Abstract
Living in space is not as simple as living on Earth. The environment in space is harmful for humans. Astronauts experience weightlessness and are exposed to dangerous radiation. On top of that, astronauts live in a tiny area, far from their loved ones. All our organs are harmed by these factors. The heart, for example, starts to age much quicker in space than on Earth. This means that astronauts have a higher risk of heart disease after going to space. It is therefore important that we investigate why this happens so that we can prevent it. In the past, these studies were based on experiments using animals or humans. Today, we can create mini-hearts in the lab for our experiments instead. In this article, we will explain how we make mini-hearts and how they help us understand and prevent the heart’s aging in space.
Space Ages Our Hearts
Many people think it is exciting to go into space! Imagine swimming weightlessly on the International Space Station, cruising in a spaceship, or just seeing our home, planet Earth, from above. In the next few years, we will build a new space station around the moon and send the first humans to the moon since 1972. As if that was not enough, before 2040, the first human ever will set foot on Mars, and soon anyone who wants to go to space will be able to! But it is not risk free to stay in space. The deeper into space we go, the more dangerous it gets.
The heart is an important human organ. It is responsible for pumping the blood, which delivers energy to all the body’s parts. Naturally, the older we become, the less efficient and weaker our hearts get, and the slower we become (Figure 1). You might have noticed this in your grandparents. In space, this phenomenon is accelerated, meaning that our hearts become weaker more quickly in space compared to on Earth. It seems that the heart ages quicker in space.
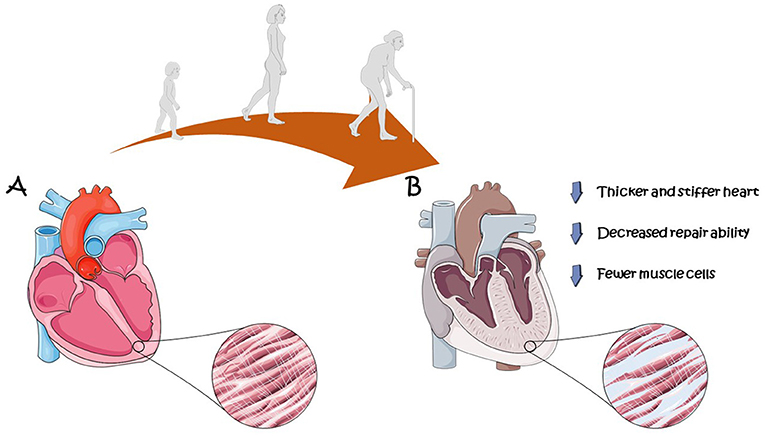
- Figure 1 - (A) A young heart compared with (B) an old heart.
- As we age, our hearts become less efficient. This is caused by several processes, such as the loss of muscle, stiffening of the heart, and a decreased ability to repair injuries. The circles show close ups of the cells of (A) a young human heart and (B) an old human heart. The red cells with stripes are heart muscle cells while the more blue cells are non-muscle cells (figure created using elements from Servier Medical Art; smart.servier.com).
Why Does Space Age the Heart?
There are several ways that space causes the heart to age. The first and most important reason is radiation. Radiation is invisible to our eyes but can be very dangerous. While not all radiation is dangerous (we use radiation to connect to the internet or make phone calls, for example) radiation in space is quite harmful, making it dangerous to stay in space for even a short time. When our cells are exposed to space radiation, they become damaged—particularly their DNA. When heart cells are damaged in this way, the risk of many heart diseases increases. Because of this, astronauts exposed to space radiation suffer from more cardiovascular diseases [1].
The second reason is weightlessness. While it might seem like a lot of fun to swim in the air or do effortless backflips, it is actually harmful to the body and organs. Being weightless means that the muscles do not need to work to support the body’s weight. This causes the astronaut’s muscles to slowly break down. The heart is also a muscle, so when gravity is not pulling the blood down toward the feet, the heart does not need to work as much to pump the blood around the body. This causes more blood to stay in the upper body compared to on Earth. Because of this, the heart’s shape becomes rounder and more similar to a ball. Some parts of the heart also become smaller and lose muscle tone [2].
The third reason space ages the heart is the loneliness and stress. It is difficult to send help into space, so astronauts are lonely and can usually only get help from each other, which can make them stressed. On top of that, spacecrafts are usually very small, with little space to move around, which makes them very stressful environments to be in. Being stressed and lonely for a long time can cause astronauts to become less motivated, weaker, and worse at teamwork. Astronauts are carefully selected to ensure that they can handle this stressful environment as best as possible [2].
Together, these three reasons cause the heart to age quicker in space [3]. If we want to send more humans into space and explore further into the galaxy, we must know how to stop this sped-up aging. Unfortunately, we still know very little about what happens to the heart deep in space, so we need to do more research on this topic.
How Can Researchers Study Aging in Space?
One common way to study organs is to perform experiments on animals. You can, for example, test medicines on animals or study what happens to a mouse’s heart when it goes into space. This does not work so well to study aging, for two main reasons. The first and most important reason is that animals’ organs are different from human organs. As you can imagine, a mouse heart is not the same as a human heart. This means that much of the research done on animals does not match what happens in the human body. For example, a medicine that treats heart disease in rats may not work for humans or may even be dangerous. Secondly, animal experiments can sometimes cause the animals to suffer.
To fix this, researchers can now create miniature human organs in a lab. We call these mini-organs organoids. Organoids represent real human organs better than animal organs do. Because of that, we can be more certain that a medicine that works on an organoid also works for humans. Researchers can also make organoids personalized. Since all humans are different, each person might react differently to a certain medication or environment. With personalized organoids, we can customize medication specifically for you, or tell you exactly how much your heart will age in space [4].
How to Build an Organoid
To build an organoid, researchers start with the smallest building blocks of the body, cells. When building a mini-heart, either heart cells or stem cells can be used. Stem cells are special cells that can turn into the different cell types of the body, so researchers can “program” them to become all the cells necessary to build a mini-heart. By instructing the stem cells to become heart cells, researchers can eventually form a mini-heart that beats. These beating mini-hearts are also called heart organoids [5].
The process of stem cells turning into other cells, such as brain cells or heart cells, is called differentiation. Differentiation is done in the lab by giving the stem cells specific nutrients and molecules. The specific combination they are given determines what type of cells the stem cells will turn into. So, researchers follow a very precise recipe of nutrients and molecules to form heart cells and mini-hearts [4].
First, researchers put stem cells together into a tiny ball. This ball is just a few hair strands wide but contains a few thousand stem cells. After the stem cell ball has formed, the very precise recipe of nutrients and molecules is followed. After a few days, hollow pockets form inside the ball and, at the same time, stem cells slowly turn into heart cells, which eventually start to beat. Within 1–2 weeks, a hollow beating ball of heart cells has formed. This is the mini-heart, and it is about 1–3 mm wide (Figure 2) [5].
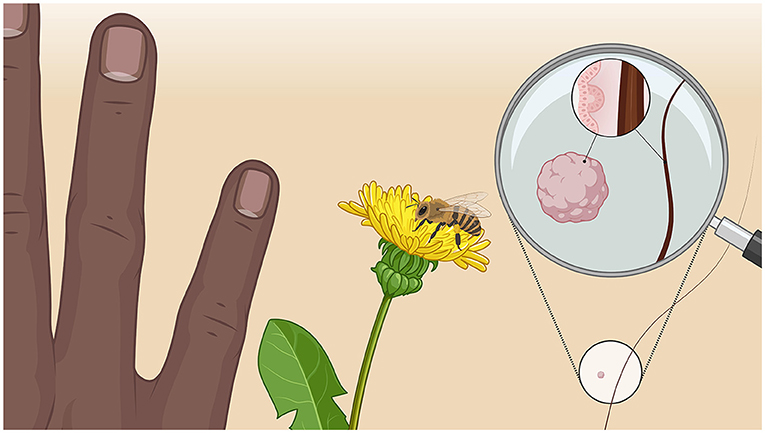
- Figure 2 - The size of a mini-heart compared to a hand, bee, and hair strand.
- The lower right circle shows the actual size of a mini-heart next to a human hair. In the magnification, you can see the mini-heart next to the human hair. The even closer magnification, above the mini-heart, shows the size of the cells of the mini-heart compared to the width of a human hair (figure created using Biorender; biorender.com).
Mini-hearts can also be created using 3D printing. Functional heart cells can be mixed into a liquid that can turn into a gel. The combination of cells and this liquid is called a bioink. By combining different cells with different liquids, different bioinks are created. Bioinks are then 3D printed in a specific shape and order to build a mini-heart [6].
The mini-hearts can also be placed into a training device that functions like a mini-gym. When mini-hearts are first formed, they are very weak. By putting pressure on the cells when they beat and giving them tiny electric shocks, the mini-heart can be trained to become stronger, just like our real hearts when we exercise. This is important if researchers want the mini-heart to mimic the human heart [7].
How Can Mini-Hearts Make Space Travel Safer?
By sending mini-hearts into space, researchers can study how the space environment affects human hearts and why the heart ages quicker in space. They can study how and why the ability of the heart to beat changes in space. They can also simulate space conditions (weightlessness, radiation, and stress) using machines and drugs on Earth. Space missions are very expensive and not very common, so performing an experiment on Earth before performing it in space can give researchers a lot of additional information.
Today, there is no specific way to prevent the heart’s quicker aging in space. With the help of organoids, mini-hearts in this case, researchers can study why our hearts age more quickly in space and how this aging might be prevented. With personalized mini-hearts, researchers will also be able to determine how much each person’s heart will age in space and how to best treat each individual. This research will help to make space travel safer for everyone in the future!
Glossary
Radiation: ↑ Invisible particles or waves that transfer energy. Highly energetic radiation can cause damage to our bodies.
Cardiovascular Disease: ↑ Diseases that affect the heart and/or vascular system
Organoid: ↑ A mini organ grown in the lab, often created from stem cells.
Stem Cells: ↑ Cells that have the capability to develop into several different cell types.
Differentiation: ↑ The process of a cell becoming more specialized. For example a stem cell turning into a heart cell.
Bioink: ↑ The combination of cells and a 3D printable liquid material that can solidify. This material needs to be able to support the growth and survival of the cells.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Vejbystrands Skola and Förskola, and the students of grade 4–6 for valuable input during the making of the figures. This work was supported by an ESA PRODEX grant IMPULSE (PEA4000134310) and the EIC Pathfinder Open project PULSE (Grant Agreement number 101099346).
References
[1] ↑ Rehnberg, E., Quaghebeur, K., Baselet, B., Rajan, N., Shazly, T., Moroni, L., et al. 2023. Biomarkers for biosensors to monitor space-induced cardiovascular ageing. Front. Sens. 4:1015403. doi: 10.3389/fsens.2023.1015403
[2] ↑ Baran, R., Marchal, S., Garcia Campos, S., Rehnberg, E., Tabury, K., Baselet, B., et al. 2022. The cardiovascular system in space: focus on in vivo and in vitro studies. Biomedicines. 10:59. doi: 10.3390/biomedicines10010059
[3] ↑ Hughson, R. L., Helm, A., and Durante, M. 2018. Heart in space: effect of the extraterrestrial environment on the cardiovascular system. Nat. Rev. Cardiol. 15:167–80. doi: 10.1038/nrcardio.2017.157
[4] ↑ Clevers, H. 2016. Modeling development and disease with organoids. Cell. 165:1586–97. doi: 10.1016/j.cell.2016.05.082
[5] ↑ Hofbauer, P., Jahnel, S. M., Papai, N., Giesshammer, M., Deyett, A., Schmidt, C., et al. 2021. Cardioids reveal self-organizing principles of human cardiogenesis. Cell. 184:3299–317.e22. doi: 10.1016/j.cell.2021.04.034
[6] ↑ Sun, W., Starly, B., Daly, A. C., Burdick, J. A., Groll, J., Skeldon, G., et al. 2020. The bioprinting roadmap. Biofabrication. 12:022002. doi: 10.1088/1758-5090/ab5158
[7] ↑ Ronaldson-Bouchard, K., Ma, S. P., Yeager, K., Chen, T., Song, L., Sirabella, D., et al. 2018. Advanced maturation of human cardiac tissue grown from pluripotent stem cells. Nature. 556:239–43. doi: 10.1038/s41586-018-0016-3
