Abstract
Did you know the reason behind wearing sunscreen is more than just preventing a sunburn? Sun damage to the skin over a lifetime can lead to the most dangerous type of skin cancer, called melanoma. Melanoma is abnormal growth of the pigment-producing cells of the skin, the same types of cells that make up moles. Though rare in young people, the risk for melanoma increases with age. Melanoma in kids looks and acts differently than it does in adults, often making the diagnosis challenging for doctors. Early diagnosis is important so that the melanoma can be removed and treated before it spreads to other parts of the body. Protective actions done in childhood, such as wearing sunscreen, avoiding excessive sun exposure, and wearing protective clothing when out in the sun, will help to prevent melanoma later in life.
Melanoma is a form of skin cancer that develops in cells called melanocytes, the pigment-producing cells of the skin (Figure 1A). Moles might come to mind upon hearing the word melanoma. That is because moles are made up of melanocytes, giving them their dark color (Figure 1B). Some people are born with these spots, while other times they appear on the skin throughout a person’s lifetime. Pigmented skin lesions are usually perfectly harmless. However, repeated damage to the skin from the rays of the sun can lead to abnormalities in melanocytes. Most of the time the body can detect the damage and fix it before any abnormal growth happens. If the body cannot fix the damage, the melanocytes reproduce uncontrollably (Figure 1C), resulting in melanoma. Preventing melanoma and treating it early are extremely important, because it is the deadliest type of skin cancer.
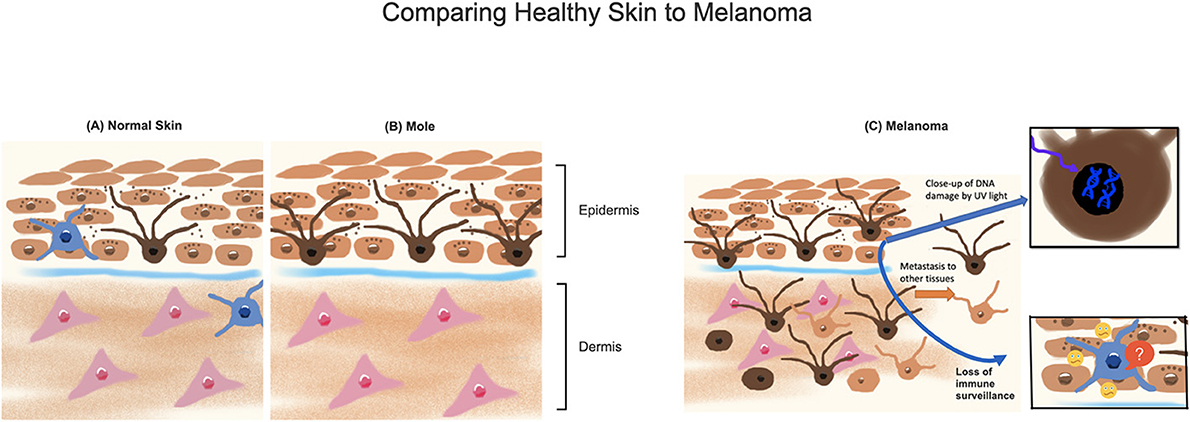
- Figure 1 - (A) Normal melanocytes (dark brown cells with “arms”) produce a pigment called melanin (dark brown dots), which is taken up by neighboring skin cells (light brown).
- Immune cells are shown in blue. (B) Multiple melanocytes close to each other form a normal mole in the skin. (C) Melanoma can develop when sunlight damages cells, creating abnormal DNA and loss of immune cell functions. Melanocytes replicate and spread into the deeper layers of the skin and non-skin tissues. Melanocytes may also change shape, lose color, or exhibit other changes.
What Causes Melanoma?
The way melanoma develops is virtually the same in children and adults. If you have ever been sunburned (ouch!), you have already experienced how the sun can damage the skin. But what does the sun have to do with melanoma? To understand, let us first review how healthy skin is made. The body, including your skin, is made up of building blocks called cells. Each cell contains a specific code, called DNA, which provides instructions for many things cells do, including how to grow, what shape to take on, and how to do their jobs in a tissue or organ to help your body function. Each piece of DNA needs to be in the correct order, just like letters need to be in the correct order to form a word that makes sense. Cells have ways of proof-reading the DNA for any abnormalities. If anything goes wrong in the process of building the DNA, checking it over, or repairing any mistakes in the code, cancer can develop (Figure 1C).
Genetic mutations are the first step in the formation of a melanoma. Some people are born with errors in their DNA codes, while others develop errors over time because of things they experience or are exposed to during their lifetimes. Powerful ultraviolet rays from the sun can penetrate the skin and directly alter DNA, resulting in the wrong code being formed in melanocytes. If mutations occur in the parts of the DNA coding for anti-cancer or repair proteins, the body cannot fix the damage [1]. Mutations could also turn on a “gas pedal” for cell division or turn off a “brake” pedal that helps stop cell division, and either can result in abnormal cell growth. For cells that are normally dividing, a special anti-cancer mechanism called contact inhibition kicks in so that cells stop dividing when they contact each other and do not pile up on top of each other. Mutations that affect contact inhibition also contribute to cancer.
The skin contains special immune cells that detect damaged or pre-cancerous cells and send them a signal that causes them to break down and eventually die. But melanocytes tend to be more resistant to this signal, so the mutated cells often do not die when the immune cells tell them to [1]. Sun damage also makes it hard for the immune cells to do their jobs properly, because sunlight can damage the immune cells or interfere with their functions. The risk of melanoma is increased in children and adults who are immunosuppressed, meaning medications or diseases that prevent the immune system from protecting the body. Immunosuppression can impede the immune system’s ability to get rid of precancerous or cancerous cells.
These factors together, from DNA damage to loss of protective anti-cancer mechanisms, result in melanoma. Like other types of cancers, for this to occur, multiple “hits” are required, which is why you do not develop melanoma after one sunburn. These “hits” include repeated sun exposure and being born with DNA that is more likely to be damaged.
How Do Doctors Know If a Spot is Melanoma?
Clinicians often use a list of characteristics known as the “ABCDE” criteria (Figure 2) to remember features that might indicate melanoma in adults. If there is a spot on the skin that is very noticeable, or that looks different from all the other spots on a person’s body, this may indicate that it is cancerous. In young people, melanoma can look different than it does in adults and may not always follow the conventional ABCDE criteria, making the diagnosis difficult [2]. In kids, melanomas are more likely to lack pigment, bleed, make raised bumps, appear uniform in color (pink or red), form from new spots on the skin, and have varying sizes [3]. Because melanoma may present differently in children, it is often mistaken for non-cancerous growths, such as warts.
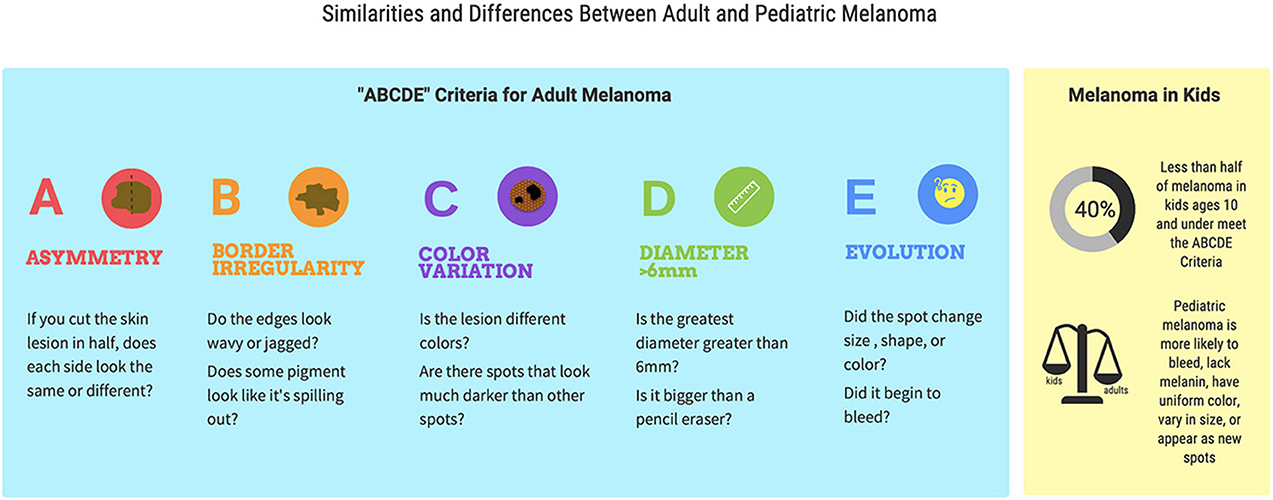
- Figure 2 - The “ABCDE” criteria help doctors to diagnose melanoma in adults.
- These characteristics include asymmetry, border irregularity, color variation, diameter >6 mm, and evolution/change of the spot. However, only 40% of children ages 10 years and younger meet the adult ABCD criteria. Pediatric melanomas tend to lack pigment, bleed, make raised bumps, appear uniform in color (pink or red), form from new skin spots, and have varying sizes [3].
When doctors are worried that a spot on the skin might not be harmless, they look at it closely, sometimes using a magnifying tool called a dermatoscope. To diagnose melanoma, doctors need to remove all or part of the mole to examine it using a microscope, in a procedure called a biopsy. Special stains that color cancerous cells can be used on the skin sample from the biopsy. These stains can help the doctor decide if the skin sample is cancer or not. Certain features of the biopsy sample are also noted, such as how thick the tumor is and how many dividing cells are seen. Thicker melanomas are associated with worse outcomes and decreased survival [4].
Risk Factors for Melanoma in Children
Pediatric melanoma is quite rare. It is estimated that 1–9 per 1,000,000 children are diagnosed with melanoma each year [2], and the incidence in children is declining [2, 5]. The majority of melanomas in children occur with no known cause, and risk increases with age. As with adults, excessive sun exposure, indoor tanning, and multiple sunburns are risk factors for children [2].
Additionally, certain traits, medical conditions, and medications can put children at higher risk [2]. Children with lighter skin, blonde or red hair, and blue eyes are more likely to get melanoma. Children who sunburn easily, freckle, or tan poorly are at higher risk. Having a parent or sibling with melanoma also increases a child’s risk of melanoma. Certain diseases that make children more sensitive to the sun increase melanoma risk, too. Lastly, kids who are born with large or giant-sized pigmented birth marks or who have a high number of moles are also at a higher risk of developing melanoma [5].
How is Melanoma Treated in Kids?
The overall survival for children with melanoma is estimated to be 93% [5]. The outcome of melanoma in children is better than it is in adults. The gold standard of melanoma treatment for both children and adults is surgery. The surgery involves removing the tumor along with a small amount of normal skin surrounding it, making sure all of the cancer cells are removed. It is important to diagnose melanoma early to fully remove and treat the cancer, to prevent it from spreading to other parts of body. When any type of cancer spreads to other parts of the body, this is called metastasis. Melanoma tends to metastasize to the lymph nodes, nearby skin, lungs, brain, liver, and bones [4]. To understand why this spread is bad, think about a laptop computer. If you spilled a small amount water on the outside of the laptop and cleaned it up shortly after, the computer would still function. If the water is not wiped up, it might seep inside the laptop and cause the keyboard or screen to stop working. If the water spreads deep into the hard drive, the computer might no longer turn on. The initial spill of water is like melanoma that has not spread, but the further it spreads, the more negative consequences it has.
If a melanoma cannot be fully removed, or if it has spread, medications are available. Medications that strengthen the immune system are approved for both children and adults, while medications targeting the melanoma itself are currently approved only for adults [5]. In cases of metastatic melanoma, chemotherapy drugs and radiation are used together.
Melanoma therapies unfortunately have side effects. Radiation and chemotherapy help kill off rapidly dividing cells, but some healthy cells are also rapidly dividing and can be killed by the therapies too. The side effects of chemotherapy and radiation often include hair loss, dry skin, diarrhea, and low red blood cell count, because cells in these tissues are constantly growing and replenishing. One side effect of immunotherapy is called vitiligo, a condition in which the immune system attacks healthy melanocytes and causes loss of pigment, resulting in patches of skin with no color. This is actually a good sign for people receiving immunotherapy, as it means their immune systems are more likely to fight off any melanoma that has metastasized.
How Can Kids Lower Their Risk of Melanoma?
Protective actions done in childhood are the most effective way to prevent melanoma later in life, because lifetime risk increases with prolonged or repeated damage to the skin [1]. Wearing sunscreen, avoiding excessive sun exposure (including indoor tanning booths), and wearing protective clothing (hats, long sleeves, and sunglasses) when out in the sun can help to prevent melanoma in the future. The sun is strongest between 10 a.m. and 2 p.m., therefore limiting outdoor time during those hours is helpful [2]. Remember that pediatric melanoma is extremely rare, and that most moles are normal. Your regular doctor can examine any concerning spots and, if needed, refer you to a specialized skin doctor called a dermatologist for a closer look.
Understanding the basics of melanoma and the need for protection against the sun early in life is the best way to keep your skin healthy, and now you can help educate others about melanoma to reduce their risks, too!
Glossary
Melanoma: ↑ A type of skin cancer that arises from uncontrolled replication and growth of pigment-producing cells.
Melanocytes: ↑ Skin cells that produce a brown-black pigment called melanin.
Mutation: ↑ A permanent change in the sequence of DNA that causes a gene to have an incorrect code.
Contact Inhibition: ↑ A normal anti-cancer mechanism that signals cells to stop dividing when they contact one another, preventing cells from growing more than one layer thick.
Immunosuppression: ↑ State in which the immune system does not function strongly to protect the body from diseases. This can be from medications like steroids or diseases like HIV.
Dermatoscope: ↑ A tool used to inspect the skin closely through magnification and light.
Metastasis: ↑ The spread of cancer cells from their original site to other parts of the body.
Vitiligo: ↑ A skin condition in which the immune system attacks pigment-producing cells, resulting in patches of skin with no color.
Conflict of Interest
JMR is an inventor on patent application #62489191, “Diagnosis and Treatment of Vitiligo” which covers targeting IL-15 and TRM for the treatment of vitiligo; and on patent application #15/851,651, “Anti-human CXCR3 antibodies for the Treatment of Vitiligo” which covers targeting CXCR3 for the treatment of vitiligo.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Gilchrest, B. A., Eller, M. S., Geller, A. C., and Yaar, M. 1999. The pathogenesis of melanoma induced by ultraviolet radiation. N. Engl. J. Med. 340:1341–8.
[2] ↑ Hawryluk, E. B. 2020. “Melanoma in children,” in UpToDate, eds M. L. Levy, and H. Tsao (Waltham, MA: Wolters Kluwer).
[3] ↑ Cordoro, K. M, Gupta, D., Frieden, I. J., McCalmont, T., and Kashani-Sabet, M. 2013. Pediatric melanoma: results of a large cohort study and proposal for modified ABCD detection criteria for children. J. Am. Acad. Dermatol. 68:913–25. doi: 10.1016/j.jaad.2012.12.953
[4] ↑ Damsky, W. E., Rosenbaum, L. E., and Bosenberg, M. 2010. Decoding melanoma metastasis. Cancers (Basel) 3:126–63. doi: 10.3390/cancers3010126
[5] ↑ Moustafa, D., Neale, H., and Hawryluk, E. B. 2020. Trends in pediatric skin cancer. Curr. Opin. Pediatr. 32:516–23. doi: 10.1097/MOP.0000000000000917
