Abstract
Imagine a tiny lab in a box that can make medicines right in the hospitals where patients are being treated. Even better, the medicines would be perfectly designed to treat each person’s specific disease! This futuristic-sounding method is the aim of a new project called NANOSPRESSO. The medicines would consist of microscopic “delivery trucks” called nanoparticles which, once injected into the body, could take the medicines directly into the cells that need them. The medicines inside the nanoparticles would be made of instruction molecules called nucleic acids that tell the cells how to fix the exact cellular problems that are causing the disease. Producing medicines using NANOSPRESSO would be much quicker and more flexible than making them in factories, which could make this method especially useful for treating rare diseases for which no medicines are currently being made. NANOSPRESSO could change the way we treat diseases, making advanced and personalized treatments available to more people around the world.
Where Do Medicines Come From?
Have you ever been sick and needed to take medicine for a cold or an infection? Maybe your doctor prescribed some pills or a liquid medicine that your parents had to pick up from the pharmacy. While today’s pharmacists check prescriptions and make sure to hand out the right medicines, they do not actually make the medicines we take—most are made in giant pharmaceutical factories and shipped to pharmacies, stores, and hospitals around the world.
But things were not always this way. Did you know that, in the past, medicines were often made right in the pharmacy itself? Not too long ago, pharmacists mixed ingredients by hand to create the exact medicine each individual patient needed, according to a doctor’s prescription. This process, which creates personalized treatments, is called compounding. But as medical science advanced and the demand for medicines grew, drug development and manufacturing moved to big factories called pharmaceutical companies. These companies developed ways to produce medicines in huge batches, making those medicines cheaper and ensuring that pharmacies and hospitals always had supplies ready for patients.
Large-Batch Medicines Are Not Always Better
While pharmaceutical factories work well for producing common, “one-size-fits-all” medicines like vaccines and painkillers, this method also creates some problems. Mass-produced medicines are created to work for as many people as possible, but not everyone responds to a medicine the same way. A treatment that works well for one person might not be as effective for someone else. This is especially true for complex diseases like cancer, or for other conditions that require specific treatments based on a patient’s unique characteristics. When medicines are only produced in a few large facilities, shortages can happen if those facilities experience production problems, material shortages, or shipping delays. Finally, producing and shipping medicines on such a large scale also uses a lot of energy and resources, adding to pollution and waste.
Even more concerning are rare conditions, called orphan diseases, for which no effective medicines exist. Developing a new medicine is super expensive, so pharmaceutical companies tend to focus on common diseases that affect lots of patients—it is generally not profitable for companies to spend millions of dollars to develop treatments that only a small number of people need. That means patients with rare conditions often have no treatment options, even though there are approximately 7,000 known orphan diseases that together affect more than 300 million people worldwide [1, 2]!
Recently, scientists have been working on a new way to make medicines—a method that is more like compounding. This new approach, called NANOSPRESSO, aims to produce personalized medicines locally, right in hospitals where patients need them, instead of relying on large factories.
What is NANOSPRESSO?
Maybe you have seen one of those cool soda machines—the kind where you pick your favorite soda, like Coke or Sprite, and then add custom flavors such as cherry, vanilla, or lime to create your own personalized drink. Or maybe your parents use a coffee machine where they pop in a small capsule of their choice and get a fresh cup of coffee, made just the way they like it. That is the basic idea behind NANOSPRESSO, a new way to make small, personalized batches of medicine right in the hospital. The name “NANOSPRESSO” comes from nano, meaning tiny particles, and espresso, a type of coffee made quickly using a special machine—to describe the way this system quickly makes tiny particles containing the exact medicines needed by each patient, according to their specific disease.
But making medicines is much more complicated than making an espresso at home or mixing flavors into your soda. The medicines that NANOSPRESSO creates are made from nucleic acids—molecules of RNA or DNA that carry the instructions telling the body’s cells how to make proteins. Proteins are the building blocks of the body, responsible for everything from making muscles move to fighting infections. But when cells make too much or too little of some proteins, or when certain proteins do not work properly, diseases can result. Nucleic acid medicines can be specially designed to provide cells with the correct instructions to make a critical missing protein. Also, in cases where cells are producing a malfunctioning protein that causes a disease, nucleic acid medicines can stick to and “block” the patient’s faulty genetic instructions before they can produce the problem protein (Figure 1).
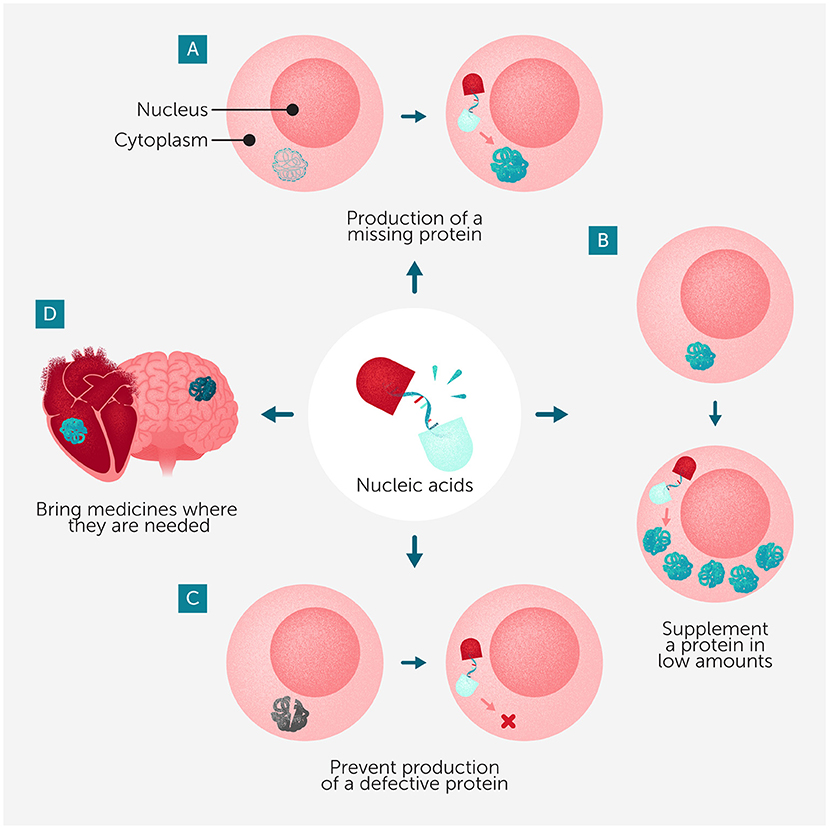
- Figure 1 - The nucleic acid medicines made using NANOSPRESSO can be designed to: (A) help cells to produce an important protein that they normally cannot produce; (B) help cells to make more of a protein they are not making enough of; or (C) stop cells from making an incorrect or malfunctioning protein that might cause problems.
- (D) NANOSPRESSO-based medicines could be designed to be delivered precisely to the organs where they are needed.
Delivering Nucleic Acids to Cells is Challenging
Delivering nucleic acid medicines into cells is not easy. Nucleic acids are usually much larger than typical medicines, and they have a negative charge—two features that make it hard for them to pass through a cell’s protective outer membrane. Nucleic acids are also delicate and can break down quickly inside the body. Without protection, these medicines would be destroyed before they could reach the right cells. So, for these medicines to work, scientists first needed to find a way to package nucleic acids so they could safely reach their target inside the body.
One way to solve this problem is to wrap nucleic acids inside nanoparticles—extremely tiny, man-made particles that can carry and protect their contents [3, 4]. These nanoparticles act like delivery trucks, safely transporting the medicine through the body to its target. The most common type of nanoparticles used for nucleic acid medicines are called lipid nanoparticles (LNPs). Lipids are fat-like molecules that can form tiny bubbles around the medicine, shielding it from damage and helping it slip into cells (Figure 2). If the Earth were shrunk down to the size of a football, and then that football was shrunk down by the same amount, the result would be about the size of a lipid nanoparticle! Nanoparticles can be designed to release their cargo at just the right time once they have entered cells. Scientists can also modify nanoparticles to “target” them to specifically enter certain tissues, such as the liver or muscles.
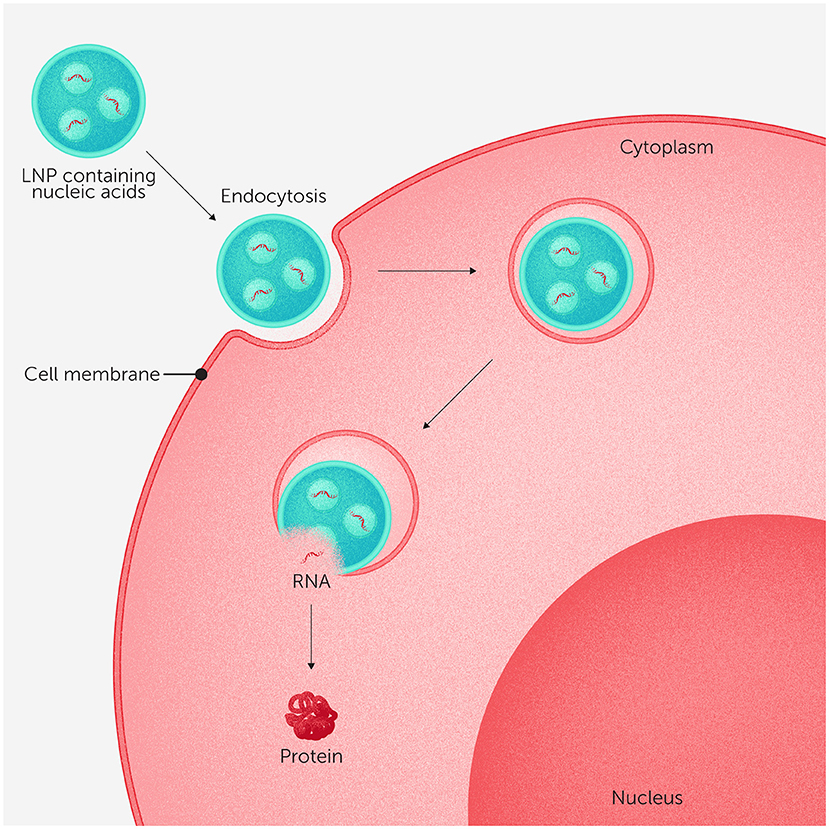
- Figure 2 - Lipid nanoparticles (LNPs) can form tiny bubbles around nucleic acid medicines, protecting the delicate nucleic acids and helping them to enter cells.
- LNPs are taken up into cells through a process called endocytosis, in which the cell membrane wraps around the LNP and pulls it inside. Once inside the cell, the LNPs break open—like a popped bubble—and release their nucleic acid cargo, which the cell can then use to make helpful proteins (for more details on how cells turn RNA into proteins, see this site).
Nanoparticle technology is not new to NANOSPRESSO. In fact, it has already played a key role in a medical breakthrough you are probably personally familiar with—the mRNA COVID-19 vaccine [5, 6]. This vaccine uses LNPs to safely deliver genetic instructions for making a harmless protein from the virus. Once inside cells, these instructions activate the body’s defense system, preparing it to fight the actual virus if it is encountered. Scientists are now using similar nanoparticle-based delivery systems for other diseases, so that the medicines they contain safely reach the patient’s diseased cells. NANOSPRESSO takes this a step further by making it possible to produce customized nucleic acid medicines for specific patients, right when they are needed in hospitals or clinics.
Making Personalized Medicine with NANOSPRESSO
To make a personalized medicine using NANOSPRESSO, the first step is to analyze a patient’s genetic makeup to identify the faulty genes or proteins causing their disease, and to determine whether a nucleic acid therapy could help. Once doctors know which nucleic acid medicine a patient needs, a custom cartridge is put together specifically for them—the way a custom coffee machine uses specific capsules to brew different kinds of coffee depending on each person’s taste. Each cartridge, about the size of a smartphone, has two compartments. One compartment holds the patient’s nucleic acid medicine, and the other holds the lipid mixture needed to form protective nanoparticles (Figure 3). The cartridge also contains thin channels where the ingredients can mix together, called a microfluidic mixing system.
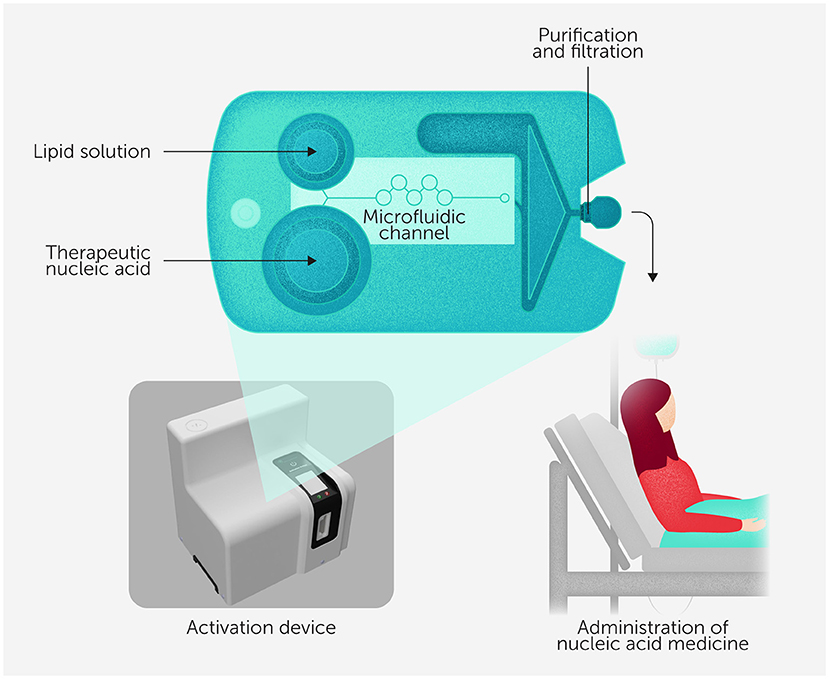
- Figure 3 - An example NANOSPRESSO cartridge, which is about the size of a smartphone.
- The lipid mixture and the nucleic acid medicine are originally contained in two separate compartments. The cartridge is inserted into the activation device, which mixes the two ingredients by pushing them out of their compartments into the thin (microfluidic) channels. This mixing creates stable nanoparticles, which are purified as they are pushed through a filter when leaving the cartridge. Finally, the purified medicine is injected into the patient. The entire process takes only minutes!
The cartridge is inserted into the NANOSPRESSO activation device, which creates a carefully controlled amount of pressure to push tiny liquid droplets from the two compartments into the microfluidic channels, mixing them very precisely. Microfluidic mixing combines the ingredients in just the right way to form stable nanoparticles. The result? A fresh batch of medicine, made quickly and safely right at the hospital, ready to be injected into the patient.
NANOSPRESSO could create treatments for many different diseases, including orphan diseases that currently have few or no treatment options. One example is methylmalonic acidemia, a disorder where the body cannot properly break down certain foods, leading to a dangerous buildup of toxic substances. Another is Crigler-Najjar syndrome, a rare liver disease that prevents the body from getting rid of waste products in the blood, which can lead to serious complications. Both conditions are caused by missing or faulty proteins, meaning they could potentially be treated using nucleic acid medicines that instruct cells to make the correct proteins.
NANOSPRESSO’s ability to make small, personalized batches of medicine could also be useful in cancer treatment. Some cancer therapies work by helping the body’s defense system recognize and attack tumors. With NANOSPRESSO, hospitals could prepare these immune-based therapies on demand, instead of waiting for them to be produced in large pharmaceutical factories. Additionally, this technology could help doctors respond quickly to emerging diseases. When a new virus appears, for example, NANOSPRESSO could be used in hospitals to create small batches of vaccines right where the new virus is infecting the most people, helping communities respond to outbreaks much faster than traditional vaccine manufacturing allows.
Can NANOSPRESSO Make Specialized Medicines Available to Everyone?
One big advantage of NANOSPRESSO is that it does not require designing a brand-new treatment system for every disease. Nucleic acids all have the same basic arrangement of molecules, so nucleic acid medicines only need to differ in their sequence and length. This means the same type of cartridge and mixing system can be used for many different medicines, making it much easier and more affordable to create new treatments. The technology is also designed to be simple enough for trained hospital staff to use, so it does not require highly specialized manufacturing experts. Overall, NANOSPRESSO could make it easier for patients everywhere to get the personalized treatments they need, no matter where they live or how rare their diseases are. In many parts of the world, access to advanced medicines is limited because they are expensive to ship and can require refrigeration. With NANOSPRESSO, doctors could produce these medicines locally, making sure effective treatments reach patients in remote or underserved areas.
Currently, NANOSPRESSO is still being developed, and there are still challenges to solve before it can be widely used. The rules governments set up to make sure medicines are safe were designed for factory-made drugs, so new rules need to be developed to ensure the safety of small batches of medicines made in hospitals. Another challenge is cost. Right now, nucleic acid medicines are expensive to produce, and hospitals would need the right equipment and would have to train their staff to use NANOSPRESSO effectively. Scientists are working on ways to make the process more affordable and ensure that every dose is safe and effective.
Once these remaining challenges are solved, NANOSPRESSO could one day be available to millions of patients around the world—providing much-needed treatments for orphan diseases, personalized therapy for certain cancers, and even new vaccines. By moving medicine production from big pharmaceutical companies to exactly where the treatments are needed, NANOSPRESSO offers a promising step toward a future where effective, personalized medicines are available on demand to more people than ever before.
Glossary
Pharmaceutical: ↑ Related to making or using medicines, especially in factories or companies that produce drugs for doctors, hospitals, and pharmacies to treat diseases.
Personalized Treatments: ↑ Medicines or therapies designed specifically for one person, based on their unique genes, disease, or body, instead of using the same treatment for everyone.
Compounding: ↑ The process of mixing ingredients to make a custom medicine for a specific patient, usually done by a pharmacist instead of a factory.
Orphan Diseases: ↑ Rare diseases that affect only a small number of people and often do not have treatments because making medicines for them is not very profitable for pharmaceutical companies.
Nucleic Acids: ↑ Molecules like DNA and RNA that carry instructions telling cells what to do, such as how to make proteins that keep the body working properly.
Proteins: ↑ Tiny machines or building blocks in the body that do important jobs, like helping muscles move, fighting germs, or carrying messages between cells.
Nanoparticles: ↑ Extremely tiny particles that can carry medicines through the body and help them get into the right cells, like microscopic delivery trucks.
Microfluidic Mixing: ↑ A way to mix very small amounts of liquids through tiny channels, helping scientists create things like nanoparticles quickly and precisely, often inside a special cartridge or device.
Conflict of Interest
RS is VP preclinical R&D of Nanocell Therapeutics was employed by CelluTx Inc.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank the young reviewers Aanya, Ayushi, Rayna, Anabelle, and Harish for their thoughtful feedback and enthusiastic collaboration during the review process. Their questions and insights greatly contributed to improving the clarity and impact of our work. Edited by Susan Debad Ph.D., graduate of the UMass Chan Medical School Morningside Graduate School of Biomedical Sciences (USA) and scientific writer/editor at SJD Consulting, LLC. We would like to thank the coauthors of the original manuscript. The project NANOSPRESSO-NL received funding from the Netherlands Science Agenda-Netherlands Organization for Scientific Research Grant No. NWA.1389.20.096. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Original Source Article
↑Estap, Ã., Senti, M., Ceccaldi, A., Luciani, M., Saber, N., Schurmann, P. J. L., et al. 2025. NANOSPRESSO: toward personalized, locally produced nucleic acid nanomedicines. Front. Sci. 3:1458636. doi: 10.3389/fsci.2025.1458636
References
[1] ↑ The Lancet Global Health 2024. The landscape for rare diseases in 2024. Lancet Glob. Health 12:e341. doi: 10.1016/S2214-109X(24)00056-1
[2] ↑ Cavaller-Bellaubi, M., Hughes-Wilson, W., Kubinová, Š., Van de Casteele, M., Van Lente, E. J., Degortes, E., et al. 2023. Patients, payers and developers of Orphan Medicinal Products: lessons learned from 10 years’ multi-stakeholder dialogue on improving access in Europe via MoCA. Orphanet. J. Rare Dis. 18:144. doi: 10.1186/s13023-023-02774-7
[3] ↑ Akinc, A., Maier, M. A., Manoharan, M., Fitzgerald, K., Jayaraman, M., Barros, S., et al. 2019. The Onpattro story and the clinical translation of nanomedicines containing nucleic acid-based drugs. Nat. Nanotechnol. 14:1084–7. doi: 10.1038/s41565-019-0591-y
[4] ↑ Jayaraman, M., Ansell, S. M., Mui, B. L., Tam, Y. K., Chen, J., Du, X., et al. 2012. Maximizing the potency of siRNA lipid nanoparticles for hepatic gene silencing in vivo. Angew. Chem. Int. Ed. 51:8529–33. doi: 10.1002/anie.201203263
[5] ↑ Schoenmaker, L., Witzigmann, D., Kulkarni, J. A., Verbeke, R., Kersten, G., Jiskoot, W., et al. 2021. mRNA-lipid nanoparticle COVID-19 vaccines: structure and stability. Int. J. Pharm. 601:120586. doi: 10.1016/j.ijpharm.2021.120586
[6] ↑ Suzuki, Y., and Ishihara, H. 2021. Difference in the lipid nanoparticle technology employed in three approved siRNA (Patisiran) and mRNA (COVID-19 vaccine) drugs. Drug Metab. Pharmacokinet. 41:100424. doi: 10.1016/j.dmpk.2021.100424