Abstract
Proper brain functioning is responsible for our feelings, behavior, and thinking. However, an injury to the brain can disrupt brain function, which can affect our emotions and behaviors. A traumatic brain injury (TBI) can be a one-time severe injury to the brain, or repeated, milder injuries. Scientists have observed that, after TBI, people are frequently sad and have difficulty concentrating. These symptoms are referred to as post-traumatic depression (PTD). PTD can affect school performance and daily activities. It is therefore important to notice any signs of PTD. If signs of PTD are present, individuals should seek help from a professional. PTD is treatable and, with adequate treatment, individuals with PTD can gradually recover their normal functioning.
What Is Traumatic Brain Injury?
Traumatic brain injury (TBI) happens frequently to people of all ages worldwide. TBI results from a blow to the head, for example when a child hits his head after falling off a bike. During a TBI, the brain’s function is affected depending on the severity of the injury.
Not all brain injuries are the same. The severity of a TBI can be rated as mild, moderate, severe, or penetrating. The above example of a child falling off his bike and hitting his head is an example of a mild TBI. Penetrating TBI occurs when a bullet hits the head of a soldier at war, for example. Moderate and severe TBI fall in between these two examples. However, even the mildest brain injury (also called a concussion) can affect brain cells. Concussions are the most common type of TBI (Figure 1), and they can cause short-term changes in brain functions including the ability to think clearly. On the other hand, severe brain injuries usually lead to more serious long-term health problems, such memory loss or inability to walk or talk properly.
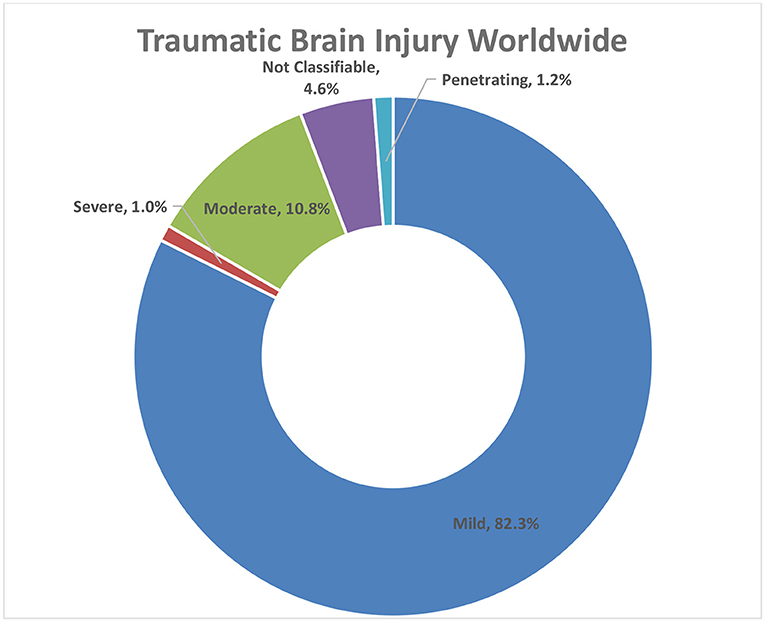
- Figure 1 - Worldwide percentages of TBI in 2000–2021.
- “Not classifiable” TBI includes TBI cases for which not enough information is available to classify them [2].
The duration of confusion and loss of memory are two of the major criteria used to classify the type of TBI a patient is suffering from. In mild TBI, confusion or memory loss last <24 h, and the brain appears normal. In moderate TBI, confusion lasts more than 24 hours, memory loss lasts more than 24 h but <7 days, and the brain appears abnormal. In severe TBI, confusion lasts more than 24 h and memory loss lasts more than 7 days. Finally, in penetrating TBI, there is an injury that causes the skull to open and harms the brain [1].
What Are the Major Causes of TBI?
TBI is very common and can be caused by a variety of factors. Around the world, about 69 million individuals suffer from TBI each year [3]. Common causes of TBI include falls, bumping into objects, car accidents, and violent physical activity. TBI causes vary between countries. For instance, falls are the most common cause of TBI in the U.S.A. (Figure 2), as well as in central and eastern Europe, Latin America, Asia, and most parts of Africa [4]. Contact sports, like ice hockey, American football, soccer, rugby, wrestling, and boxing are also major causes of TBI. Micheal Schumacher is a famous German car-racing champion who has won many Formula One races. In 2013, Michael fell while skiing with his son and hit his head on a rock. The hit resulted in severe TBI and, according to doctors, his helmet was the reason he did not die. Michael was in a coma for several months. Now, he cannot walk and needs a wheel chair, and he has problems speaking and remembering things.
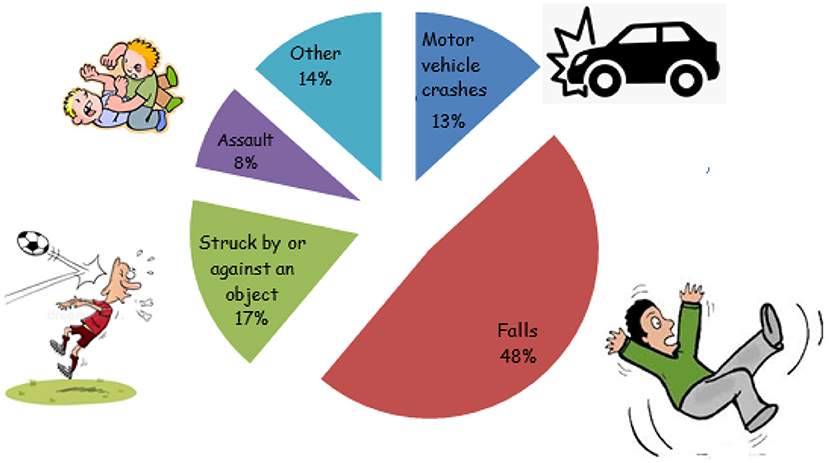
- Figure 2 - Major causes of TBI in the U.S. according to data from 2014.
- Falls make up almost half of the reported cases of TBI [5].
What Can Happen After a TBI?
Depending on the severity of the TBI, complications can last for a few days, or for months or years. In mild to moderate cases, there are four major categories of symptoms: memory/brain function, physical, emotional, and sleep (explained in Table 1). However, in the worst cases, when a TBI is very severe, it can lead to death. Emotional problems are among the most common and persistent complications that follow TBI. These problems include depression (sadness), anger, and aggression [6].
| Memory/brain function | Physical | Emotional | Sleep |
|---|---|---|---|
| Difficulty thinking clearly | Feeling tired or having no energy | Nervousness or anxiety | Sleeping more or less than usual |
| Difficulty concentrating | Headache, dizziness, sensitivity to noise or light, problems in balance, blurry vision | Sadness | Trouble falling asleep |
| Difficulty remembering new information | Nausea or vomiting | Irritability | Trouble maintaining sleep |
- Table 1 - Four main categories of symptoms following TBI.
TBI Changes How People Feel
After TBI, a person may feel sad most of the time and may experience a loss of interest in hobbies or a loss of pleasure in things that used to be enjoyable. People may not enjoy socializing and prefer to be alone. These emotion and mood changes are symptoms of depression. Depression that takes place after TBI is referred to as post-traumatic depression (PTD). Depression and PTD have similar symptoms, but they differ in the underlying causes. Depression is considered a mental disorder that can be caused by several factors including abnormalities in brain chemicals called neurotransmitters. On the other hand, PTD is depression that develops due to a hit on the head.
There are some signs that help differentiate between the two types of depression. Depression often comes with a feeling of guilt, meaning that the depressed person feels like they did something wrong and they feel bad about it—even though they did not really do anything wrong. In contrast, PTD is not usually associated with feelings of guilt. Also, PTD is sometimes accompanied by stress or anger. This is why individuals with TBI may become violent for seemingly no reason [7]. People with PTD may also feel tired and can have trouble getting good sleep, or they may sleep more or less than usual. PTD also affects attention. After a TBI, people usually have poor attention and concentration. They have difficulty focusing on tasks without being distracted, which can result in poor performance at school and can affect daily activities.
People are especially prone to being sad and having PTD during the first year after injury. Several factors may contribute to the development of PTD. For example, people are more likely to develop PTD if they already feel depressed before they experience TBI. People who do not get proper support from their families and friends also have a higher chance of PTD. Also, PTD happens more frequently in females [8].
Dealing With Depression After TBI
If a patient with TBI has any signs of depression, it is very important that they seek professional help. Psychotherapy and lifestyle changes are usually attempted first. This involves seeing a counselor to work on improving thoughts and behaviors. A healthy lifestyle, including regular exercise and a balanced diet low in junk food, has been shown to improve signs of PTD [9]. However, if a TBI results in physical disabilities, exercise should be done under the supervision of a professional. Techniques that improve wellbeing, like yoga and meditation, can also be helpful.
Sometimes, a doctor might also recommend antidepressants. An antidepressant is a medication that works to balance the neurotransmitters in the brain, to decrease the signs of depression. Antidepressants are not addictive and do not have to be taken forever—they can be taken until the patient feels better, and then stopped.
It is important to keep in mind that depression can be treated. People who feel depressed should avoid isolation and seek professional help. With proper help and family support, depression sufferers can gradually improve and start enjoying their regular activities again.
Conclusion
TBI affects people of all ages, all around the world. Depending on the severity of the injury, the consequences can last for days, months, or years. TBI can alter how people act and feel and can predispose people to depression, stress, and anger. Depression is characterized by a persistent feeling of sadness and an inability to enjoy daily activities, frequently accompanied by decreased attention and concentration, resulting in poor performance at school. However, PTD is treatable and individuals with signs of PTD should seek care from a professional and seek support from their families.
Always remember that even if TBI lasts for a short time, its effects can remain much longer. The best way to prevent the long-term effects of TBI is to prevent TBI from happening in the first place! So, stay safe—always wear a seat belt when in a car and a helmet when biking, skiing, or playing contact sports.
Glossary
Traumatic Brain Injury: ↑ Broad term that refers to several type of injuries that can happen to the brain. This includes hitting the head or piercing the skull with an object and damging the brain tissue.
Concussion: ↑ Type of traumatic brain injury that is mild. It is caused by a hit to the body or the brain causing a rapid move of the head back and forth. This movement can result in a damage to the brain cells.
Depression: ↑ A mood disorder in which the patient has a continuous feeling of sadness and loss of interest. It usually causes the patient to stop doing his normal activities.
Post-traumatic Depression: ↑ Mental health condition that is triggered by a certain event, most likely the accident that caused the traumatic brain injury.
Neurotransmitter: ↑ A chemical secreted by a brain cell that acts as a messenger between the brain cell and another brain cell, a muscle cell, or a gland cell.
Psychotherapy: ↑ A process that involves talking with a therapist to treat a mental illness like depression or emotional problems. Also called talk therapy or counseling.
Antidepressants: ↑ Medications that help to relieve or prevent depression by correcting the imbalance of certain neurotransmitters in the brain.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Wilmoth, K., and McCrea, M. 2020. What do we learn from studying traumatic brain injury? Front. Young Minds. 8:158. doi: 10.3389/frym.2019.00158
[2] ↑ Military Health System. 2022. DOD TBI Worldwide Numbers. Military Health System. Available online at: https://health.mil/Military-Health-Topics/Centers-of-Excellence/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBI-Worldwide-Numbers (accessed January 20, 2023).
[3] ↑ Dewan, M. C., Rattani, A., Gupta, S., Baticulon, R. E., Hung, Y. C., Punchak, M., et al. 2018. Estimating the global incidence of traumatic brain injury. J Neurosurg. 130:1–18. doi: 10.3171/2017.10.JNS17352
[4] ↑ GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. 2019. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18:56–87. doi: 10.1016/S1474-4422(18)30415-0
[5] ↑ Centers for Disease Control and Prevention. Surveillance Report of Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths 2014. Available online at: https://www.cdc.gov/traumaticbraininjury/get_the_facts.html (accessed January 20, 2020).
[6] ↑ Neumann, D. 2017. Treatments for emotional issues after traumatic brain injury. J. Head Trauma Rehabil. 32:283–5. doi: 10.1097/HTR.0000000000000337
[7] ↑ Juengst, S. B., Kumar, R. G., and Wagner, A. K. 2017. A narrative literature review of depression following traumatic brain injury: prevalence, impact, and management challenges. Psychol. Res. Behav. Manag. 10:175–86. doi: 10.2147/PRBM.S113264
[8] ↑ Rapoport, M. J. 2012. Depression following traumatic brain injury: epidemiology, risk factors and management. CNS Drugs. 26:111–21. doi: 10.2165/11599560-000000000-00000
[9] ↑ Lucke-Wold, B. P., Logsdon, A. F., Nguyen, L., Eltanahay, A., Turner, R. C., Bonasso, P., et al. 2018. Supplements, nutrition, and alternative therapies for the treatment of traumatic brain injury. Nutr. Neurosci. 21:79–91. doi: 10.1080/1028415X.2016.1236174
