Abstract
People with severe brain damage can suffer from a disorder of consciousness (DoC) such as a coma. They may be unconscious for decades, with little or no awareness of themselves or their surroundings, or they might emerge slowly into consciousness. People with DoCs usually cannot control any of their movements to respond to questions, so diagnosing them is difficult. However, methods of looking at brain activity are helping us learn more about each patient’s remaining abilities and thus choose the best treatments. Treatments including physical therapy, rehabilitation, medications, music therapy, and brain stimulation can increase patients’ brain function and sometimes help them recover communication or other behaviors. Nurses and physical therapists are generally needed to help reduce patients’ pain and other discomfort. DoCs can strongly impact patients and their families, but many groups provide support. Research scientists and doctors also help by finding new ways to understand consciousness in general and treat DoCs.
What is a Disorder of Consciousness?
What happens when something hits your head? You might get a cut, bruise, or a bump that goes away after several days. Your brain will probably be OK, since it is well protected by your skull. But what happens when you injure your brain? Severe brain damage from outside causes (like a severe blow to the head or other traumatic brain injury), or from within the brain (like a stroke or problems with drugs or medications) can lead to a disorder of consciousness (DoC) that starts as a coma. People who are comatose are unconscious and do not feel pain. Their eyes are closed and they look like they are asleep. They cannot make their bodies move, although they may have automatic movements such as spasms or tremors. People in comas do not show any awareness of their surroundings, they do not think about anything, and they cannot be woken up.
Some people in comas die after several days or weeks. Others will quickly improve and need rehabilitation to fully recover. Other patients will open their eyes after a while, but still be unable to talk or communicate with their families and friends. This is called unresponsive wakefulness syndrome (UWS) [1] because they do not respond to simple questions (Click here for more). Some patients recover a low level of consciousness and can respond to things happening in their environment. For example, they can follow people with their eyes, but they still cannot communicate otherwise. They are said to be in a minimally conscious state (MCS). People may live in the same state for a very long time (up to decades), which is called a prolonged DoC. A few patients emerge from DoCs fully conscious but paralyzed, which is called locked-in syndrome (LIS). They might be able to communicate “yes” or “no” by making small eye blinks or other movements to respond to questions, or they might be able to use a brain-computer interface (BCI). Figure 1 summarizes LIS and the three types of DoCs.
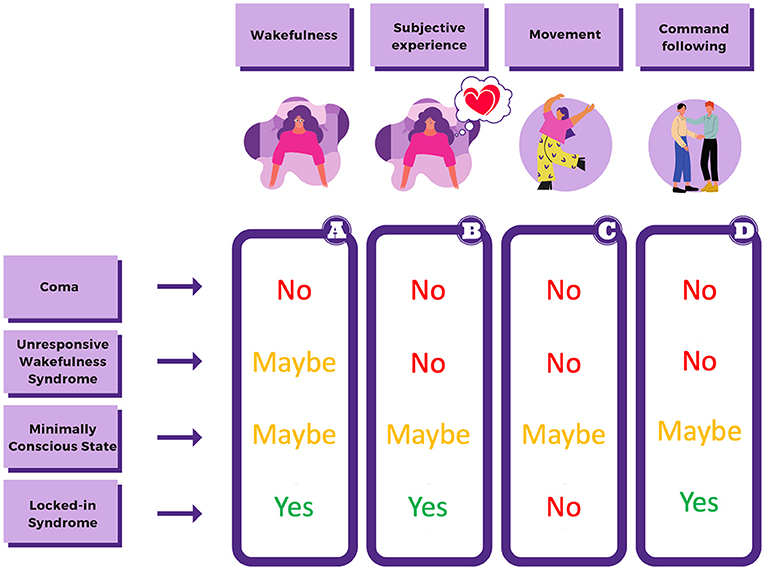
- Figure 1 - LIS and three types of DoCs (coma; UWS, and MCS) have similarities and differences.
- This figure shows whether patients with each condition have: (A) periods of time with eyes open, which indicates wakefulness; (B) awareness of themselves and their environment, called subjective experience; (C) voluntary (on purpose) body movements; and (D) the ability to follow instructions. Most people with LIS are mentally able to follow commands, but only through limited movements such as blinking or moving a finger.
Diagnosing DoCs with Movements and Behavior
To help patients recover, medical teams and families must make informed decisions about treatment. Therefore, they need to understand the amount and nature of conscious activity in each patient. Medical teams diagnose consciousness with behavioral scales such as the Coma Recovery Scale-Revised (CRS-R). This scale uses 23 different behavioral tests to assess how well each patient can hear, see, move, talk, communicate, and respond to things in their environment. More precisely, doctors ask patients to perform several movements, such as shaking hands, blinking, and sticking out their tongues. Patients who can move and respond to these instructions are probably in MCS or better. A patient with UWS will not be able to perform any of the movements they are asked and will only show automatic reflexes (such as the startle reflex, which refers to automatically closing the eyes after a loud noise).
Diagnosing DoCs with Brain Imaging
Imagine that you are dreaming vividly, but you do not move at all. How would anyone know anything about your dream or other mental experiences? Doctors and scientists can try to learn more about a person’s conscious experiences using brain imaging and electrodes tools, which are devices and methods to measure and understand brain activity. Recently, guidelines for the care of people with DoCs have recognized the need for better ways to diagnose them, and these guidelines recommend that brain imaging techniques be used alongside behavioral tests [2]. These techniques can help doctors learn whether people can hear, feel, understand speech, follow commands, make choices, and other mental tasks.
The fluorodeoxyglucose positron emission tomography (FDG-PET) scanner is a brain imaging tool that shows how specific areas of the brain use a type of sugar called glucose. Active neurons (brain cells) use more glucose, so networks of neurons working together in the brain use more glucose when they are supporting mental activities, including consciousness. Two networks of brain activity are related to two types of consciousness: one network for self-awareness and the other for awareness of the environment. Self-awareness is everything that relates to oneself—that inner voice that tells you “I have to tidy up my room”. To generate thoughts like these, we need enough activity in the blue areas of Figure 2. Awareness of the environment is everything that has to do with perception—the experiences generated by the five senses. This type of awareness involves the external network of consciousness, in red in Figure 2.
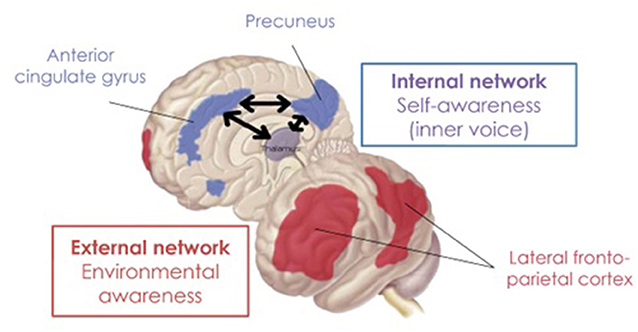
- Figure 2 - The front image shows the brain as if you were looking through someone’s left ear.
- The image in the back shows the brain section you would get when drawing an imaginary line from the tip of one’s nose to the spine. The blue areas form a network (indicated with black arrows) of regions working together for self-awareness—thoughts about yourself or things you do. The red areas manage environmental awareness. In coma or UWS, the activity of both networks is (almost) absent. In MCS, the activity is partially preserved. In LIS, both networks work like in healthy people.
When doctors use the activity in these brain areas to measure consciousness, up to two-thirds of UWS patients might actually be conscious, even if they do not show conscious behaviors. Many of these patients (who were diagnosed incorrectly based on behavior only) actually recover signs of consciousness later. Of course, not all patients with DoCs can get an FDG-PET scan, since this is a very expensive and specialized exam, and there are not many FDG-PET scanners.
There are many other ways to measure brain function. The brain’s electrical activity can be measured by electroencephalography (EEG), which is relatively portable, inexpensive, and easy to use. The patient wears an electrode cap, which looks like a swimming cap with many brain imaging and electrodes that measure the brain’s electrical activity. Electrical activity changes whenever a person sees, hears, moves, thinks or performs other mental activities. EEGs can help doctors determine how the brain is working, including after brain injury. EEG-based tools based on brain computer interfaces (BCIs) can help some individuals with LIS or DoCs show us they are conscious and even help them to communicate, just by performing mental activities like counting the vibrations they feel on the wrist. For more information about how to diagnose and even interact with people with DoC using BCIs and other tools (Click here for more).
Treatment Options
Figure 3 shows various treatments that can help people with DoCs respond better and become healthier overall [3]. These methods need to target brain areas and networks that are important for consciousness, so a lot of research focuses on identifying these brain areas. Rehabilitation is important, including physical and speech therapy or sensory stimulation. Sensory stimulation may include sounds (such as music or a family member’s voice), pictures or lights, smells such as their favorite perfume, tactile stimuli like a pleasant touch, and taste stimuli like something sweet. Some medications such as amantadine and apomorphine are also used to help patients with DoCs to recover. Amantadine can help patients become and remain more awake. Apomorphine is a relatively new therapy and its efficacy is still being tested, but it seems that it can increase the level of awareness. Psychedelics are another type of medication under investigation. Psychedelic (which means “mind-revealing”) drugs might restore “wakefulness-like” brain activity in patients with DoC, making them more aware. Music therapy is another option and might help engage patients to interact with the environment. Some groups are studying brain stimulation to help patients with DoCs by stimulating the brain from either the outside or the inside of the skull. Most brain stimulation requires electric or magnetic fields, but other options include infrared light, shockwaves, or ultrasound waves. EEGs and other methods can also help predict whether and how patients might improve over months or years.
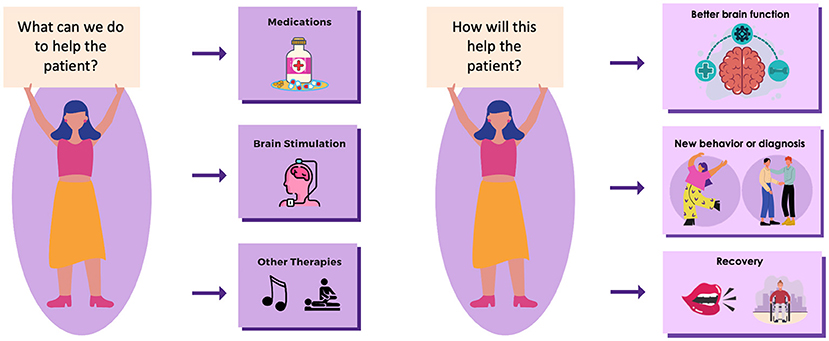
- Figure 3 - People with DoCs have several treatment options.
- Medications can sometimes help. Brain stimulation can be used, in which electrodes worn on the head send a weak electrical current to the brain networks important for consciousness. Other options include rehabilitation or music therapy. The aim of these treatments is to help patients be more conscious by increasing their brain activity. With treatment, patients may perform new behaviors, get a different diagnosis, or even recover the ability to speak and/or use tools like a wheelchair.
The effects of treatment vary. Sometimes patients are more awake after treatment and suffer less from drowsiness. Other treatments change brain activity to resemble more healthy patterns. Patients responding to brain stimulation might show some new behaviors that they never showed before the start of the treatment. With some rare and still somewhat experimental treatment options, a very small percentage of patients (about 5%) show a remarkable recovery and can communicate or even walk again. More often, no changes are observed, but treatment is still worth trying.
Other Ways to Help Patients and Families
Caring for patients with DoCs requires a lot of time and money. They need help just to stay alive. They need machines to help them eat, drink, and breathe. They must live somewhere with a medical expert who can respond quickly if anything goes wrong. They may live with family at home, but more often live in hospitals, nursing homes, or other specialized care centers. Nurses must wash and shampoo them, provide medication, move them on their beds so they do not get bedsores from being in the same position for too long, and provide other care. Physical therapists may provide therapy to reduce tremors, spasms, muscle pain, and other causes of discomfort.
DoCs do not just affect the patients. Friends and family cannot work, play, or even chat with DoC patients. Sometimes people who know the patient will not visit because they think the patient cannot understand them—even though this may be incorrect. Many families and patients have reported feeling powerless, alone, and misunderstood as they try to cope with DoCs. People may need help deciding where the patient should live, which doctors and medical treatments to use, how patients might improve after (or without) various types of treatment, how to get support, and numerous other details.
Fortunately, many groups and resources exist to help people learn more and meet others with similar challenges. For example, the MindCare International Foundation is a non-profit organization that provides information and support to patients and their families after mild to severe head injury. They organize conferences, research activities, “healthy mind” activities like meditation and support meetings, and networks of people who can share information, provide advice, or just give emotional support.
Conclusion
DoCs are rare medical conditions that include coma and varying levels of reduced consciousness. Correctly diagnosing DoC patients can be challenging, but incorrect diagnoses can be avoided by combining behavioral and brain imaging techniques. Several treatment options are being developed to help increase consciousness in DoC patients, but much work still needs to be done. Patients’ families might experience much uncertainty, and caregivers should not forget about them.
Doctors, scientists, engineers, therapists, psychologists, and other experts continue exploring new ways to help patients and understand consciousness. This work often requires teams of people with different skills, including neuroscience, psychology, medicine, engineering, programming, mathematics, and communications. If you are interested in this field, you could be part of the team that develops the next breakthrough for improved diagnosis, communication, treatment, care, prediction, or support—all while helping people learn more about consciousness in all of us.
Glossary
Disorder of Consciousness (DoC): ↑ A condition resulting from severe brain damage in which patients show little or no arousal nor awareness. DoCs include coma, unresponsive wakefulness syndrome (UWS), and minimally conscious state (MCS).
Coma: ↑ A type of DoC which can occur acutely after severe brain injury in which patients are unable to wake up and unaware of their environments. They are not conscious and don’t respond to stimuli like talking or touching.
Rehabilitation: ↑ Methods like stretching, massaging, and moving patients can help them recover from injuries, improve motor function, and reduce pain and discomfort.
Unresponsive Wakefulness Syndrome (UWS): ↑ In this DoC, patients’ eyes are open but they don’t respond to questions. Even if these patients have open eyes, they are as unaware as patients in a coma.
Minimally Conscious State (MCS): ↑ A type of DoC in which patients may show limited responsiveness and respond to some stimuli.
Locked-In Syndrome (LIS): ↑ A condition in which patients are conscious but cannot reliably control their movements. Diagnosing these patients is difficult since they cannot respond to most commands.
Brain-Computer Interface (BCI): ↑ A system that directly measures brain activity and translates it into signals that help a patient communicate. BCI methods can be used to help people with DoCs and LIS.
Brain Imaging: ↑ Technologies to learn about the brain's structure and function. Many brain imaging systems use electrodes outside the head (like EEG) or inside the head.
Electrodes: ↑ Sensors that measure the brain's electrical activity. Electrodes might be placed in an electrode cap to measure EEG or on the brain's surface during brain surgery.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to thank Arnaud Arseni for artwork with the figures and Melanie Fried-Oken for her insight on an earlier version of this manuscript. PC is research fellow and SL is research director at FRS-FNRS. JA is postdoctoral fellow funded (1265522N) by the Fund for Scientific Research-Flanders (FWO). The study was further supported by the University and University Hospital of Liège, GIGA Doctoral School for Health Science, the BIAL Foundation, the Belgian National Funds for Scientific Research (FRS-FNRS), the European Union’s Horizon 2020 Framework Programme for Research and Innovation under the Specific Grant Agreement No. 945539 (Human Brain Project SGA3), the FNRS PDR project (T.0134.21), the ERA-Net FLAG-ERA JTC2021 project ModelDXConsciousness (Human Brain Project Partnering Project), the fund Generet, the King Baudouin Foundation, the Télévie Foundation, the European Space Agency (ESA) and the Belgian Federal Science Policy Office (BELSPO) in the framework of the PRODEX Programme, the Public Utility Foundation ‘Université Européenne du Travail’, “Fondazione Europea di Ricerca Biomedica”, the BIAL Foundation, the Mind Science Foundation, the European Commission, the Fondation Leon Fredericq, the Mind-Care foundation, the DOCMA project (EU-H2020-MSCA-RISE-778234), the National Natural Science Foundation of China (Joint Research Project 81471100), and the European Foundation of Biomedical Research FERB Onlus.
References
[1] ↑ Laureys, S., Celesia, G. G., Cohadon, F., Lavrijsen, J., León-Carrión, J., Sannita, W. G., et al., 2010. Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med. 8:1–4. doi: 10.1186/1741-7015-8-68
[2] ↑ Giacino, J. T., Katz, D. I., Schiff, N. D., Whyte, J., Ashman, E. J., Ashwal, S., et al., 2018. Practice guideline update recommendations summary: disorders of consciousness: report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology; the American congress of rehabilitation medicine; and the national institute on disability, independent living, and rehabilitation research. Arch. Phys. Med. Rehabilit. 99:1699–1709. doi: 10.1212/WNL.0000000000005926
[3] ↑ Thibaut, A., Schiff, N., Giacino, J., Laureys, S., Gosseries, O. 2019. Therapeutic interventions in patients with prolonged disorders of consciousness. Lancet Neurol. 18:600–14. doi: 10.1016/S1474-4422(19)30031-6
