Abstract
Traumatic brain injury, or TBI, is an injury to the brain caused by a bump or hit to the head. It is a common injury in children and can cause lasting symptoms and disabilities. There are different causes of TBI, such as car accidents, falls, or football tackles. Fortunately, there are ways we can reduce TBI by making safe choices, such as buckling our seatbelts and wearing helmets while playing sports.
Introduction
Before we dive into talking about brain injury, we want to introduce something scientists call the Monroe-Kellie Doctrine, which is important for understanding how traumatic brain injury (TBI) happens. Think about your skull like a suitcase. If you are packing for a trip, you can only fit in a certain number of items. So, if you pack too many clothes, you would not be able to pack other things, like your favorite book. The Monroe-Kellie Doctrine states that there is a limited amount of space in the skull to hold all of the cells that make up the brain tissue, the blood that supplies oxygen to the tissue, and a special type of fluid that cushions the brain, called cerebrospinal fluid. So, because the space is limited, if there is an increase in any one of these three things, one or both of the other two will have to decrease. That means that if you hit your head and the brain swells, there will be less room for blood, which could mean the brain will become even more injured. Or, if you hit your head and the blood vessels in your brain start to bleed, the brain tissue may end up getting squished to make room for the blood.
Types of Head Injuries
There are different types of TBI. First, we will talk about primary vs. secondary injuries. A primary injury is the initial injury; we will discuss what you can do to prevent a primary injury from happening. After the primary injury, secondary injury can cause even more damage to the cells and tissues. Some common examples of secondary injuries include inflammation (where brain tissue and blood vessels swell), hypoxia (when there is less oxygen going to the brain), and cellular death [1].
TBIs can also be grouped into two types: focal vs. diffuse. Focal means that the injury occurred in a specific part of the brain. As you can see in Figure 1, the brain is divided into different parts, each with a different job.
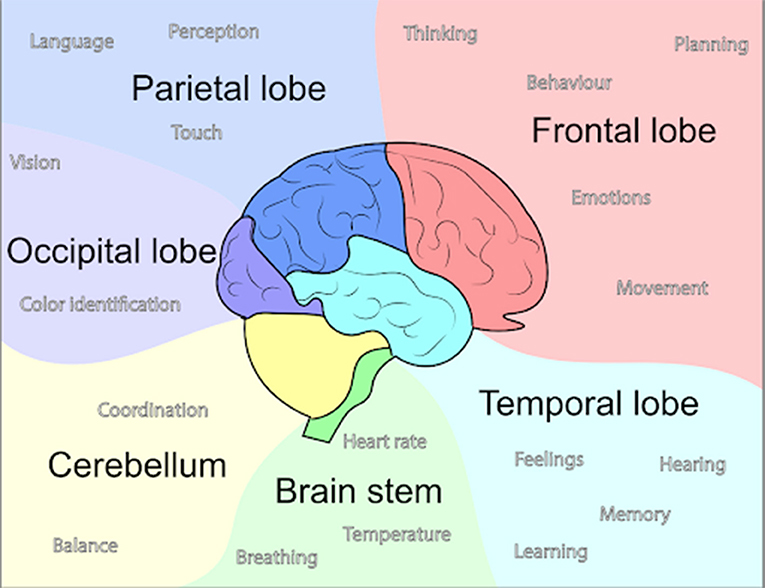
- Figure 1 - The brain is divided into different sections, called lobes, shown in different colors in this diagram.
- Lobes control things like movement, speech, and behavior. When a head injury occurs to a certain lobe or brain structure, then the functions that lobe or structure is responsible for can be impaired. For example, an injury to the temporal lobe can result in memory loss.
Many focal injuries occur in the membranes covering the brain and spinal cord, which are called the meninges (see Figure 2). For instance, blood can collect between the two outermost membranes. We call this type of bleeding a hemorrhage or hematoma [2]. This takes us back to the Monroe-Kellie Doctrine. In hemorrhage, if too much blood builds up in the skull, the amount of brain tissue and/or cerebrospinal fluid must decrease. Compression of brain tissue can damage or kill brain cells, and this can prevent a person from functioning normally.
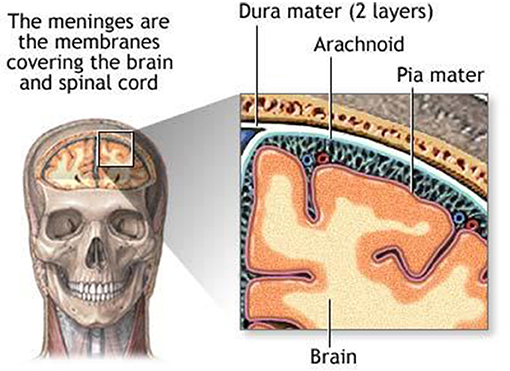
- Figure 2 - The membranes covering the brain and spinal cord are called the meninges.
- The three meninges are called the dura, arachnoid, and pia mater. Bleeding most commonly occurs between the dura and the arachnoid layers. Public domain image obtained from Wikimedia Commons: https://commons.wikimedia.org/wiki/File:Meninges_diagram.jpg.
Diffuse injuries occur over a larger area of the brain. In many of these injuries, less oxygen flows into the brain, similar to what happens in hypoxia [3]. Another common type of diffuse brain injury involves damage to the axons, which are the parts of brain cells that transport signals between the brain cells and the body. Axon damage can lead to the inability to move normally [2].
Brain injuries can have many other symptoms besides movement problems. Speaking normally, understanding what other people are saying, memorizing things, and eating can become difficult. Sometimes, mood swings and even depression can occur. Fortunately, patients can re-learn some of these tasks with therapy. The type of therapy a patient needs will depend on the location and severity of the injury, but might include physical therapy (to help with muscle weakness), occupational therapy (to help adapt to challenges in fine motor skills like brushing your teeth or cutting up your food), psychological counseling (to help with depression and anxiety), or appointments with a learning specialist (to help with problems reading and focusing).
Now that you have a general idea of what TBI is, we will discuss how these injuries occur and, more importantly, how you can prevent one from happening.
Causes, Mechanisms, and Preventions
In children and teenagers, the brain and skull continue to grow and more complex brain functions develop [4]. Because of these changes, TBIs can affect children at different ages in distinct ways. For instance, a brain injury could cause more harm to a baby than it would a teenager, by interfering with normal brain growth and development.
Unfortunately, TBIs can occur during many fun activities (such as sports, running, or walking) and/or other things that we spend a lot of time doing (such as driving/riding in a car). Fortunately, however, there are ways to reduce our risk of TBI! Table 1 includes the common causes of TBI. Scientists have learned a lot about how TBI happens, by studying it in humans as well as modeling the condition in animals. While it may seem strange to give an animal like a mouse a TBI, it is a great opportunity for TBI researchers because, by using animals, variations that occur in humans, like diet, sleep cycles, and genetics, can be tightly controlled so that we know which factors contribute to TBI. From the human and animal studies, scientists have learned that TBIs activate a number of processes in the body, such as inflammation, cellular stress, and cell death.
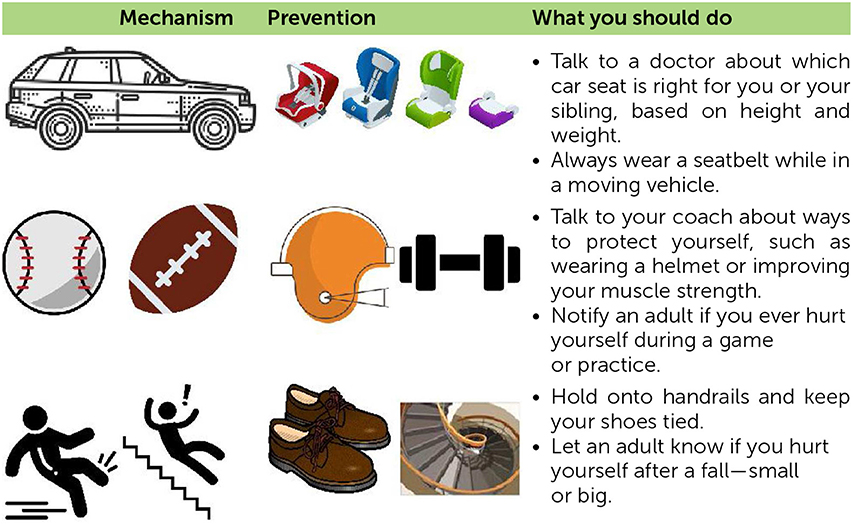
- Table 1 - A summary of the most common mechanisms of TBI, and some easy prevention strategies to practice.
Sports-Related Injuries
A hit to the head can occur while playing tackle football, skateboarding, doing gymnastics, or playing softball; thankfully, most are of these head injuries are mild injuries, such as concussion [5, 6]. But there is a good reason that parents, coaches, and other grownups always tell us to wear our helmets! Helmets protect the head, brain, and face from injuries while we play the sports we love. A helmet works best when it is the right size, when the chin strap is buckled tightly, and when there is padding on the inside. If a helmet is too big, not buckled, or is not cushioned, then when a player is tackled or a skateboarder wipes out, a TBI is more likely to occur [7]. While helmets typically do a great job of protecting us, TBIs can still happen even when we wear them. You should always tell an adult (a parent, guardian, or coach) if you hit your head, so that the adult can check you out and take you to a doctor if needed! Researchers are trying to improve helmet design by making the outside and inside work together better to protect your head from TBI, so that you can keep participating safely in the sports and activities that you love [7].
Motor Vehicle Collisions
Motor Vehicle Collisions (MVCs) can result in many types of injuries, including TBI. Injuries from an MVC cannot always be avoided, but they can be minimized by practicing seat belt safety. Seat belts keep us from being jerked around during fast turns and sudden stops. If your seatbelt is not worn properly, it is more likely that you could hit your head on objects inside the car or even get thrown from the car in the case of a collision. Researchers have found that people who were properly wearing their seat belts during MVCs were less likely to have TBIs, and they also had lower rates of TBI complications, such as brain bleeds or memory loss [8]. This is just one of the reasons why it is always important to wear a seat belt, and to use additional restraints, such as booster seats, if needed. These safety measures apply whether you are just traveling down the street or all the way across the state. Kids are not always big enough to fit into their seat belts properly. If you can wiggle in the seat belt, then an additional restraint, like a car seat or booster cushion, is suggested [9]. This is usually the case for all kids, from babies to 11-years-old. It is important to remember that the type of car seat or booster seat needed depends on the child's height and weight. Be sure to check the manufacturer's guidelines or check with a doctor when choosing a product that will keep you safe in the event of an MVC.
Falls
An innocent slip and fall can result in serious injuries, including a TBI. Falls can happen anywhere: walking around the house (especially with socks on a tile floor), playing tag in the park, going up and down the stairs, or jumping on the bed [4]. To prevent falls from happening, always use a handrail when going up and down stairs, do not run inside the house, keep your shoes tied to avoid tripping, and refrain from standing or jumping on furniture.
What else can I do?
Other than taking the common safety measures we have described, there are other things that you can do every day to help make your brain more resistant to injury. It all begins with living an active and healthy lifestyle. This means that it is important to eat your green vegetables (especially spinach!) because they contains a lot of vitamin E, which helps your brain cells, and thus your brain, to stay in tip-top shape [10].
When your brain is performing at its best, it is more likely to recover from an injury. Junk foods like cheeseburgers, chips, and ice cream are good to eat on occasion, but it is important to remember that we need to keep our brains and bodies healthy. Exercise is also important for building your brain's resistance to injury [10]. You can go to the park to play with your siblings and friends a few times a week or play sports–wearing a helmet, of course!
Conclusion
Scientists have put a lot of time and effort into learning about how TBIs occur, their impact on the human body, and the ways we can better protect ourselves from TBI (such as better helmet design). Although there are multiple types of head injuries, all with different symptoms, the important thing to remember is that they all result in an imbalance of brain fluid, tissue, and blood within the skull.
Glossary
Traumatic Brain Injury (TBI): ↑ A brain injury caused by a bump or hit to the head.
Focal Injury: ↑ A brain injury that occurs in a specific part of the brain.
Meninges: ↑ The membranes covering the brain and spinal cord.
Diffuse Injury: ↑ A brain injury that occurs over a wider area of the brain.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Reference
[1] ↑ Bramlett, H. M., and Dietrich, W. D. 2015. Long-term consequences of traumatic brain injury: current status of potential mechanisms of injury and neurological outcomes. J. Neurotrauma 32:1834–48. doi: 10.1089/neu.2014.3352
[2] ↑ Davidsson, J., and Risling, M. 2011. A new model to produce sagittal plane rotational induced diffuse axonal injuries. Front. Neurol. 4:41. doi: 10.3389/fneur.2011.00041
[3] ↑ Andriessen, T. M., Jacobs, B., and Vos, P. E. 2010. Clinical characteristics and pathophysiological mechanisms of focal and diffuse traumatic brain injury. J. Cell. Mol. Med. 14:2381–92. doi: 10.1111/j.1582-4934.2010.01164.x
[4] ↑ Ibrahim, N. G., Wood, J., Margulies, S. S., and Christian, C. W. 2012. Influence of age and fall type on head injuries in infants and toddlers. Int. J. Dev. Neurosci. 30:201–6. doi: 10.1016/j.ijdevneu.2011.10.007
[5] ↑ Pfister, T., Pfister, K., Hagel, B., Ghali, W. A., and Ronksley, P. E. 2016. The incidence of concussion in youth sports: a systematic review and meta-analysis. Brit. J. Sports Med. 50:292–7. doi: 10.1136/bjsports-2015-094978
[6] ↑ Sharma, V. K., Rango, J., Connaughton, A. J., Lombardo, D. J., and Sabesan, V. J. 2015. Current state of head and neck injuries in extreme sports. Orthopedic J. Sports Med. 3:1–6. doi: 10.1177/2325967114564358
[7] ↑ Daneshvar, D. H., Baugh, C. M., Nowinski, C. J., McKee, A. C., Stern, R. A., and Cantu, R. C. 2011. Helmets and mouthguards: the role of personal equipment in preventing sport-related concussions. Clin. Sports Med. 30:145–63. doi: 10.1016/j.csm.2010.09.006
[8] ↑ Kuo, C., Chiou, H., Lin, J., Tsai, S., Chiang, Y., Lin, C., et al. 2015. Seatbelt use and traumatic brain injury in Taiwan: a 16-year study. Iran J. Public Health 44:470–8. doi: 10.1016/b978-0-12-802686-1.00010-9
[9] ↑ World Health Organization. The Need for Seatbelts and Child Restraints.
[10] ↑ Gomez-Pinilla, F., and Kostenkova, K. 2008. The influence of diet and physical activity on brain repair and neurosurgical outcome. Surg. Neurol. 70:333–6. doi: 10.1016/j.surneu.2008.05.023