Abstract
Could toy hearts possibly work as well as a real heart? To find out, we purchased six toy hearts, ranging from a spooky Halloween beating heart to a colorful plush heart. Our guess was that toy hearts would not work as well as a real human heart! We tested the toys in our laboratory using the exact same tools and methods we use for testing real hearts and mechanical blood pumps. We looked at flow, pressure, volume, and how well the toy heart pumped water. We also asked three heart surgeons to judge each toy heart based on how real they looked and what features they liked. As expected, the toy hearts were not realistic and could not pump as well as a real heart. This article combines human health and engineering as a fun and silly scientific question. Our hope is that readers will find it educational and entertaining!
The Heart is Important!
We are a group of scientists, engineers, and doctors who study the heart as part of our jobs. The heart is an extremely important organ! Humans only have one heart, and if it gets sick, it does not heal very well and we cannot grow a new one. The heart is made of muscle and is located inside the chest. It is about the size of a fist and it pumps blood through the body to keep a person alive. A special group of cells inside the heart, called the sinoatrial node, sends electrical impulses through the heart to tell the heart muscle cells to squeeze. When these cells squeeze at the same time, the whole heart squeezes and pumps blood to the rest of the body. When the heart muscle cells relax, the heart relaxes and can re-fill with blood for the next squeeze.
The blood pumped by the heart carries oxygen and nutrients to the rest of the body (Figure 1). Blood flows through the heart in a specific way. Blood inside the left atrium flows into the left ventricle through the mitral valve (all heart valves make sure blood flows in only one direction). Blood in the left ventricle then gets pumped through the aortic valve and into the aorta, which is a large artery that sends blood to smaller arteries that reach all the organs in the body, including the heart itself. The organs use up the oxygen and nutrients in the blood. Veins in these organs carry the oxygen-depleted blood and waste products back to the heart. All of the veins empty into the vena cava, which is the largest vein in the body. Blood flows from the vena cava to the right atrium, through the tricuspid valve, and into the right ventricle. The right ventricle pumps the blood through the pulmonic valve and into the pulmonary artery. The pulmonary artery sends blood to the lungs to get a fresh supply of oxygen. Oxygen-filled blood then leaves the lungs via the pulmonary veins and enters the left atrium. This cycle repeats with every heartbeat.
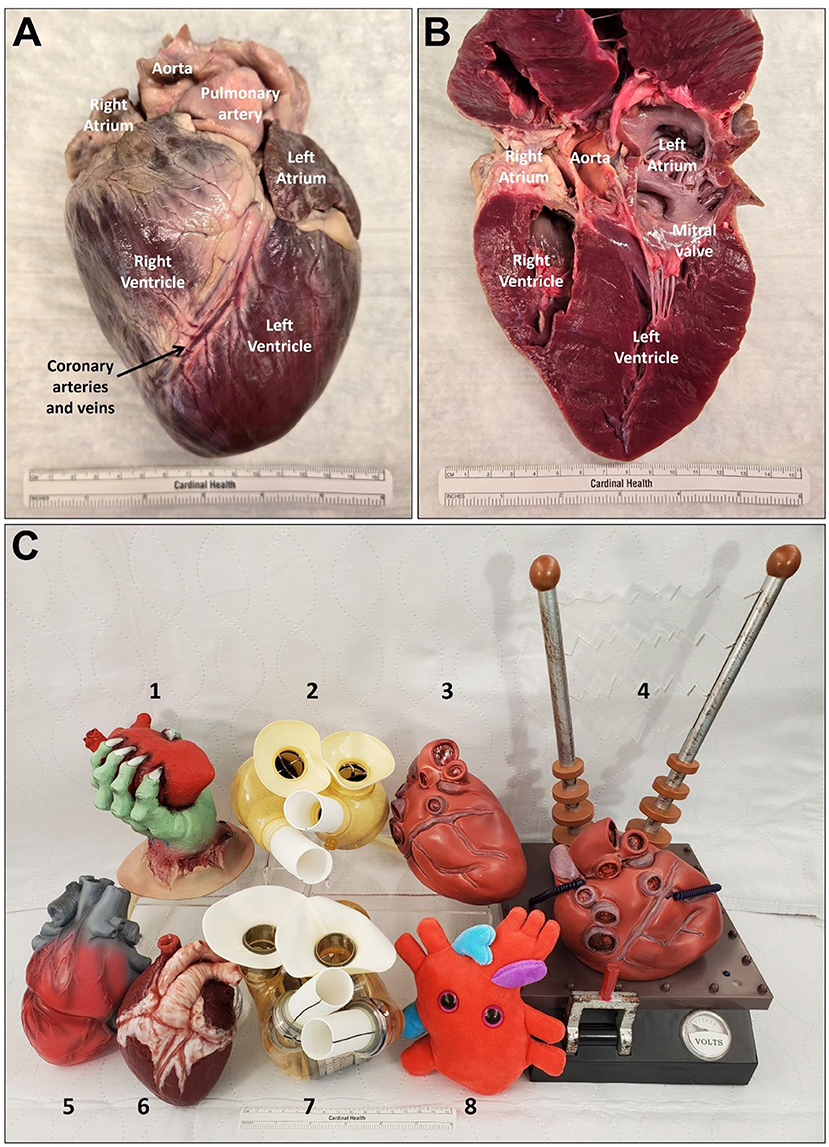
- Figure 1 - (A) The outside of a pig heart, looking at it from the front.
- The pig heart has the same structural features as a human heart. (B) The heart cut open, to show the structures on the inside. (C) The six toy hearts tested in this study and two real mechanical blood pumps. (1) Toy heart called Claw. (2) A SynCardia total artificial heart. (3) Toy heart called Beating. (4) Toy heart called Frankenstein. (5) Toy heart called Light Up. (6) Toy heart called Gummy. (7) An AbioCor total artificial heart. (8) Toy heart called Cute (Figure credit [1]).
The Heart can Get Sick
Sometimes a person’s heart becomes sick and weak. When this happens, it cannot pump enough blood to the rest of the body. This is a disease called heart failure [2]. Doctors first try to give the person medicines to help the heart work better. For some people, medicines are not enough and they continue to get sicker. The only treatment for heart failure is to get the person a new, healthy heart. This procedure is called a heart transplant. Transplanted hearts come from organ donors who have agreed (or their families have agreed) to give their hearts to someone else when they die.
There are more than 6 million people in the United States with heart failure, but the problem is only about 4,000 heart transplants are performed a year. Why so few? There are not enough donor hearts available for everybody who needs one. If a heart failure patient cannot get a new heart, they could die. How can we help all these people who need a heart transplant but cannot get one? Heart surgeons can implant a small machine inside the person’s chest to help their sick heart pump blood [3]. These machines are called mechanical blood pumps. Amazingly, these pumps have been in use since the 1960s and have helped more than 30,000 people!
Testing Toy Hearts
There are a lot of different toys hearts for sale in stores and online. We were curious how realistic these toys were and how well they actually worked. No one had ever studied toy hearts before. Since we are experts at studying the heart and mechanical blood pumps, we decided to have some fun with this experiment!
We bought six toy hearts, ranging from a spooky Halloween beating heart to a cute, colorful, plush heart (Figure 1C). We gave each toy heart a funny name: Claw, Beating, Frankenstein, Light Up, Gummy, and Cute. We asked three heart surgeons to judge each toy heart based on how realistic the heart looked and what interesting features they liked.
We tested each toy heart using the exact same tools we use for studying real hearts and mechanical blood pumps in our laboratory [4, 5]. We used special cameras to take pictures of the toy hearts. We then used plastic tubing to mimic a person’s circulatory system and we filled the tubing with water instead of real blood. We connected each toy heart to this system and used sensors to observe how well the toy heart pumped the water. We measured flow using a flow probe placed around the tubing. A flow probe calculates flow using crystal sensors to measure the speed that sound waves travel through the water. We measured pressure using a small tube filled with water (a catheter) that we placed inside the toy hearts. Pressure waves inside the toy hearts travel through the tubing to a bendable mechanical sensor—the higher the pressure, the more the sensor bends. We also measured volume using a catheter placed inside the toy heart. The catheter contains electrical sensors that measure changes in the diameter of different sections of the heart to calculate the total volume. The flow, pressure, and volume sensors used in the toy hearts are the same ones we use in our laboratory and in the hospital.
What did we Find?
As expected, the toy hearts did not work as well as a real heart. Figure 2 shows some photos from our experiments. Figure 3 shows the data from our experiments compared to a real, healthy heart.
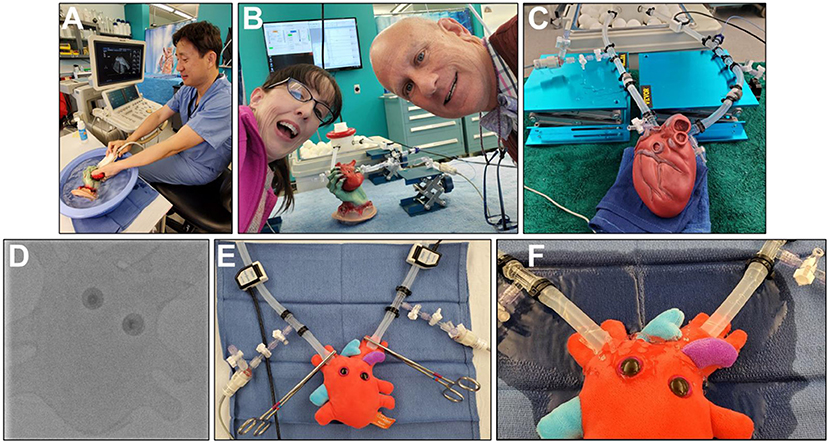
- Figure 2 - (A) Author Jiapeng taking images of Claw.
- (B) Authors Gretel and Steven having fun while testing how well Claw can pump water. (C) Beating during testing. (D) An X-ray image of Cute. (E) Getting Cute ready for testing. (F) Cute leaking water all over the place (Figure credit: (D–F) from Monreal et al. [1]). Figure contains images of the author(s) only.
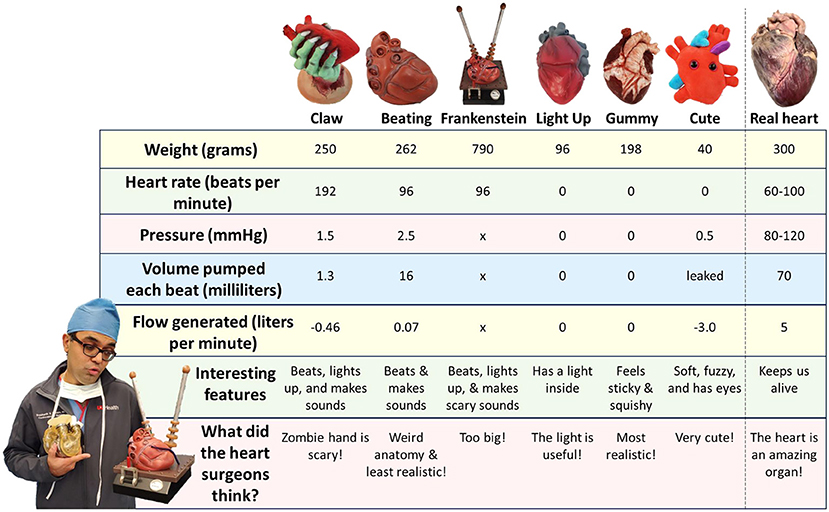
- Figure 3 - The results of our experiment compared to a normal, healthy heart.
- An “x” means the data were not collected.
We measured the weight of each toy heart. One of the toys, Beating, weighed 262 g. This is just a little lighter than a human heart, which weighs about 300 g—about the weight of two oranges. We measured each toy’s heart rate. A human heart beats 60–100 times a minute. Two of the toy hearts, Beating and Frankenstein, each beat 96 times per minute, which is just like a human heart. The toy heart Claw beat very fast–192 times a minute! This is much faster than a human heart and more similar to a rabbit or chicken heart. The other three toy hearts did not beat at all.
We used the flow, pressure, and volume sensors to find out how well each toy heart pumped water. A healthy human heart usually pumps 70 ml of blood during each heartbeat. The toy heart that worked the best (Beating) only pumped 16 ml of water during each beat (Figure 2C), which is more similar to a small dog’s heart. Claw was even worse—it only pumped 1.3 ml of water during each beat (Figure 2B). Light Up, Gummy, and Cute could not pump at all, and Cute leaked all over the place during our experiment (Figure 2F).
We asked three heart surgeons to carefully evaluate and score each toy heart on how realistic the hearts were and what features they liked. The heart surgeons did not like Claw’s zombie hand—it was too scary. They thought Beating had a weird structure (it was missing a lot of important blood vessels) and was not very realistic. They thought Frankenstein was too big. They thought that the light inside Light Up would be very helpful at night. Gummy was very sticky and squishy and was voted most realistic and their favorite toy heart. All three heart surgeons thought that Cute was—you guessed it—very cute!
What we Learned
We learned that the toy hearts we chose were not very realistic and did not pump very well at all. They definitely did not work as well as a real heart! Performing experiments like this is a good reminder that the heart is very important and we need to keep it as healthy as possible. Overall, this was a really fun experiment to perform, and it gave us a chance to use our knowledge to perform serious science on a very silly topic!
Glossary
Valve: ↑ A part of the heart that ensures that when the heart beats, blood only circulates in one direction. The human heart has four heart valves.
Artery: ↑ A type of blood vessel that carries oxygenated blood from the heart to the rest of the body.
Vein: ↑ A type of blood vessel that carries oxygen-depleted blood from the rest of the body back to the heart.
Heart Failure: ↑ A disease in which the heart becomes weak and cannot pump enough blood to the rest of the body.
Heart Transplant: ↑ A surgery where doctors remove a person’s sick heart and replace it with a healthy donor heart.
Mechanical Blood Pump: ↑ A small machine implanted inside the body (either inside the chest or inside a large blood vessel) to help pump blood when the heart is sick and weak.
Heart Surgeon: ↑ A type of doctor who is trained to perform surgery on the heart.
Circulatory System: ↑ The network of blood vessels and the heart that helps to circulate blood through the body.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Siddharth V. Pahwa MD, Michele Gallo MD, and Erin M. Schumer MD, MPH (Department of Cardiovascular and Thoracic Surgery, University of Louisville, Louisville, KY, USA) for participating in these experiments. The authors thank Clara Banas for her helpful review of our article. This study was funded by author Gretel Monreal and the Department of Cardiovascular and Thoracic Surgery at the University of Louisville (Louisville, KY, USA). GM, SK, JH, and MS are investigators on a NIH grant (R44HL144214) with Inspired Therapeutics unrelated to this project. GM is an investigator on a grant from Abiomed unrelated to this project. GM and SK were investigators on a Kentucky Academy of Science Athey Science Education and Outreach Grant unrelated to this project. GM, SK, JH, and MS were investigators on now-completed NIH grants R43HL149451 and R43HL152767 (Bionet Sonar) unrelated to this project. GM, SK, and MS were investigators on now-completed NIH grants all unrelated to this project: R43HL142385 (MAST), R43HL152894 (MAST), R43HL142337 (Cor Habere), R43HL152774 (RT Cardiac Systems), R43HLI44214 (Inspired Therapeutics). GM, SK, JH, and MS were investigators on a now-completed subcontract with CoRISMA MCS Systems Inc, unrelated to this project. GM and SK were investigators on a now-completed NSF EPSCoR grant unrelated to this project. SK is an investigator on a NIH grant (R01HL150346) unrelated to this project. SK was an investigator on a now-completed NIH grant (R43NS115226, Bionet Sonar) unrelated to this project. MS is a consultant with Magenta Medical and is on the advisory board of Medtronic. MS was the Editor-in-Chief of ASAIO Journal. GM is supported in part by a gift from Robert M. Prizant to the Legacy Foundation of Kentuckiana. JH has funding from the National Institute of Environmental Health Sciences (P30ES030283), National Center for Advancing Translational Sciences (1U18TR003787-01), National Heart, Lung, and Blood Institute (R01HL158779-01), the American Heart Association (23CSA1052735), National Institute of Allergy and Infectious Diseases (R01AI172873-01), and the National Institute of General Medical Sciences (P20GM155899-01) unrelated to this project. JH is a consultant for GE Healthcare, Medtronic, and Mindray, which are unrelated to this project. JH received research funding from Gilead Sciences, Mespere LifeSciences, GE Healthcare, and Potreo Medical, which are unrelated to this project.
AI Tool Statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Original Source Article
↑Monreal, G., Koenig, S. C., Huang, J., and Slaughter, M. S. 2024. Anatomical and hemodynamic characterization of totally artificial hearts. ASAIO J. 70:338–47. doi: 10.1097/MAT.0000000000002209
References
[1] ↑ Monreal, G., Koenig, S. C., Huang, J., and Slaughter, M. S. 2024. Anatomical and hemodynamic characterization of totally artificial hearts. ASAIO J. 70:338–47. doi: 10.1097/MAT.0000000000002209
[2] ↑ Heidenreich, P. A., Bozkurt, B., Aguilar, D., Allen, L. A., Byun, J. J., Colvin, M. M., et al. 2022. AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145:e895–1032. doi: 10.1161/CIR.0000000000001063
[3] ↑ Jorde, U. P., Saeed, O., Koehl, D., Morris, A. A., Wood, K. L., Meyer, D. M., et al. 2024. The society of thoracic surgeons intermacs 2023 annual report: focus on magnetically levitated devices. Ann. Thorac. Surg. 117:33–44. doi: 10.1016/j.athoracsur.2023.11.004
[4] ↑ Monreal, G., Koenig, S. C., Kelley, J. F., Illg, J. J., Tamez, D., Kelley, M. S., et al. 2024. Early-stage Development of the CoRISMA Mechanical Circulatory Support (CMCS) System for heart failure therapy. Cardiovasc. Eng. Technol. 15:667–78. doi: 10.1007/s13239-024-00743-0
[5] ↑ Monreal, G., Koenig, S. C., Slaughter, M. S., Morello, G. F., Prina, S. R., Tompkins, L. H., et al. 2022. Feasibility testing of the Inspired Therapeutics NeoMate mechanical circulatory support system for neonates and infants. PLoS ONE 17:e0266822. doi: 10.1371/journal.pone.0266822