Abstract
Our everyday lives depend on the cooperation of about 100 billion brain cells called neurons. Neurons are vital for every action, from breathing to moving to thinking. Regardless of the complexity and importance of the brain, it is still susceptible to diseases called neurodegenerative disorders. These terrible illnesses involve the death of neurons in particular parts of the brain. There are many neurodegenerative diseases, however, Parkinson’s disease is among the most common and causes the most severe movement problems. Although a lot has been learned about Parkinson’s disease, there is still no cure. Recently, studies have shown that small molecules found in many fruits and vegetables might help protect the brain from neurodegenerative disorders.
When the Brain Gets Sick
The human brain is an extremely complex organ made of billions of interconnected cells. This network enables us to breathe, walk, think, or feel—we depend on our brains every second of every day. If the brain is healthy, it can do all these tasks properly. But when the brain “gets sick”, people experience problems in their everyday lives. Because of the brain’s complexity, disorders can arise from very small miscommunications between brain cells called neurons. Neurodegenerative diseases are complicated illnesses that hinder the brain’s function.
Examples of neurodegenerative diseases include Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease. As for Parkinson’s disease, the number of cases in industrialized countries ranges from 10 to 18 per 100,000 people every year. Age is the biggest risk factor, but the causes are not fully understood. Only about 10% of cases have been linked to changes in specific genes, and exposure to some toxins or chemicals (particularly pesticides, herbicides, or solvents) can increase the risk of developing Parkinson’s disease.
Parkinson’s disease symptoms are mainly motor (movement) problems, such as tremors, slow movement, stiff muscles, and loss of balance and coordination. However, Parkinson’s disease can also cause memory loss, depression, hallucinations, sleep problems, and constipation, among other serious symptoms (Figure 1).
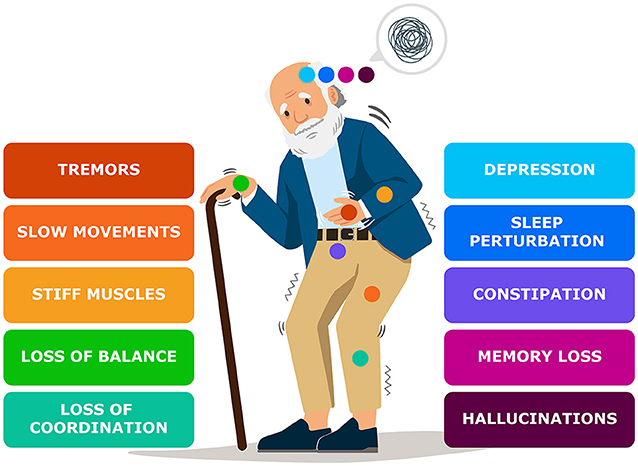
- Figure 1 - Spotting Parkinson’s symptoms.
- The most common symptoms of Parkinson’s disease can be divided into movement related symptoms (left side) or non-movement related symptoms (right side). Each colored dot represents the symptom listed in the same color and where to look for it in the body.
All people affected with Parkinson’s lose brain cells in a part of the brain called the substantia nigra pars compacta (Figure 2). It sits in the middle of the brain and is packed with cells called dopaminergic neurons. These neurons send signals to parts of the brain that control movement. It is estimated that by the time a person starts showing movement problems, 50–70% of the dopaminergic neurons in the substantia nigra pars compacta have already died.
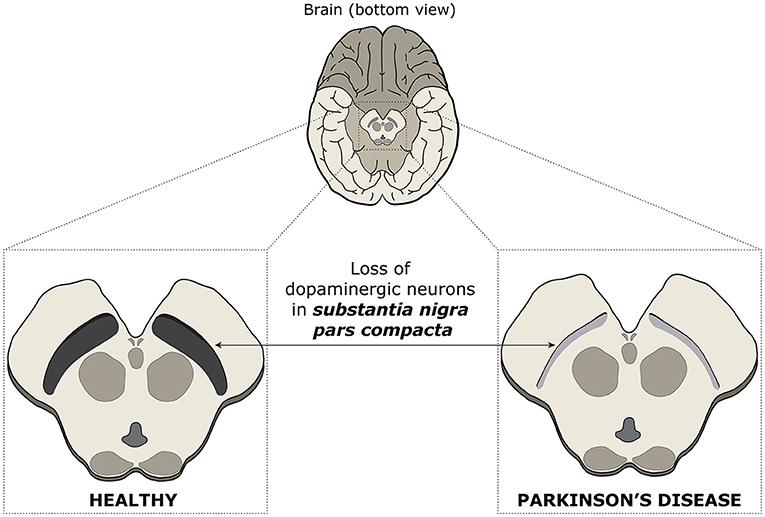
- Figure 2 - Spotting differences in healthy and Parkinson’s disease brains.
- The loss of cells called dopaminergic neurons during Parkinson’s disease can be observed in a specific region of the brain—the substantia nigra pars compacta. This small brain region is located in the midbrain, and in Parkinson’s it gets thinner and loses its characteristic dark color due to the death of dopaminergic neurons. Dopaminergic neurons from the substantia nigra pars compacta are important because they send information to other brain structures that help to regulate movement.
Features of Parkinson’s Disease
Multiple events contribute to the death of neurons in Parkinson’s disease (Figure 3). One is related to proteins—the building blocks of each cell, tissue, and organ in the body. Without these crucial molecules, the body could not function. Proteins must fold into the right shapes to work correctly. However, sometimes proteins fold incorrectly and lose their normal functions. They can also attach to each other (aggregate), which makes them toxic for cells. This is called pathological protein aggregation [1].
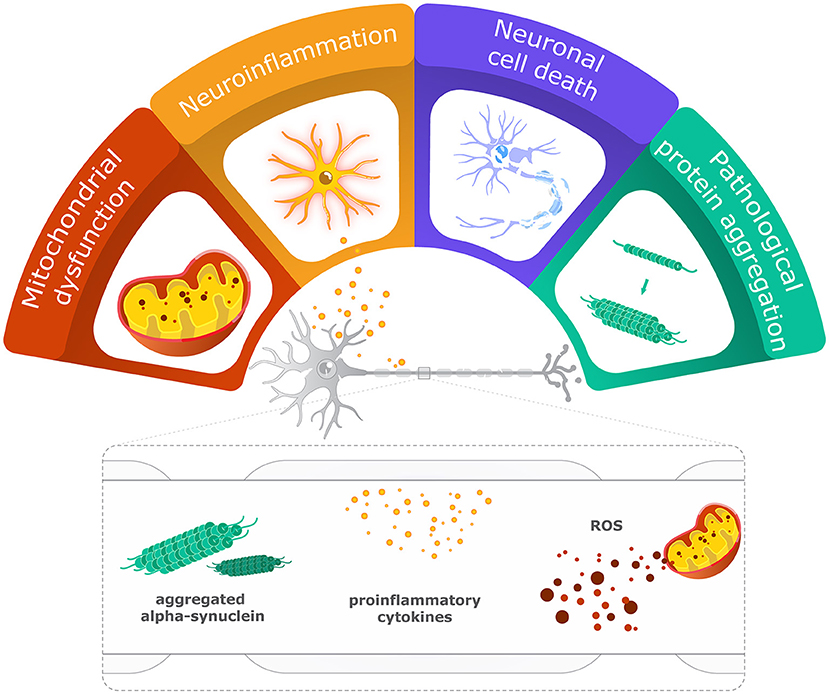
- Figure 3 - What happens inside the brain in Parkinson’s disease?
- Several problems within the brain, including issues with energy production by mitochondria, neuroinflammation, and pathological protein aggregation, can lead to the death of neurons and consequently to the development of Parkinson’s disease symptoms.
Alpha-synuclein is a protein found in neurons that regulates communication between these cells, making it essential for brain functioning. However, when alpha-synuclein aggregates, it makes the neurons sick, causing their death [2].
Problems at the Powerhouse
Another problem in Parkinson’s disease involves producing enough energy for normal brain functioning [1, 3]. Energy comes from mitochondria—structures within cells that break down nutrients to produce energy. Every cell has a different number of mitochondria. Since dopaminergic neurons in the substantia nigra pars compacta are highly active cells, they need a lot of mitochondria. In the brains of people with Parkinson’s disease, mitochondria change their form and function. So, instead of producing energy, they start producing toxic molecules that affect numerous cellular processes, ultimately causing cell death [3].
When a Friend Becomes a Foe
Although neurons are the most important cells in the brain, they are not alone. There is an entire class of cells called glial cells that are usually the keepers of brain health and function. There are several types of glial cells, but the most affected in Parkinson’s disease are microglia and astrocytes [1].
Microglia are natural immune cells of the brain that work very hard to protect us from sickness. When there is no threat, microglia are just doing surveillance. However, when something attacks the brain, like bacteria or toxic proteins, these cells become active and start releasing molecules that can cause neuroinflammation, in which the brain’s immune cells get activated to fight off the invaders or repair damage. If neuroinflammation is temporary, it helps the brain to remove the threat. However, if it lasts longer, as in Parkinson’s disease, neuroinflammation becomes toxic for the brain, causing damage and death of neurons [4].
Microglia also closely interacts with astrocytes. In a healthy brain, astrocytes provide nutrients to neurons, maintain a healthy brain environment, and provide structural support. In Parkinson’s disease, however, astrocytes do not function properly, and they start releasing substances that lead to neuroinflammation.
It is not hard to imagine how difficult Parkinson’s disease can be for neurons. With multiple problems happening at the same time, including abnormal alpha-synuclein, thousands of dysfunctional mitochondria, and overactivated microglia and astrocytes, the neurons in the substantia nigra pars compacta suffer the most and start dying [1].
Cure, Please!
Although scientists have learned a lot about Parkinson’s disease over the years, there is much more to discover to find a cure. The therapies developed so far can help patients with their movement disorders, but these therapies have harsh side effects when used for a long time. Current therapies also do not help with pathological protein aggregation, neuroinflammation, or mitochondria dysfunction. Since these processes cause the movement problems seen in Parkinson’s disease patients, it is really important to find a cure that can affect these processes. That is why scientists are trying to find new therapies that are better and safer. Luckily, more and more scientific evidence is showing that there is a class of natural molecules that can help protect the brain from the changes that lead to Parkinson’s disease.
Food Shield
Have you heard the saying “you are what you eat”? Well, studies show that food can help when it comes to neurodegenerative diseases like Parkinson’s. One class of nutrients in foods is called polyphenols. Polyphenols are present in fruits, vegetables, cocoa, tea, and coffee, among others. When polyphenols are digested by the normal bacteria in the gut, their chemical structure changes and they become polyphenol metabolites. Polyphenol metabolites can then cross the intestinal barrier, reach the blood circulation, and reach various organs in the body, including the brain.
Polyphenol metabolites can have positive effects on blocking or dampening dangerous inflammation. They can also improve mitochondrial function [5]. Some polyphenol molecules also seem to be able to slow down or prevent the incorrect folding and aggregation of alpha synuclein [6]. Overall, polyphenols seem to work in various ways to protect brain cells and reduce the death of neurons. Recent studies have shown that an everyday diet rich in polyphenols from fruits can postpone and ease most of the pathological features of Parkinson’s disease [7].
However, most of the results showing how polyphenols affect Parkinson’s disease come from studies done in animals. While these studies show great possibilities of polyphenols, there are still no studies done on humans with Parkinson’s disease. Therefore, more studies are needed to explore the effects of polyphenol metabolites on the human brain. Some very recent studies done in humans with other types of diseases are showing that polyphenol-rich foods are very powerful in reducing neuroinflammation and mitochondria problems [8]. This is very good news, as these processes also play important roles in Parkinson’s disease. We hope that, in the near future, studies will be done involving people with Parkinson’s to test how a polyphenol-rich diet affects the progression of the disease. For now, scientists are still busy unraveling the multitude of effects polyphenol metabolites have on the brain. While much of this work is still at very early stages, initial evidence has scientists excited about the future.
Glossary
Neurons: ↑ Special cells in the brain and nervous system that send and receive messages to help you think, speak, feel, and move.
Neurodegenerative Diseases: ↑ Illnesses that affect the neurons, preventing the brain from working properly.
Dopaminergic Neurons: ↑ Special neurons that release dopamine, a chemical that helps control movement, mood, and feelings of reward.
Pathological Protein Aggregation: ↑ When proteins with an abnormal shape stick together in clumps, which makes them toxic to cells.
Alpha-synuclein: ↑ The main protein that gets folded incorrectly in Parkinson’s disease.
Brain Glial Cells: ↑ Cells in the brain that support and protect neurons, keeping the brain healthy and functioning well.
Neuroinflammation: ↑ When the brain’s immune cells become active to fight off threats, but if this goes on too long, it can harm the brain.
Polyphenols: ↑ A type of compounds found in healthy foods and drinks, like fruits, vegetables, natural fruit juices, and tea. They are broken down in the gut to become polyphenol metabolites.
Conflict of Interest
AR, CP, IS, CS, and NL-V were employed by iNOVA4Health. IS and CS were employed by iBET.
Acknowledgments
To European Research Council (ERC), Grant no. 804229; to iNOVA4Health (LISBOA-01-0145-FEDER-007344; UIDB/04462/2020) by Fundação para a Ciência e Tecnologia (FCT)/Ministério da Ciência e do Ensino Superior (MCTES), through national funds, and by FEDER under the PT2020 Partnership Agreement. To FCT for financial support of CP (2023.00453.BD) and of IS (2023.02417.BD).
References
[1] ↑ Wilson, D. M., Cookson, M. R., Van Den Bosch, L., Zetterberg, H., Holtzman, D. M., Dewachter, I., et al. 2023. Hallmarks of neurodegenerative diseases. Cell 186:693–714. doi: 10.1016/j.cell.2022.12.032
[2] ↑ Srinivasan, E., Chandrasekhar, G., Chandrasekar, P., Anbarasu, K., Vickram, A. S., Karunakaran, R., et al. 2021. Alpha-synuclein aggregation in Parkinson’s disease. Front. Med. 8:736978. doi: 10.3389/fmed.2021.736978
[3] ↑ Murali Mahadevan, H., Hashemiaghdam, A., Ashrafi, G., and Harbauer, A. B. (2021). Mitochondria in neuronal health: from energy metabolism to Parkinson’s disease. Adv. Biol. 5:2100663. doi: 10.1002/adbi.202100663
[4] ↑ Troncoso-Escudero, P., Parra, A., Nassif, M., and Vidal, R. L. 2018. Outside in: unraveling the role of neuroinflammation in the progression of Parkinson’s disease. Front. Neurol. 9:860. doi: 10.3389/fneur.2018.00860
[5] ↑ Yan, L., Guo, M.-S., Zhang, Y., Yu, L., Wu, J.-M., Tang, Y., et al. 2022. Dietary plant polyphenols as the potential drugs in neurodegenerative diseases: current evidence, advances, and opportunities. Oxid. Med. Cell Longev. 2022:5288698. doi: 10.1155/2022/5288698
[6] ↑ Loncarevic-Vasiljkovic, N., and Carregosa, D. Nunes dos Santos C. 2022. Chapter 8. Neuroprotective Mechanisms of Berry Bioavailable Polyphenol Metabolites. London: Royal Society of Chemistry. p. 208–45.
[7] ↑ D'Amico, R., Impellizzeri, D., Genovese, T., Fusco, R., Peritore, A. F., Crupi, R., et al. 2022. Açai berry mitigates Parkinson’s disease progression showing dopaminergic neuroprotection via Nrf2-HO1 Pathways. Mol. Neurobiol. 59:6519–33. doi: 10.1007/s12035-022-02982-5
[8] ↑ GrabeŽ, M., Škrbić, R., Stojiljković, M. P., Vučić, V., Rudić Grujić, V., Jakovljević, V., et al. 2022. A prospective, randomized, double-blind, placebo-controlled trial of polyphenols on the outcomes of inflammatory factors and oxidative stress in patients with type 2 diabetes mellitus. Random. Controll. Trial. Rev. Cardiovasc. Med. 23:57. doi: 10.31083/j.rcm2302057
