Abstract
Pain usually goes away after an injury, but for some children and teens, it lasts much longer. This kind of ongoing pain, called chronic pain, can make everyday life difficult. For many years, doctors did not have good ways to recognize or treat chronic pain in young people. Dr. Jennifer Stinson has worked to change that by listening carefully to what young people say about their pain and partnering with them to design better tools and treatments. She helped create tools like PainSCAN, Teens Taking Charge, and iCanCope, to make it easier for kids and teens to get the care they need. Her work has also helped train healthcare providers across Canada and beyond. Today, young people with chronic pain are not just patients—they are shaping the future of healthcare, thanks to leaders like Dr. Stinson who recognized that their voices matter.
Dr. Jennifer Stinson was awarded the 2025 Peter Gilgan Canada Gairdner Momentum Award “For international leadership in digital therapeutics and training initiatives focused on childhood illness- related pain assessment and self-management for conditions such as juvenile idiopathic arthritis, sickle cell disease, chronic pain and cancer”.
When Pain Does not go Away
Can you remember a time when some part of your body hurt? Maybe you scraped your knee, bumped your elbow, or had a bad headache or toothache. Usually, these types of pain go away in a few hours or days. For some kids, though, pain does not just disappear—it sticks around for weeks, months, or even years. This kind of ongoing pain is called chronic pain, and it can make everyday life hard for kids and their families.
Chronic pain in kids can have many causes. Some kids have medical conditions that cause ongoing pain by affecting their joints, blood, or other body parts over time. Others might have pain after an injury or surgery that does not heal the way it should. And sometimes, the pain does not seem to have a clear cause at all. Whatever the underlying cause, chronic pain has a huge impact on kids’ lives.
Kids with chronic pain often miss school, have trouble sleeping, or stop doing the things they love, like playing sports or hanging out with friends. For a long time, doctors and nurses did not have good ways to understand or treat chronic pain in children. That meant children’s pain was sometimes ignored or misunderstood—not because people did not care, but because they did not have the right tools to measure and manage it. When I became a nurse, I quickly saw that children’s pain was often not recognized or treated properly. There was a big gap between what I had learned in school and what was happening in real hospitals and clinics. That experience made me realize that better tools—and better research—were urgently needed to help kids with pain.
Listening to Kids—and Letting Them Lead
Doctors, nurses, and researchers often use special tools to measure pain, including number scales (“How much does it hurt from 0 to 10?”), checklists of symptoms, or diagrams that let a patient mark where their pain is. These tools help healthcare providers understand what a patient is feeling, especially when we cannot see the cause of the pain from the outside, like we can with a cut or a bruise. For a long time, most of these tools were made for adults, not kids. They were not always the right fit for children or teenagers, who might describe their pain differently, experience it in different ways, or need unique kinds of support.
When I first started working with children and teens who live with chronic pain, I did not just want to study them—I wanted to work with them to understand their experiences and create better ways to support them. I asked young people to tell me, in their own words, what their pain felt like, what made it harder to deal with, and what helped.
Kids and teens had all kinds of insights I had not seen in the research before. Some told me they wanted to track their symptoms using an app, not on paper forms. Others said that the way pain questions were worded did not match what they were feeling. I realized that if we wanted better tools, we had to build them together—not for kids, but with them. Over the past 20 years, I have built strong, trusting partnerships with young people and families across Canada to help guide this work. Their voices are at the center of everything I do. I try to follow the principle: “nothing for us, without us”, meaning that youth and families are involved at every stage—from designing research studies to testing and improving new tools. Listening to them has taught me more than any textbook ever could.
Building Better Ways to Recognize Kids’ Pain
As I worked with families and healthcare providers, I started to notice that some kinds of pain in children and teens were especially difficult to recognize. Pain caused by damage or problems in the nerves, which is called neuropathic pain, can happen after surgery, injury, certain infections, or medical treatments like chemotherapy for cancer. Neuropathic pain might feel like burning, tingling, or electric shocks. Another condition, called complex regional pain syndrome, sometimes shows up after a minor injury like a sprain or broken bone. For reasons we do not fully understand, the nervous system becomes overly sensitive, and the pain does not go away—it actually gets worse. The affected area might swell, change color or temperature, or become very painful to the touch. These conditions do not always show up clearly on tests or scans, and the symptoms can vary a lot, making it difficult for kids to get an accurate diagnosis and the right kind of care.
To help with this, a physical therapist and PhD student in my lab worked with my team to create a screening tool called Pediatric PainSCAN. This is a questionnaire that asks children and teens about the quality, location, and patterns of their pain, in words that make sense to them [1]. We worked closely with young people to test and improve this questionnaire. Their feedback helped us choose the right questions, get the wording right, and make sure it felt easy to use and matched what kids were feeling. The result is a tool that gives kids a stronger voice in the process—and helps doctors and nurses catch pain problems early and start treatment sooner, which can make a big difference (to learn more about Pediatric PainSCAN and the other tools described in this article, see my lab website).
Helping Teens Take Charge of Their Health
One thing I have learned over the years is that teens want to be involved in their own care—they just need the right tools and support. That is what led to Teens Taking Charge, a program I helped create for adolescents living with juvenile idiopathic arthritis (JIA) [2]. “Juvenile” means that it starts in children and teens, “idiopathic” means doctors do not know exactly what causes it, and arthritis is a disease that causes joint pain, stiffness, and fatigue. JIA can make everyday life more complicated, especially during a time when teens are trying to gain more independence.
Teens Taking Charge is a freely available web-based program that helps young people learn how to manage their symptoms, cope with stress, and stay involved in health decisions. It includes interactive lessons, quizzes, and videos. We also created a version for caregivers, so parents and guardians could support their teens without taking over. In a large national study, teens who used the program reported less pain and a better quality of life, and those improvements lasted up to a year later [2].
However, not every project went the way we hoped. A few years ago, we developed a gamified app to help kids with arthritis manage their pain. But just before we were ready to launch it, the company we were working with had to shut down. It was a tough disappointment—but it taught me an important lesson. Even when things do not work out, you can find new paths forward. After that, I built a stronger partnership with a hospital-based digital health team, and together we continue to create even better tools to support young people living with pain. Most importantly, this partnership makes sure that these tools will be supported far into the future.
We have also adapted our digital approach to other conditions, like sickle cell disease—a blood disorder people are born with that can cause sudden episodes of severe pain, along with long-term health complications. That program is called iCanCope with Sickle Cell Disease (Figure 1) [3]. For both iCanCope and Teens Taking Charge, the idea is the same: give teens easy-to-understand information, help them track their symptoms, teach them skills for managing stress and pain, and make space for them to set goals that matter to them.
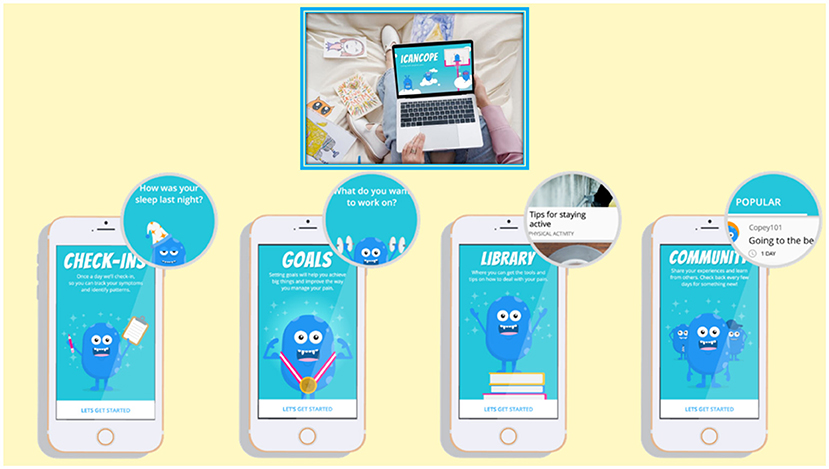
- Figure 1 - iCanCope with Pain is a digital pain education and self-management platform for kids living with painful conditions including sickle cell disease, chronic pain, arthritis, neurofibromatosis, and post-operative pain.
- It was built in collaboration with pain management experts from around the world and in partnership with young people living with pain. It allows users to track their symptoms, set goals, learn pain management skills, and get community support.
Changing the Way We Care for Kids in Pain
Creating new tools for kids and teens is one part of the work—but making sure those tools get used in real clinics, by real healthcare providers, is just as important. That is why I have also focused on changing the way we train doctors, nurses, therapists, and other professionals who care for children in pain. Many of them received only minimal training in how to assess or manage chronic pain in young people, especially the more complex cases. I wanted to help fill that gap in knowledge and improve their confidence to manage chronic pain in kids.
One way I have done this is through a program called Pediatric Project ECHO for Pain [4]. It is a virtual education series that connects doctors, nurses, therapists, and other community medical professionals so they can learn together, share knowledge, and get support as they apply new skills. We cover topics like how to assess pain in kids, how to use different treatment strategies—including physical, psychological, and medication-based approaches—and how to work with families as part of the care team. Thousands of professionals have participated, including providers in rural and remote areas who might not otherwise have access to this kind of training.
At the SickKids Pain Center, which I co-lead, we have a group of more than 60 youth and families who share ideas and give advice to help improve patient care, education, and research. Many of these young people have gone on to become doctors, nurses, psychologists, or researchers themselves. One young person who especially stands out developed chronic nerve pain after a minor sports injury. She was determined to overcome her pain and make a difference. She volunteered in my lab, mentored other young people through our iPeer2Peer mentoring support program, and later became a research coordinator. Today, she is a PhD student in my lab, working to create new ways to help young people with sickle cell disease feel more understood and supported. Watching young people take their experiences and turn them into ways to help others has been one of the most rewarding parts of my career.
Curiosity, Courage, and Collaboration
Over the years, I have worked with so many incredible young people who live with pain. They have taught me just as much as I have tried to teach them. They have helped shape better tools, better research, and better care (Figure 2). What is exciting is that these methods work! When teens have access to tools that are made for them—and when they are treated as partners in their care—they can learn to manage their health in ways that are both effective and empowering.

- Figure 2 - To create our tools, we work directly with a team of young people who live with chronic pain, so we can understand their needs and design the tools that will support them as best as possible.
- After the tools are designed and kids start to use them, the feedback those kids provide helps us to improve the tools, making them even better (figure credit: Somersault18:24).
If you are currently living with chronic pain, I hope this article reminds you that your voice matters. And if you are curious about science, healthcare, or helping others, you can be part of this kind of work, too. Whether you are drawn to technology, nursing, medicine, allied health, psychology, research, or education, there are so many ways to make a difference in the lives of children and teens.
If I could share a few pieces of advice, they would be these: first, stay curious and passionate. Some of the best ideas come from asking simple questions and not being afraid to think differently. Work hard and work together—collaboration and communication are just as important as individual effort. And never stop learning. Being open to feedback and keeping up with new tools, like the latest advances in technology and AI, will help you tackle challenges in ways we cannot even imagine yet. There are so many important problems waiting for new and fresh ideas. The next great idea could come from someone just like you!
Glossary
Chronic Pain: ↑ Pain that lasts for weeks, months, or longer. It can keep going even after an injury heals, and it can make everyday life very hard.
Neuropathic Pain: ↑ Pain caused by damage or problems in the nerves, often described as burning, tingling, or shooting sensations that can happen after injury, surgery, infection, or medical treatments.
Complex Regional Pain Syndrome: ↑ A condition where the nervous system becomes overly sensitive after an injury, causing lasting pain, swelling, and changes in skin color, temperature, or touch sensitivity.
Diagnosis: ↑ The process of figuring out what health problem a person has by looking at their symptoms, asking questions, and sometimes using tests like blood work, scans, or exams.
Screening Tool: ↑ Simple tests or questionnaires that help doctors and nurses quickly find signs of a health problem, even before a full diagnosis is made.
Juvenile Idiopathic Arthritis: ↑ A long-term illness in children that causes pain, swelling, and stiffness in the joints. “Idiopathic” means doctors do not know exactly what causes it.
Sickle Cell Disease: ↑ An inherited blood disorder where red blood cells are shaped like sickles instead of round, causing pain crises, anemia, and other serious health problems.
Psychological: ↑ Related to the mind, thoughts, emotions, and behavior. Psychological treatments often focus on how people feel, think, and cope with challenges.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I wish to thank Dr. Susan Debad for her thoughtful questions, collaborative input, and her contributions as co-author. Figure 2 was created by Somersault18:24. I would like to acknowledge grant funding from the Canadian Institutes of Health Research, the American Society for Peripheral Nerve, and The Plastic Surgery Foundation, The Mayday Fund, The Canadian Arthritis Network, The Arthritis Society, and National Institutes of Health.
AI Tool Statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
[1] ↑ Mesaroli, G., Campbell, F., Hundert, A., Birnie, K. A., Sun, N., Davidge, K. M., et al. 2022. Development of a screening tool for pediatric neuropathic pain and complex regional pain syndrome: pediatric painscan. Clini. J. Pain 38:15–22. doi: 10.1097/AJP.0000000000000993
[2] ↑ Stinson, J. N., Lalloo, C., Hundert, A. S., Campillo, S., Cellucci, T., Dancey, P., et al. 2020. Teens taking charge: a randomized controlled trial of a web-based self-management program with telephone support for adolescents with juvenile idiopathic arthritis. J. Med. Intern. Res. 22:e16234. doi: 10.2196/16234
[3] ↑ Palermo, T. M., Zempsky, W. T., Dampier, C. D., Lalloo, C., Hundert, A. S., Murphy, L. K., et al. 2018. Icancope with sickle cell pain: design of a randomized controlled trial of a smartphone and web-based pain self-management program for youth with sickle cell disease. Contemp. Clini. Trials 74:88–96. doi: 10.1016/j.cct.2018.10.006
[4] ↑ Lalloo, C., Mohabir, V., Campbell, F., Sun, N., Klein, S., Tyrrell, J., et al. 2023. Pediatric Project ECHO® for Pain: Implementation and mixed methods evaluation of a virtual medical education program to support interprofessional pain management in children and youth. BMC Med. Educ. 23:71. doi: 10.1186/s12909-023-04023-8
