometimes these are factors that people are born with, while others are acquired during the man or woman’s lifetime. Examples include structural problems with parts of the reproductive system, for example the testes, ovaries, uterus, or penis. Other causes include the existence of infections or cancer (and cancer treatments) [1, 4]. Finally, genetic abnormalities or problems with the production of hormones can also cause infertility. In women, aging and obesity seem to have a special negative effect on fertility. In fact, female fertility starts to decrease in the mid-30s and greatly decreases after the age of 35. This is because women are born with a fixed number of oocytes in their ovaries, and this number decreases with age. Furthermore, the quality of oocytes decreases as they age. Men, however, can produce sperm daily during their entire lives, although men’s fertility might also decline after the age of 45 [2, 4]. The age factor is a big problem in today’s society. In fact, due to job or other life-related circumstances, couples frequently postpone having a child until they are older than 35, decreasing their chances of having a successful pregnancy [1, 3].
Lifestyle aspects such as diet and physical activity can also affect fertility. Also, addictive substances (e.g., tobacco, alcohol, drugs), and exposure to harmful agents (e.g., extreme temperatures, toxic compounds) can decrease fertility [1, 2, 4]. More recently, lots of attention has been given to a possible role of stress in infertility [5]. Nevertheless, when the identification of a cause is not possible, infertility is called idiopathic or unexplained [1, 4].
Are There Treatments for Infertility?
Before talking about treatments, it is crucial to highlight the importance of investing in reproductive health literacy. This is the most powerful tool that someone can have to support their reproductive health, as it can increase a person’s knowledge on topics ranging from the structures of the reproductive system, how fertilization happens, or even when a woman’s fertility is the highest. Reproductive health literacy will also promote awareness about risk factors and diseases that might harm fertility, empowering people to make healthy choices and to pay attention to their reproductive health so that they can quickly address any problems that might occur. Reproductive health literacy also teaches people that infertility is not anyone’s “fault,” reducing the social stigma that can be associated to those with fertility problems.
In terms of treatment, sometimes surgery can help. For example, surgery can remove tumors or the overgrowth of uterine tissue that happens in a disease of women called endometriosis. Surgery can also unblock ducts that are not allowing gametes to move through them. In other situations, doctors can prescribe medications that can be used to treat infections or that can otherwise improve fertility. A good example is a medication that can induce ovulation if a woman cannot release oocytes from her ovaries properly. Finally, in cases where men or women have abnormal hormone levels, doctors can offer them hormone treatments [1, 2, 4].
When it is not possible to identify a cause for infertility, doctors can still recommend treatments like dietary supplements, such as vitamins and antioxidants [1, 4], and they can remind patients to practice healthy lifestyle habits. These include a well-balanced diet, moderate exercise, and avoiding alcohol and tobacco use [1, 4].
Sometimes these treatments are not enough to restore fertility. In those cases, doctors may recommend techniques called assisted reproduction technologies. These technologies do not treat the cause of infertility but can still allow a couple to have a child [1, 2, 4]. There are 3 main types of assisted reproduction technologies that can be used, depending on the problems identified in the couple (Figure 2):
• Intrauterine insemination (IUI): In this technique, sperm cells are collected and placed directly in the uterus during the ovulation period. This treatment is advised when sperm cells have low motility (cannot swim well or fast enough), when vaginal sex is not possible (due to physical or psychological problems), or when having unprotected sex is not safe (e.g., if one partner has human immunodeficiency virus (HIV) or similar issues).
• In vitro fertilization (IVF): For this technique, the sperm and oocytes are collected and brought together in the laboratory. This means that the fertilization process occurs outside the body. Then, after 3–5 days, the embryo is transferred to the uterus. This technique is usually advised when a problem has been identified in the female, likely in the fallopian tubes.
• Intracytoplasmic sperm injection (ICSI): In this technique, sperm cells are collected from a man and analyzed by a scientist called an embryologist. The best sperm cell that is found is then injected into the oocyte. This technique is also performed in the laboratory. Similar to IVF, when the embryo is ready, it will be transferred to the uterus. ICSI is mostly used for couples in which the man has very few sperm cells and/or the sperm cells have low motility [1, 3].
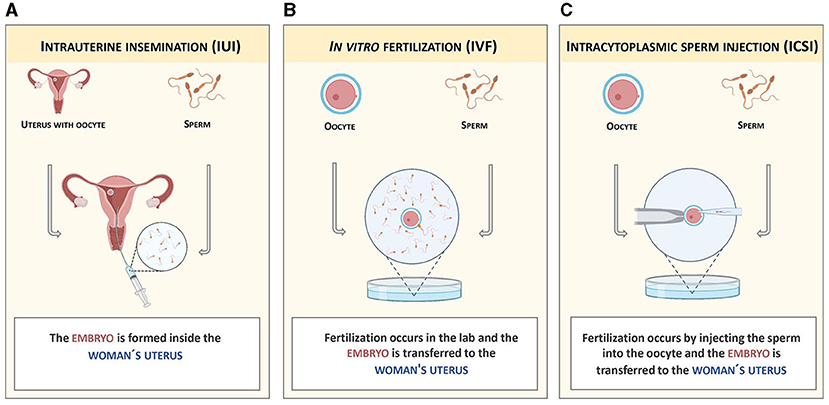
- Figure 2 - Main types of assisted reproduction technologies.
- (A) In IUI, the embryo is formed inside the woman’s uterus. (B) In IVF, fertilization and early embryo formation occur outside the body, in a lab. (C) ICSI is also performed in the lab but differs from IVF in the fertilization step. The sperm is injected into the oocyte by an embryologist using a microscope and other tools. IVF and ICSI allow doctors to monitor the development of the embryo and select the one(s) with the highest quality to be transferred to the woman’s uterus or to cryopreserve (freeze) for later use.
Unfortunately, the success rate of these techniques is not very high, and they do not work for all couples. In those cases, gamete donation can be an option. Many countries now have public banks of gametes—places where sperm and oocytes donated from healthy individuals are stored for further use. In these situations, assisted reproductive technologies must be used. The woman will give birth to a child that is genetically different from both (in the case of both oocyte and sperm donation) or one (in the case of sperm or oocyte donation) of the members of the couple. Surrogacy, carrying and giving birth to a baby for someone else, is also possible in some countries. However, laws usually only make surrogacy an option for women with medical conditions that make it impossible or dangerous to be pregnant. Surrogacy can also help single people and same-sex couples, yet it also depends on assisted reproductive technologies. Sadly, the possibility of never being able to have a child is also real. In this case, couples should have proper counseling with psychologists or other specialists. Adoption can also be a consideration for these couples.
Overall, although making babies is a complex process that is vulnerable to problems of various types, science and medicine are working hard to solve them and help couples to overcome fertility issues. However, it is important to keep in mind that being informed about these topics and choosing healthy habits are really important ways to minimize fertility issues. Every one of us can do our part to keep ourselves healthy and knowledgeable.
Glossary
Gametes: ↑ The reproductive cells of an organism, sperm in males and oocytes in females. Each gamete only carries half the normal amount of DNA.
Fertilization: ↑ The process in which the two gametes join and fuse to form an embryo.
Hormones: ↑ Important substances produced in several organs that work as chemical messengers in reproduction and other important processes.
Reproductive Health Literacy: ↑ Having knowledge about topics related to reproduction, which can be used to make good decisions about reproductive health.
Endometriosis: ↑ A disease affecting nearly 10% of women, in which the tissue that lines the uterus (called the endometrium) grows outside the uterus, causing pain and/or infertility.
Ovulation: ↑ The process by which an oocyte is released from the ovary, which makes the oocyte ready for fertilization.
Assisted Reproduction Technologies: ↑ Medical procedures that can help infertile couples to conceive a baby.
Surrogacy: ↑ When a woman carries and gives birth to a baby for someone else who cannot have children, helping them become parents through a special legal agreement.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was financed by Portuguese national funds via Fundação para a Ciência e Tecnologia (FCT), under the projects UIDB/04539/2020, UIDP/04539/2020, and LA/P/0058/2020. MC and AS were supported by FCT through PhD scholarships: 2021.05170.BD and SFRH/BD/129429/2017, respectively, at the scope of the PhD Programme in Experimental Biology and Biomedicine.
References
[1] ↑ Nieschlag, E., Behre, H. M., Nieschlag, S. 2010. Andrology: Male Reproductive Health and Dysfunction. Heidelberg: Springer. doi: 10.1007/978-3-540-78355-8
[2] ↑ Smith, R. 2017. Netter’s Obstetrics and Gynecology E-Book. New York, NY: Elsevier Health Sciences..
[3] ↑ Zegers-Hochschild, F., Adamson, G. D., Dyer, S., Racowsky, C., de Mouzon, J., Sokol, R., et al. 2017. The international glossary on infertility and fertility care. Fertil. Steril. 108:393–406. doi: 10.1016/j.fertnstert.2017.06.005
[4] ↑ Salonia, A., Bettocchi, C., Boeri, L., Capogrosso, P., Carvalho, J., Cilesiz, N. C., et al. 2022. European association of urology guidelines on sexual and reproductive health-2021 update: male sexual dysfunction. Eur. Urol. 80:333–357. doi: 10.1016/j.eururo.2021.06.007
[5] ↑ Simionescu, G., Doroftei, B., Maftei, R., Obreja, B. E., Anton, E., Grab, D., et al. 2021. The complex relationship between infertility and psychological distress. Exper. Therap. Med. 21:306. doi: 10.3892/etm.2021.9737