Abstract
Burn injuries range from being quite mild, like sunburn, to very severe, like burns from touching fire. Burns cause pain and can result in long-term complications such as scarring or limited function of the affected body part. Burn severity is classified based on how deep the burns are which ultimately affects the recovery process. Skin grafting, which involves replacing burn-damaged skin with healthy skin, can be used to treat severe burns and help them heal. Skin grafts can come from the burn patients themselves for from other people who volunteer to donate some of their skin. This article explores how burns affect the body and describes the science of skin grafts, including how they work and new techniques to improve burn healing, like stem cell therapy.
Introduction
Every year, millions of people worldwide suffer from burn injuries due to various causes such as fire, hot surfaces, chemicals, and electrical accidents [1]. Burn injuries range from mild (like sunburn) to severe (burns from touching fire). Burns can not only cause significant pain but can lead to long-term problems such as scars and poor function of the burned body part [1]. Skin grafting is one treatment that has been used effectively to promote healing and restore skin functions in burn victims [1]. Skin grafts involve transplanting healthy skin to the burn site. This article will discuss burns and how skin grafts can be used to treat them.
What Happens During a Burn?
How bad a burn is, also known as its severity, depends on many factors. These include which area(s) of the body was burned, how much of that area was burned, and for how long that area was exposed to the source of the burn [1]. After a burn injury, the body begins to repair the damaged tissue through a process called inflammation.
Initially, the burned area shows signs of inflammation, such as redness and swelling, as blood rushes to the burn site carrying white blood cells (WBCs). These WBCs are the “clean up team”; they serve as the front line of defense, fighting any potential bacterial invaders and attempting to stop any infection that could take place. WBCs also release chemicals that help the body fight infection and allow it to heal.
The inflammation phase can also cause pain due to the flow of blood and body chemicals that are trying not only to fight infection, but also to repair the damaged skin. Over approximately three days, the body begins to make collagen, an important skin protein that helps to rebuild and strengthen the damaged tissue.
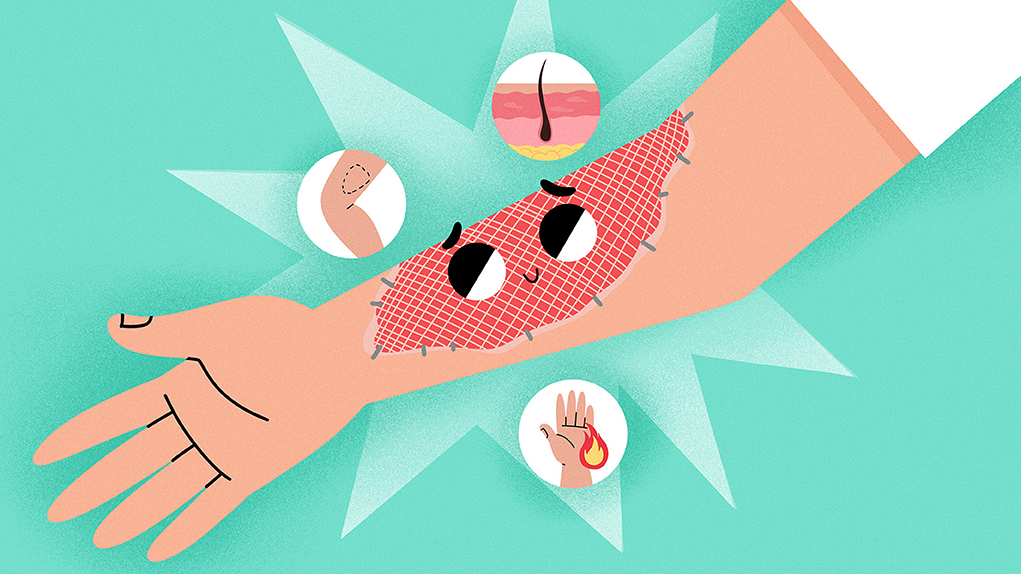
The skin can be divided into three layers (Figure 1). The top layer is the epidermis, then we have the dermis, and under the dermis is the subcutaneous tissue (hypodermis). Burns are classified based on their depth through these layers, with deeper burns being more severe. A summary of burn types and their characteristics is shown in Table 1.
- Figure 1 - The skin has three main layers: the epidermis, the dermis, and the hypodermis.
- The severity of burns is determined by how deeply they penetrate through these layers. First degree burns affect only the epidermis. Second degree burns affect the epidermis and dermis. Third degree burns affect all three skin layers and are therefore the most severe.
| Burn degree | Skin layers affected | Appearance | Healing time |
|---|---|---|---|
| First degree | Epidermis (first/top layer) | Pink and dry | 5–10 days (no scarring) |
| Second degree | Epidermis and surface of dermis (second/middle layer) | Pink or red, blisters (fluid filled pockets) | 2–3 weeks (scarring may occur) |
| Third degree | Epidermis, dermis, hypodermis (third/bottom layer) | Brown or black, leathery and dry | May take months and require surgery to heal |
- Table 1 - Burn classification.
The medical problems that happen following burn injuries can be very severe. The inflammation that occurs after a burn may cause full-body complications, such as low blood pressure and organ damage. The lungs may be injured after inhaling smoke. The kidneys can be injured following inflammation and low blood pressure. Patients are prone to developing infections as well. These complications are usually worse with higher-degree, larger burns [1].
The Science Behind Skin Grafts
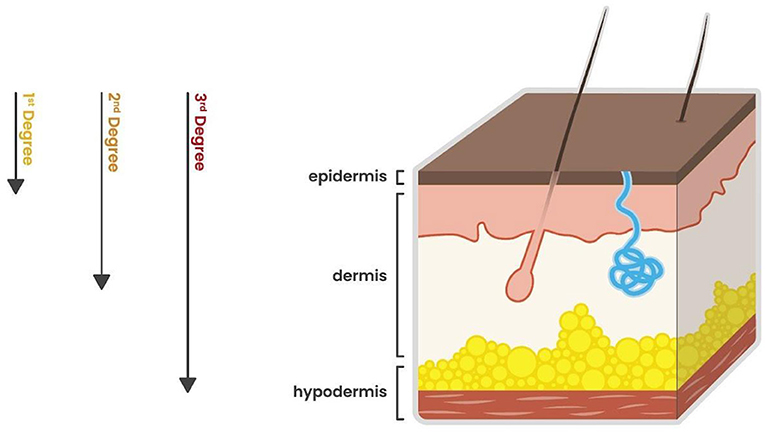
Skin grafting is used to treat severe burns. It involves taking healthy skin from a healthy part of the body to treat the damaged area (Figure 2) [2]. Skin grafts vary based on where the skin comes from and what types of burns it can be used for [3]. Autografts come from the patient’s own healthy skin in an unburned part of the body. Allografts are taken from another individual of the same species, like from someone who has died. Xenografts are skin taken from animals. For example, pig skin can be used to replace the skin in the burnt area. Allografts and xenografts are temporary solutions until the patient’s own skin is healthy enough to be used.
- Figure 2 - Left arm after a burn and skin graft.
- There is a rectangular skin graft shown here. The color is slightly different to the patient’s arm skin, which can sometimes happen. Sutures (stitches) are seen securing the graft to the patient’s arm.
Split-thickness skin grafts (STSGs) are composed of the top layer of the skin (the epidermis and the outer layer of the dermis) and are used for larger wounds. Full-thickness skin grafts (FTSGs) contain all the skin layers and are used for smaller areas. Composite grafts contain skin and other tissue types like cartilage, and they are used if the burn damages the muscles and bones underneath the skin. These grafts also have their own blood supply, so they are ideal for healing wounds with poor blood circulation.
STSGs are the fastest to heal and the least likely to scar because they contain the least amount of skin layers. FTSGs, because they are thicker, take longer to heal but provide more natural-appearing results. Composite grafts also have a long healing time and scar similarly to FTSGs due to their thickness.
Process of Skin Grafting
The degree of the burn determines the size and thickness of the graft [4]. Most often, skin grafting requires hospitalization to monitor healing and watch for signs of infection [5]. The first step in emergency in-hospital treatment is to give medicines called antibiotics to prevent infection, and pain medication as needed. Then, the burned area is cleaned and damaged tissue is removed. This can be done surgically or non-surgically. Then a burn cream is applied to the wound.
At this stage, the graft can be taken from another body part, which is determined by accessibility, skin color, and wound healing ability. The most common areas are the buttocks, stomach, and thigh. The skin graft is removed using a small razor blade or an electric shaver, and it can then be made into a mesh by using a special machine that puts tiny holes in it. The mesh pattern allows natural inflammatory fluids at the burn site to pass through the holes so they do not lift the graft off the underlying surface as they are produced. After removal, a sponge and dressing are commonly applied to the site where the graft was taken, to decrease blood loss and pain and to speed up skin growth. Sometimes the graft is a slightly different color to the surrounding skin that it is attached to. The way it looks is caused the “cosmetic affect”.
The burned area is called the recipient area. The graft can be applied directly onto the recipient area and kept in place by either staples, sutures, steristrips (paper stitches), or pressure dressings. It is kept hydrated with a moisturizing gauze or a covering that protects against air and water exposure. Dressings are usually changed 3 days after the operation and every day thereafter [6].
The Future of Skin Grafts and Burn Treatment
Although the overall survival of the skin graft is vital, the appearance of the graft after it heals is equally important. Scars are common after a skin graft procedure and can cause stress, pain, and decreased movement. Additionally, wound healing can take a long time and can lead to changes in skin color.
Many new ideas are being developed for burns treatments and skin grafts [2]. For instance, a potential treatment for scarring is the use of stem cells. Stem cells are special cells that can turn into other cell types, making them ideal for wound healing. Another new treatment is the use of silicone, which is commonly used to create a protective layer that acts like a layer of the skin. Silicone has been shown to decrease pain, itchiness, and scar thickness. There has also been an increased use of laser therapy to improve the look of the healed skin after burn injuries. Lasers can help the tissue to repair itself, decrease scar thickness, and improve overall skin function.
Skin tissue engineering is a developing field in which new living tissue can be made to imitate human skin [2]. Much research has focused on producing living tissue that has the appropriate strength and healing abilities. The future of skin tissue engineering looks promising as new advances are being made; however, there is still room for improvement to make sure that engineered skin fits well with the body’s own tissue and looks natural.
Conclusion
In summary, when the skin suffers a burn injury, the body starts a complicated healing process involving inflammation and tissue repair. The severity of the burn varies from first to third degree, based on depth. Severe burns can lead to complications like infections. Skin grafting is commonly used to treat severe burns and involves transplanting healthy skin to the damaged areas. Various types of skin grafts exist, and each has its own unique healing properties and sources. Despite the success of skin grafting, it often results in scarring and decreased skin elasticity or “stretchiness”. Emerging treatments like stem cell therapy, silicone application, and laser therapy aim to improve outcomes. Skin tissue engineering is a new technique that holds promise but requires further development for optimal integration and longevity. Hopefully, continued research into skin grafting will help people with severe burns to have better function and cosmetic effect.
Glossary
Skin Grafting: ↑ Putting new skin on an area that has been burnt. It can be the patient’s own skin from a different site, donor skin (from someone else), from an animal or from synthetic (manmade) material.
Inflammation: ↑ The body’s response to an injury, including a burn. It involves redness, heat, pain and loss of function.
Collagen: ↑ Protein that makes up tissues in the body.
Sutures: ↑ Stringlike material used by doctors to sew tissue together; also called stitches.
Steristrips: ↑ Thin, tape-like strips of paper that are used to hold tissues together.
Pressure Dressings: ↑ An external bandage applied to a wound to provide a little pressure to stop fluid from building up inside the wound.
Stem Cells: ↑ Very young cells that have the potential to develop into many different body parts/tissues.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AI tool statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
[1] ↑ Jeschke, M. G., van Baar, M. E., Choudhry, M. A., Chung, K. K., Gibran, N. S., and Logsetty, S. 2020. Burn injury. Nat. Rev. Dis. Primer. 6:11. doi: 10.1038/s41572-020-0145-5
[2] ↑ Anyanwu, J. A. and Cindass, R. 2023. “Burn debridement, grafting, and reconstruction”, in StatPearls (Treasure Island, FL: StatPearls Publishing). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK551717/ (Accessed on 24 July 2024).
[3] ↑ Braza, M. E. and Fahrenkopf, M. P. 2025. “Split-thickness skin grafts”, in StatPearls (Treasure Island, FL: StatPearls Publishing). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK551561/ (Accessed on 24 July 2024).
[4] ↑ Andreassi, A., Bilenchi, R., Biagioli, M., and D’Aniello, C. 2005. Classification and pathophysiology of skin grafts. Clin. Dermatol. (2005) 23:332–7. doi: 10.1016/j.clindermatol.2004.07.024
[5] ↑ Ryssel, H., Gazyakan, E., Germann, G., and Öhlbauer, M. 2008. The use of MatriDerm® in early excision and simultaneous autologous skin grafting in burns—a pilot study. Burns. 34:93–7. doi: 10.1016/j.burns.2007.01.018
[6] ↑ Valencia, I. C., Falabella, A. F., and Eaglstein, W. H. 2000. Skin grafting. Dermatol. Clin. 18:521–32. doi: 10.1016/S0733-8635(05)70199-6