Abstract
Sepsis is a life-threatening reaction to an infection in which the immune system, which usually helps fight infections, reacts abnormally and can cause organs to stop working. About 20% of deaths worldwide are attributed to sepsis—more than any type of heart disease or cancer. Sepsis can be difficult for doctors to recognize because symptoms start out similar to many other medical conditions, and it is hard to treat because the bodily “malfunctions” that cause sepsis vary between patients. To recognize sepsis early and understand differences between patients, researchers are looking at many parts of the immune system at once, collecting lots of data on patients’ genes and proteins. Computers are used to analyze the data, to identify unique patterns or connections. By doing so, scientists have identified unique groups of sepsis patients that differ in their immune responses. This knowledge can help doctors choose the best treatment for each person and might even help protect people from severe COVID-19 or future pandemics.
Sepsis—A Major Medical Emergency
At some point, you have probably had an infection—maybe a cut or scrape you got while playing outdoors became red and swollen; or maybe you had a fever and cough and were diagnosed with the flu, pneumonia, or COVID-19. You may have recovered on your own or been prescribed some medicines to treat the infection, but chances are you got better without too much trouble—thanks to your immune system. Normally, the immune system acts like a well-trained defense team, identifying and attacking harmful invaders and helping our bodies recover. But sometimes things can go wrong.
When some people get serious infections, especially older people or those who are already sick or weak, the immune system might become dysregulated. In these cases, the immune system does not react to infection the way it should—for example, it might overreact, damaging healthy parts of the body, or not react strongly enough, allowing germs to spread more easily. Immune system dysregulation can lead to a very serious medical condition called sepsis—an abnormal, life-threatening response to infection that affects the whole body. Think of it like a fire that breaks out in one room but then quickly spreads through the entire house. In the worst cases, sepsis can cause vital organs like the heart, lungs, and kidneys to stop working properly, leading to death.
You might be surprised to learn that sepsis is one of the leading causes of death worldwide. In fact, sepsis causes almost 1 in 5 deaths each year—more than any type of heart disease or cancer! In 2017 alone, sepsis killed about 11 million people [1]. Many people do not realize how common and deadly sepsis is, partly because it is not always listed as the cause of death—often, it is “hidden” behind other infections or diseases the person might have been suffering from. The COVID-19 pandemic highlighted this problem, as most of the deaths caused by severe COVID were actually due to sepsis, in which the virus triggered a dysregulated immune response [2].
Currently, sepsis treatment involves medicines to fight the underlying infection and supportive care to keep the organs functioning—but there are no treatments to fix the immune system dysfunction that causes sepsis in the first place. Sepsis treatments might work in some patients but not in others and, even with current treatments, >22% of people hospitalized with sepsis die [1].
Sepsis Symptoms Can Differ Between Patients
One of the things that makes sepsis so deadly is that it is often difficult for doctors to know when patients have it. The early symptoms of sepsis can look like those of many other common health problems—abnormal body temperature, blood pressure, breathing rate, and heart rate, for example—making early diagnosis difficult [3]. Another thing that makes sepsis difficult to diagnose is that the symptoms can be different for each patient, so there is no one list of symptoms that doctors can “check off” to confirm that sepsis is the problem. The longer it takes a doctor to diagnose sepsis, the sicker the patient gets, and the more difficult the sepsis is to treat. Variability also helps to explain why some treatments might not work for every patient.
Researchers still do not know why sepsis is so variable. Variability could be caused by patient factors, like age, sex, genes, other diseases the patient might have, and the types of medicines they are taking. Variability might also come from factors specific to the infection, like which type of organism caused it (e.g., bacteria or virus), the original site of infection (e.g., lungs, urinary tract, or skin), or how long the patient has had the disease (Figure 1).
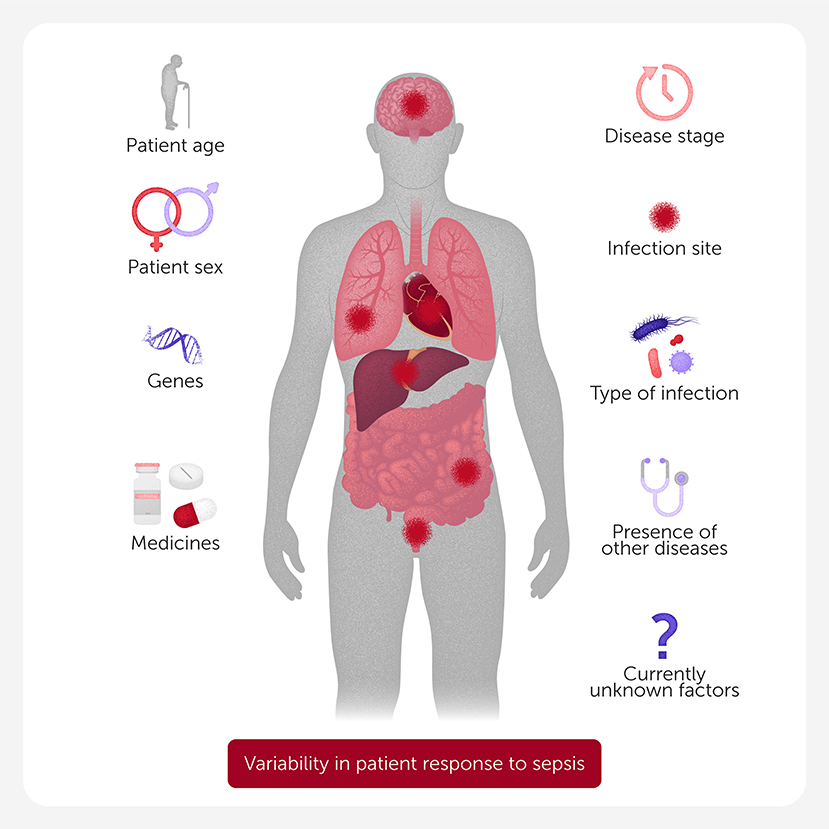
- Figure 1 - Sepsis is often difficult to diagnose because the early symptoms can be seen in other diseases and can differ between patients.
- Researchers are still unsure why sepsis is so variable, but several factors probably play a role—both patient factors, like age, sex, genes, medicines, and the presence of other diseases; and infection-specific factors, like the type of infection, the part of the body that is infected, and the disease stage. Other still-unknown factors probably play a role, too.
To improve sepsis diagnosis and treatment, researchers first need to understand what is happening in the immune systems of individual patients. Maybe understanding the ways the immune system becomes dysfunctional might help explain why sepsis symptoms are so variable between patients.
Seeing the Big Picture
Imagine trying to complete a 1,000-piece jigsaw puzzle. How would you tackle this challenge—would you “zoom in”, to focus on the tiny details of each individual puzzle piece, or “zoom out” and look at the “big picture” on the box? Probably a little bit of both, right? But without the big picture, it would be a lot harder to put the puzzle together.
Like a huge jigsaw puzzle, the immune system has hundreds of components. Many types of cells and proteins work together to protect our bodies from invaders. The dysregulation that occurs during sepsis can involve many of the “puzzle pieces” of the immune system, and it affects other bodily systems, too. While “zooming in” to study how one type of cell or protein acts during sepsis can give researchers some important information, only by “zooming out” can they see how all the pieces work together and how the complex coordination might go wrong. This type of “big picture” approach, in which mathematical analysis is used to help researchers understand immunity, is called systems immunology [4]. But how exactly can researchers use systems immunology to understand sepsis?
Studying Active Genes Uncovered Five Types of Sepsis
One way that researchers have been using systems immunology to understand the “big picture” of the immune system in sepsis is to look at which immune system genes are active (turned on) in sepsis patients. As you might already know, genes are cellular instructions for making proteins—the molecules responsible for nearly everything that happens in our bodies, from building tissues and organs to fighting off infections (Figure 2A). During sepsis, certain genes become more active than usual, while others may become less active, affecting how the immune system responds.
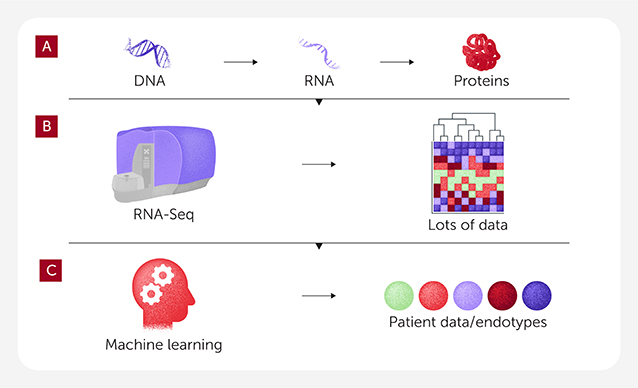
- Figure 2 - (A) Genes, made of DNA, contain the instructions for making proteins.
- When genes become activated, they first make an RNA copy of the DNA, then the RNA is used as a template to assemble the protein. This means that the presence of RNA can tell researchers if a gene is active or not. (B) Using RNA-Seq, researchers can figure out which genes are turned on (or not) in sepsis patients. RNA-Seq generates a lot of data. (C) Using machine learning, a type of artificial intelligence, researchers identified patterns in the gene data of sepsis patients, allowing patients to be divided into five unique groups, called endotypes.
Researchers can use powerful laboratory techniques, including a method called RNA-Seq, to study how active each gene is. Essentially, they “measure” the gene activity in a patient’s cells by looking at the production of RNA, which happens when a gene is activated to make proteins (Figure 2B). By looking at how active (or inactive) certain genes are in sepsis patients, researchers can begin to understand how the immune system is dysregulated in sepsis and how it behaves differently from one person to another.
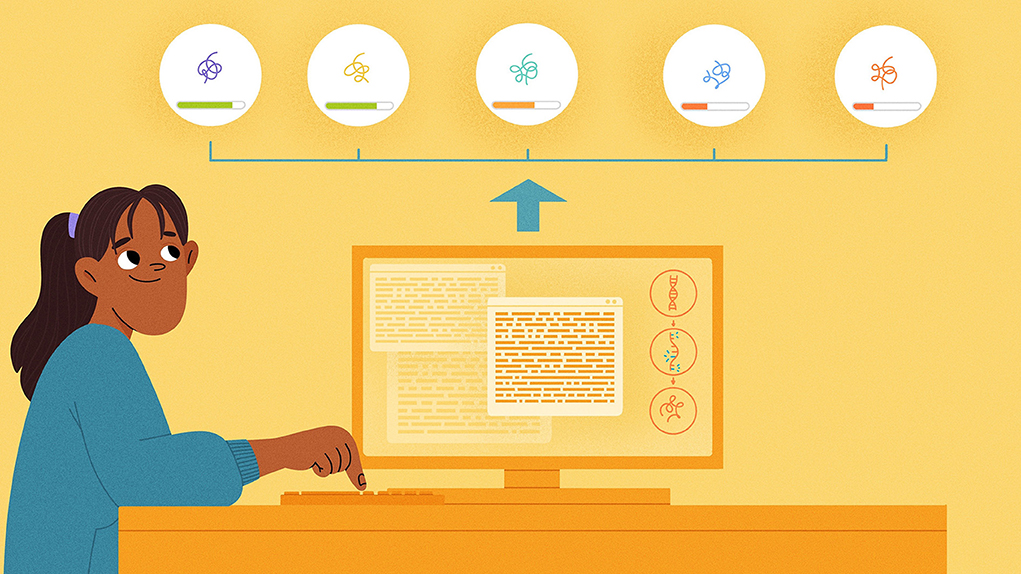
When researchers used RNA-Seq to study immune cells from hundreds of people with sepsis, they were faced with an enormous amount of data—more than they could possibly analyze without the help of computers. So, they turned to machine learning, a type of artificial intelligence that can sift through huge amounts of data to find hidden patterns (Figure 2C). Machine learning identified common genes with changed activity, enabling early diagnosis. The researchers also discovered variability between patients, identifying five main types of sepsis, which they called endotypes. Each endotype represents a unique immune system response with its own specific set of 200 genes that are either more or less active than normal, resulting in different symptoms (Figure 3) [5]. For example, RNA-Seq indicates that patients of one endotype have a type of sepsis in which the immune system is overactive, leading to excessive inflammation, while in another endotype the immune system might be suppressed (not active enough) and struggle to fight off the infection.
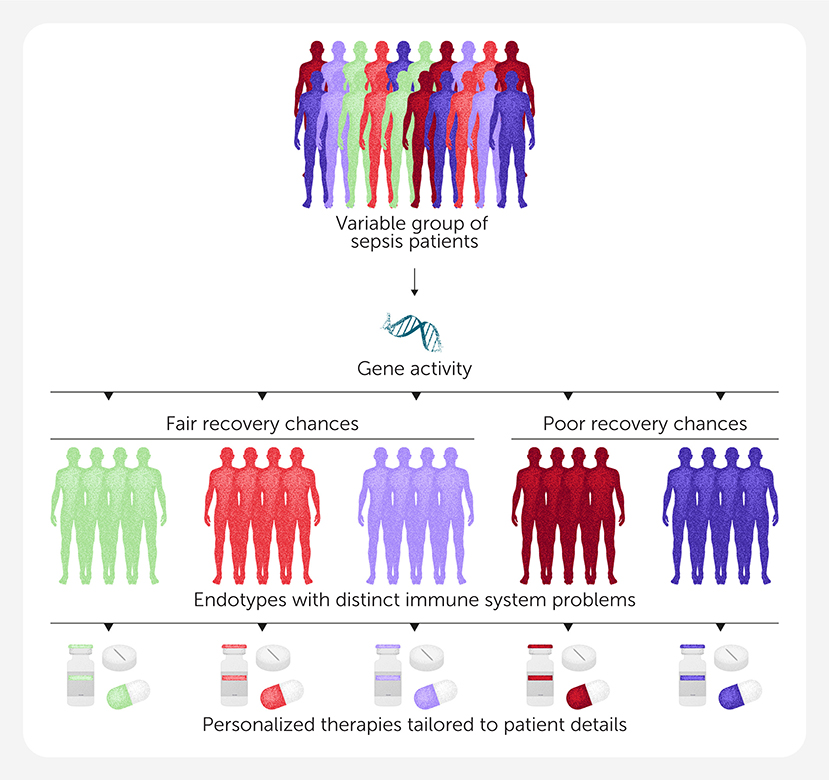
- Figure 3 - By examining gene activity using RNA-Seq, researchers could divide sepsis patients up into five main types, called endotypes.
- Each endotype is characterized by its own specific set of 200 genes that are either more or less active than normal, contributing to a unique set of immune system problems and resulting in different symptoms. The existence of sepsis endotypes allows doctors to tailor therapies specifically to the symptoms experienced by each patient, instead of using a one-size-fits-all approach.
The discovery of sepsis endotypes is exciting because they can be detected very early—sooner than doctors can usually diagnose sepsis. As mentioned, the earlier patients are diagnosed, the better their chances for recovery. Endotypes can also help to explain why some patients respond to a certain treatment while others do not. This opens the door to personalized medicine—an approach in which doctors tailor treatments to the specific details of each patient, instead of relying on a one-size-fits-all solution. Based on a patient’s gene activity, doctors may soon be able to diagnose the specific endotype of sepsis a patient has and provide the treatment that will be the most effective for their particular condition—a big step forward!
What Else Can Systems Immunology Teach Us About Sepsis?
Sepsis is not just different between patients—it also changes over time within the same patient. This means that the immune system might behave differently at different stages, as sepsis progresses. Early on, it might be hyperactive, causing excessive inflammation, but later it could become suppressed, putting the patient at risk for additional infections. These shifts in immune responses over time are another factor that currently makes sepsis difficult to treat. By using RNA-Seq, researchers can track how immune system gene activation changes over time in individual patients. Such information could lead to stage-specific treatments—therapies that are tailored not just to the endotype of sepsis a patient has, but also to whether they are in the early, middle, or late phases of the disease. More precise and effective treatments could improve patients’ chances of recovery.
Understanding what is happening to cause sepsis and how to treat it might also help doctors manage severe cases of viral infections, like COVID-19. Many researchers now believe that future pandemics could also involve some form of sepsis, regardless of the virus or bacteria involved. This means that developing therapies that target a dysfunctional immune response, rather than the specific germ, might be an important goal. If scientists can find ways to manage the immune dysfunction seen in sepsis, they could save lives in future pandemics—even before specific vaccines or treatments for the infection are available.
In the end, studying sepsis is about more than understanding a single disease—it is about solving a puzzle that could help improve health for millions of people all over the world [6]. By looking at the big picture and learning how the immune system responds to infections, researchers are not only saving lives today, but also preparing for the challenges of tomorrow.
Glossary
Immune System: ↑ A complex network of organs, cells, genes, and proteins that defend the body against infection; diseases occur when it fails or reacts inappropriately.
Dysregulated: ↑ When gene activity changes, causing the immune system to respond improperly—either overreacting, underreacting, or attacking the body itself, leading to various diseases and health issues.
Sepsis: ↑ An abnormal, life-threatening response to infection leading to (multi)organ dysfunction and failure; results from a dysregulated immune system.
Systems Immunology: ↑ A field that studies all parts of the immune system together, like genes and proteins, to see how they work and interact. Scientists use computer tools to understand these complex connections.
RNA-Seq: ↑ A method for converting RNA to DNA and then sequencing it to determine the activity of each gene in the body. Also called transcriptome sequencing.
Machine Learning: ↑ A type of AI in which computers use data and repeated calculations to imitate human thinking, improving solutions over time and handling much more information than humans can.
Endotypes: ↑ Groups of patients with similar underlying causes for a disease. Complex diseases like sepsis, cancer, and asthma have different endotypes, affecting progression, severity, and treatment effectiveness.
Personalized Medicine: ↑ Recognizing and using an individual’s specific characteristics to guide decisions made regarding the prevention, diagnosis, and treatment of disease.
Conflict of Interest
RH is the inventor on two patents covering early sepsis diagnostics (e.g., EP3117030A4) and endotypes (WO2022246553A1) respectively. These technologies have been licensed to Sepset Biosciences Inc. that is partly owned by Asep Medical Inc. and REWH is a shareholder and CEO of both companies.
Acknowledgments
Edited by Susan Debad Ph.D., graduate of the UMass Chan Medical School Morningside Graduate School of Biomedical Sciences (USA) and scientific writer/editor at SJD Consulting, LLC. We would like to thank the coauthors of the original manuscript: Andy An, Claudia C. dos Santos, and Amy H. Y. Lee. The author wishes to acknowledge funding from the Canadian Institutes for Health Research for his sepsis and systems immunology research. He currently holds a UBC Killam Professorship.
Original Source Article
↑Hancock, R. E. W., An, A., dos Santos, C. C., and Lee, A. H. Y. 2025. Deciphering sepsis: transforming diagnosis and treatment through systems immunology. Front. Sci. 2:1469417. doi: 10.3389/fsci.2024.1469417
References
[1] ↑ Rudd, K. E., Johnson, S. C., Agesa, K. M., Shackelford, K. A., Tsoi, D., Kievlan, D. R., et al. 2020. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the global burden of disease study. Lancet. 395:200–11. doi: 10.1016/S0140-6736(19)32989-7
[2] ↑ Vincent, J. L. 2021. COVID-19: It is all about sepsis. Future Microbiol. 16:131–3. doi: 10.2217/fmb-2020-0312
[3] ↑ Vincent, J.-L. 2016. The clinical challenge of sepsis identification and monitoring. PLoS Med. 13:e1002022. doi: 10.1371/journal.pmed.1002022
[4] ↑ Forlin, R., James, A., Brodin, P. 2023. Making human immune systems more interpretable through systems immunology. Trends Immunol. 44:577–584. doi: 10.1016/j.it.2023.06.005
[5] ↑ Baghela, A., Pena, O. M., Lee, A. H., Baquir, B., Falsafi, R., An, A., et al. 2022. Predicting sepsis severity at first clinical presentation: the role of endotypes and mechanistic signatures. eBioMedicine. 75:103776. doi: 10.1016/j.ebiom.2021.103776
[6] ↑ Maslove, D. M., Tang, B., Shankar-Hari, M., Lawler, P. R., Angus, D. C., Baillie, J. K., et al. 2022. Redefining critical illness. Nat. Med. 28:1141–1148. doi: 10.1038/s41591-022-01843-x