Abstract
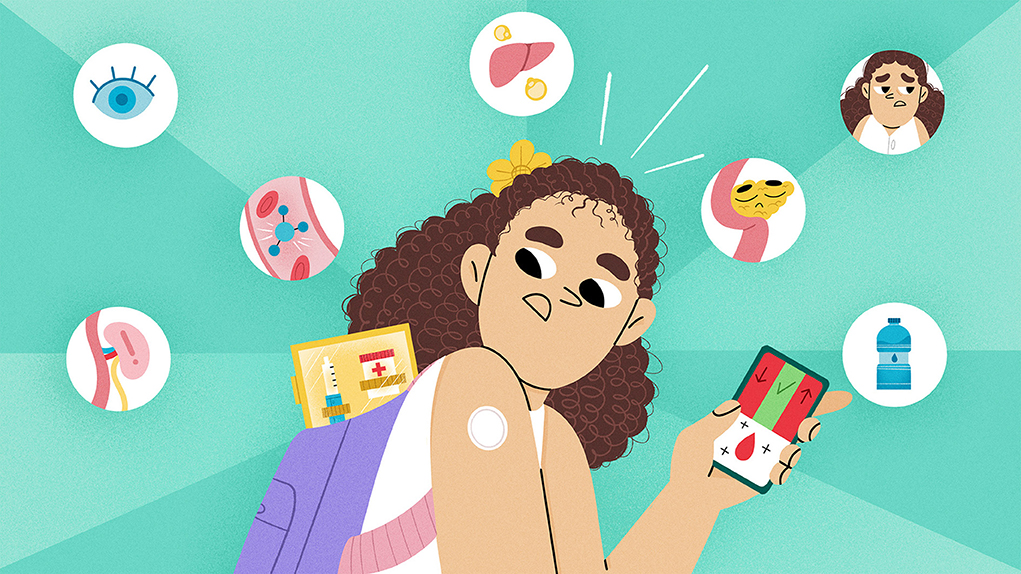
In this interactive article, we ask our young readers to approach the material like detectives to uncover the mystery of the missing insulin in the body and how this connects to type 1 diabetes. To make the learning experience more engaging, glucose, insulin, and the pancreas are introduced as story characters. Type 1 diabetes is an autoimmune disease, in which beta cells in the pancreas are destroyed by the body itself, causing little to no insulin to be produced. This is not good news for glucose, but why? We hope our readers learn about type 1 diabetes, its symptoms, and its treatment so they can better understand this condition and what it means for anyone they know who might have this condition.
Mystery Case
My name is Inspector Torres. Mr. Glucose reported that his best friend, Ms. Insulin, is missing. His work friends, called cells, are worried because they need Mr. Glucose to keep working, but without Ms. Insulin, they cannot meet. I need your detective skills to solve this mystery and keep the cells working.
Who is Mr. Glucose?
Have you ever heard of blood sugar? That is another name for Mr. Glucose. Glucose comes from carbohydrates, which are found in almost all foods with grains—like the bread in your sandwich or spaghetti. Glucose usually stays in the bloodstream or is stored in the liver. Glucose is important because it is the body’s main source of energy. Our cells use glucose for energy so that we can run, jump, draw, and even talk! Without it, our cells would turn off and stop working. Mr. Glucose uses the bloodstream as a highway to travel all over the body.
Who is Ms. Insulin?
Ms. Insulin belongs to a family of molecules called hormones. Hormones are messengers that travel in the bloodstream and tell cells what to do. Insulin is made by cells called beta cells in an organ called the pancreas. When the pancreas detects too much glucose in the blood, it tells the beta cells to make insulin. Insulin helps glucose leave the bloodstream and enter cells, where it can be used for energy. In the bloodstream, there are red blood cells whose job is to carry oxygen throughout the body. Unlike other cells, red blood cells can directly take glucose without the help of insulin. Without insulin, glucose cannot enter the cells and stays in the blood (Figure 1).
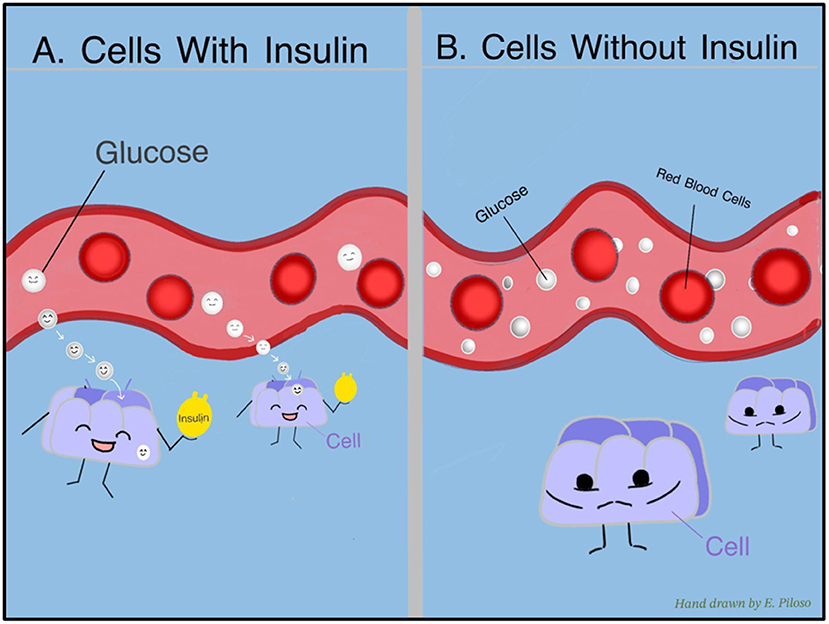
- Figure 1 - (A) Insulin connects with cells and lets glucose move from the bloodstream into the cells.
- (B) Without insulin, cells cannot let glucose in, so the cells cannot make energy, and glucose builds up in the bloodstream.
Levels of Glucose in the Body
The body requires a certain amount of glucose in the blood. When glucose is not controlled, it can cause hyperglycemia (too much sugar in the bloodstream) or hypoglycemia (too little sugar in the bloodstream) (Figure 2). Hyperglycemia can make a person extremely thirsty, weak, or have to pee a lot. Hyperglycemia happens when the pancreas does not make enough insulin, so glucose stays trapped in the bloodstream with nowhere to go. Hypoglycemia can cause a person to become hungry, shaky, tired, or have a headache. This happens when the body makes too much insulin, which causes too much glucose to leave the blood and enter the cells.
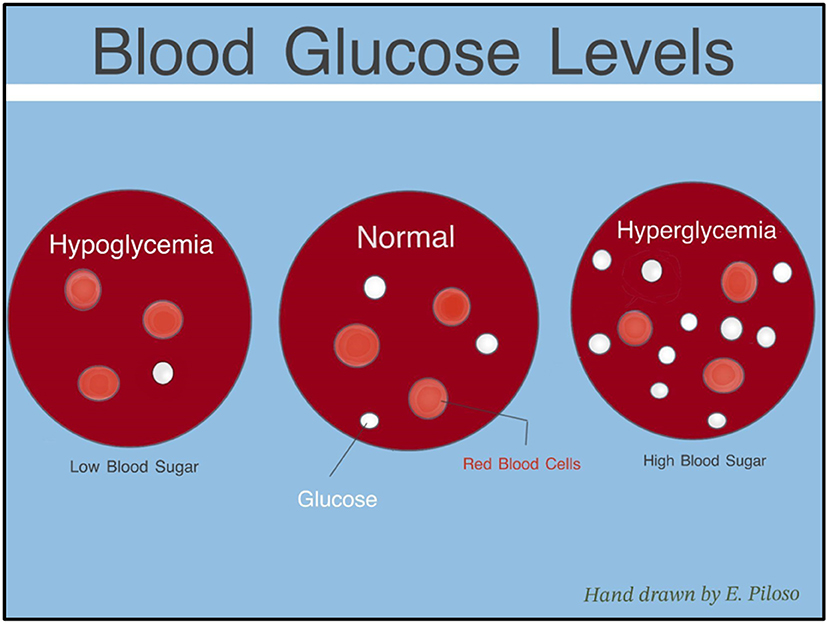
- Figure 2 - Levels of glucose in the blood need to be closely checked.
- Hyperglycemia occurs when there is too much glucose in the bloodstream. Hypoglycemia happens when there is too little glucose in the bloodstream.
What are Autoimmune Disorders?
The body’s systems work as a team to keep us healthy. The immune system is a team of cells and organs that fight harmful things like germs. The immune system searches for germs to destroy, but sometimes it gets confused and attacks healthy cells. Health problems caused by the immune system attacking the body’s healthy cells are called autoimmune disorders.
A few months ago, the immune system began destroying the beta cells in the pancreas of our subject. Sometime later, Mr. Glucose realized he could not find Ms. Insulin. Detective, could these two events be connected?
Type 1 Diabetes
Detective, one of our deputies overheard the pancreas talking about insulin being involved with type 1 diabetes. Let us do a background check on type 1 diabetes.
Type 1 diabetes, also known as T1D, is an autoimmune disorder in which the immune cells mistakenly destroy the beta cells in the pancreas. We know that the beta cells are important because they make insulin. Without beta cells, the body’s insulin decreases [1]. Scientists are working hard to understand why the immune system attacks itself, but they believe it is a mix of genes and environment [2].
Detective, do not confuse type 1 diabetes with type 2 diabetes. In type 2 diabetes, the pancreas produces some insulin, but the body cannot use it. While both types of diabetes involve problems with insulin, the key difference is that type 2 diabetes can often be prevented by eating healthy and staying active [3]. After the beta cells are attacked, loss of insulin can happen quickly or slowly [4]. When all the beta cells are gone and no insulin is made, the symptoms of diabetes begin. Symptoms are like clues the body uses to tell us something is wrong. The symptoms of type 1 diabetes include peeing too much, feeling thirsty all the time, feeling very tired, feeling hungrier than usual, and losing weight.
Sugar Watch: What is Glucose Monitoring?
Detectives: We need to keep a close eye on our subject’s blood sugar levels.
If a patient has diabetes, their doctor will monitor their blood sugar with an A1C test a few times a year, which gives the patient and the doctor an idea of how much sugar has been in the bloodstream in the last 2–3 months. Also, the person with diabetes will need to check their glucose levels throughout the day. This can be done using a finger stick test, in which the person pricks their finger with a small pointy needle device and catches a drop of blood on a test strip. The strip is inserted into a device that reads the glucose level. Glucose can also be monitored using a continuous glucose monitor (CGM), which is a small patch-like device that can be worn attached to the body for up to two weeks. It measures glucose every few minutes and can send the data to the user’s phone (to learn more about CGMs, see this Frontiers for Young Minds article).
Correcting Insulin Levels
Scientists have designed many ways to get insulin into the bloodstream where it can help move glucose into cells. The amount of insulin each person needs can change as they grow, and everyone’s treatment is unique.
There are two main types of insulin. One is called rapid-acting insulin. This is the kind of insulin people usually take before eating, to stop their sugar levels from becoming too high. Before meals, it can help the body control blood sugar for about 2–4 h [5]. The seconds type is called long-acting insulin. This is an injection taken once a day, and it helps maintain blood sugar levels constantly throughout the day [5].
What Happens if a Person With Diabetes Does Not Take Insulin?
Detective, when the body does not have enough insulin, it can act funny. Specifically, a condition called diabetic ketoacidosis (DKA) can happen when the liver uses fat for energy instead of glucose [6]. This is dangerous because burning fat quickly for energy can create ketones which makes the blood too acidic. This can damage organs like the heart and brain. DKA typically occurs when a person is sick, misses their insulin shots, or if they have an insulin pump that is not working well. Typical symptoms of DKA include being very thirsty, needing to pee more often, fruity-scented breath, weight loss, and confusion. Doctors can tell the difference between T1D and DKA by running a test to see if the patient’s urine contains a high level of ketones, which are released when the liver burns fat. If you have some of these symptoms, please talk to a parent. Detective, we need you to be healthy so that you can complete all the mysteries ahead!
Other problems can develop over time if a person with diabetes does not control their blood sugar levels (Figure 3). For example, high blood sugar can hurt a person’s kidneys and other organs and prevent the organs from working correctly [4]. The kidneys serve as a filter for the body. If they are not working, waste can build up in the blood, which is harmful to other organs.
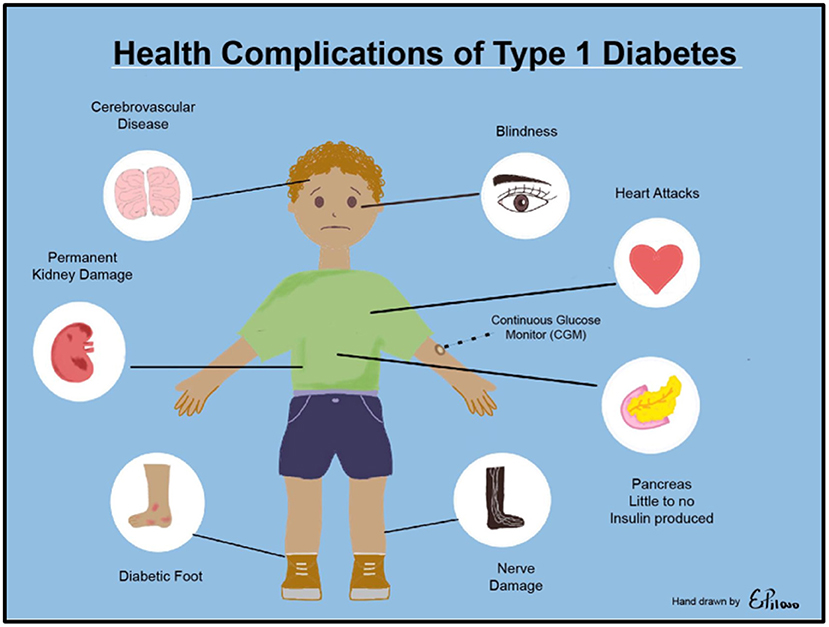
- Figure 3 - If a person’s blood sugar levels are too high, they could develop problems with their eyesight, brain, heart, nerves, feet and legs.
- This child is wearing a CGM to check glucose levels continuously.
Mission Complete: A Map to the Long-Lost Insulin
By completing this mission, we hope you have learned a lot about type 1 diabetes, so that you can now help others learn more about this condition. If you have type 1 diabetes, remember you are not alone. There are many people to help you and lots of things you can do to continue living the beautiful, fun, life of a detective. Stay healthy, continue to ask questions, and do not forget to have FUN!
Glossary
Glucose: ↑ A type of sugar that the body uses as energy.
Insulin: ↑ A hormone that lets glucose enter cells, where it is used for energy.
Hyperglycemia: ↑ High amount of glucose in the bloodstream.
Hypoglycemia: ↑ Low amount of glucose in the bloodstream.
Autoimmune Disorders: ↑ Health problems caused by the immune system attacking the body’s healthy cells.
Type 1 Diabetes (T1D): ↑ A health condition where your body does not produce insulin because beta cells are destroyed.
A1C: ↑ A blood test that checks a person’s average blood sugar level over the past 2–3 months.
Diabetic Ketoacidosis (DKA): ↑ A condition that diabetics can get if their blood sugar gets too high for too long.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Elizabeth Piloso for creating the hand-drawn illustrations used in this manuscript which are used with permission.
AI Tool Statement
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
[1] ↑ Atkinson, M. A., and Maclaren, N. K. 1994. The pathogenesis of insulin-dependent diabetes mellitus. N. Engl. J. Med. 331:1428–36. doi: 10.1056/NEJM199411243312107
[2] ↑ Rewers, M., and Ludvigsson, J. 2016. Environmental risk factors for type 1 diabetes. Lancet. 387:2340–8. doi: 10.1016/S0140-6736(16)30507-4
[3] ↑ Krause, M., and De Vito, G. 2023. Type 1 and type 2 diabetes mellitus: commonalities, differences and the importance of exercise and nutrition. Nutrients. 15:4279. doi: 10.3390/nu15194279
[4] ↑ Mittal, M., Porchezhian, P., and Kapoor, N. 2024. Honeymoon phase in type 1 diabetes mellitus: a window of opportunity for diabetes reversal? World J. Clin. Cases. 12:9–14. doi: 10.12998/wjcc.v12.i1.9
[5] ↑ Chiarelli, F., Dahl-Jørgensen, K., Kiess, W., and Kiess, W. 2005. Diabetes in childhood and adolescence. Basel. 94–96:231. doi: 10.1007/s00125-005-0081-7
[6] ↑ American Diabetes Association Professional Practice Committee. 2024. 2. Diagnosis and classification of diabetes: standards of care in diabetes–2024. Diabetes Care. 47:S20–42. doi: 10.2337/dc24-S002