Abstract
You probably have a favorite ice cream flavor, but do you really know how you perceive it? In this article, you will see that flavor is the result of your brain integrating information from several sensory systems. Your tongue gives you information about the taste of food. But your sense of smell also plays an important role when you breathe air out while eating. Yes, when you breathe out, not in! This knowledge will help you to understand why food lacks flavor when you are sick and your nose is stuffy or runny.
Have you ever noticed how flavorless food is when you have a cold and your nose is running? If your parents give you a hot bowl of chicken soup, you might not perceive the chicken flavor at all! To better understand what happens when you are ill, we will first explain what happens when you are well: what is flavor?
Flavor: A Combination of Several Senses
Food is composed of various molecules that are released when you put it in your mouth and chew. Some of these molecules are detected by taste receptors, which are mostly found on the surface of taste cells located within the papillae, the little bumps you can see on your tongue. For now, think of food molecules as “keys” and receptors as “locks” that let cells know what is going on in the external world. Taste receptors therefore tell you how food tastes: sweet, salty, sour, bitter, or savory.
However, taste is just a small component of your perception of flavor [1]. So, what is the dominating component? Some food molecules do not stay in the mouth, they can also travel to the nose! Olfaction, the sense of smell, can be divided into two routes, called orthonasal and retronasal. Orthonasal olfaction occurs when you inhale (breathe air in)—odor molecules that are in the air flow into your nose. Retronasal olfaction is the route that plays an important role when you eat food. When you exhale (breathe air out), some molecules in your mouth are carried toward the back of your nose via your throat (Figure 1). You can do a simple test to understand the role of olfaction in flavor. Take a piece of chocolate, pinch your nose, and then put the chocolate in your mouth. You should taste the sweetness of the chocolate, but not the full flavor. When it has melted, unpinch your nose. You should now experience the added odor component. Similar to the taste system, some food molecules are detected by olfactory receptors on olfactory receptor cells located in the olfactory epithelium inside the nose [2].
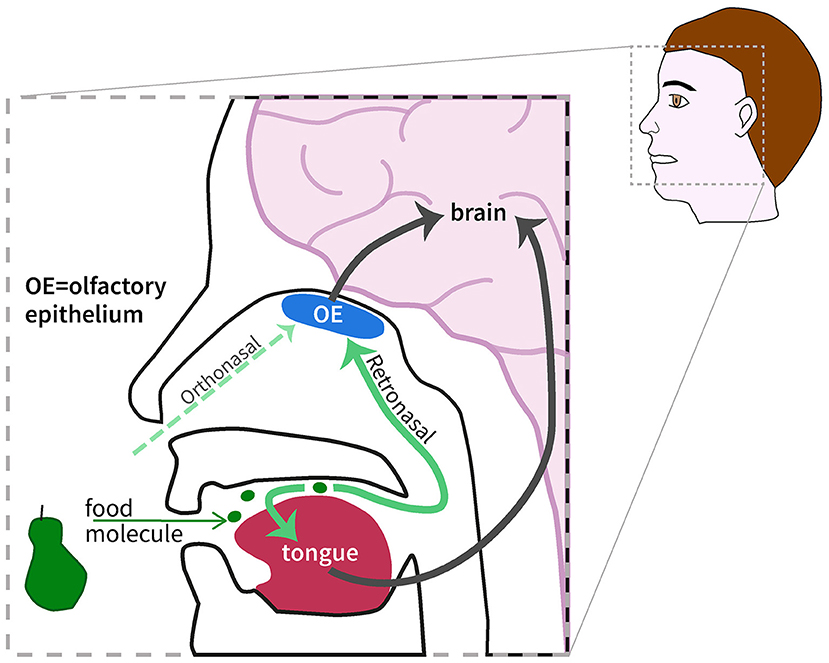
- Figure 1 - Combining smell and taste: when you eat, different molecules are released from the food in your mouth.
- These molecules can be detected by special cells on the tongue (taste of the food), or travel to the back of the nose and be detected by cells in the olfactory epithelium (smell of the food). These cells then send the different pieces of information to other cells, up to cells in the brain, which integrates them into the flavor we perceive.
But what exactly happens when a food molecule is detected either by a taste receptor or by an olfactory receptor? Detection means that the molecule binds to the receptor or, to return to the simple “lock and key” analogy, that the molecule is the right key that fits into the lock. The binding of the molecule activates the cell on which the receptor is located, and this results in the release of signaling molecules that are detected by specific receptors on brain cells. The brain then integrates the information from the various senses, giving rise to the perception of flavor (Figure 2) [3].
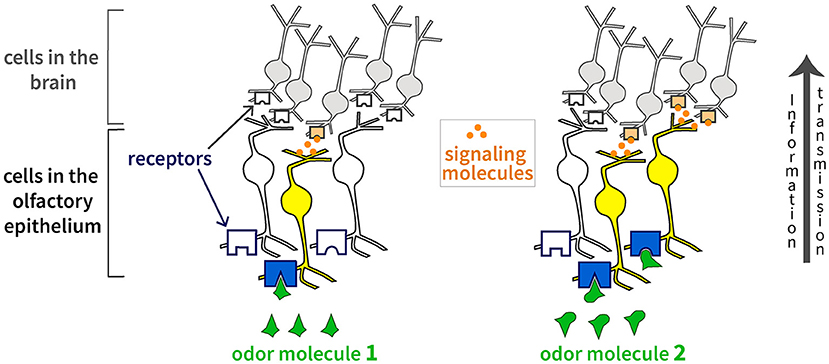
- Figure 2 - The binding of an odor molecule (the “key”) to a receptor (the “lock”) activates the cell on which the receptor is located.
- The cell releases signaling molecules to communicate the information to other cells. Since different odor molecules fit into different receptors, each odor activates a unique combination of olfactory receptor cells (color-coded in yellow).
Humans have about 400 types of olfactory receptors, while dogs have about 800 and rats about 1,200. However, this does not mean that humans can only detect 400 odors. Why is this? Each olfactory receptor cell has several olfactory receptors on its surface, but they all belong to the same type. Different odor molecules can bind to the same type of olfactory receptor, and one molecule can bind to several types of receptors. Therefore, each odor is coded by a unique combination of activated olfactory receptor cells (Figure 2) [[4]; see also this Frontiers for Young Minds article). This is something difficult to calculate, but researchers currently estimate the number of odors humans can discriminate to be at least 10,000. Concerning taste, it seems that humans have one or two types of receptors per taste molecule, except for bitter molecules, for which 25 different kinds of receptors have been found [5]. However, it is still unclear if there is only one type of receptor per cell.
The flavor of food can be influenced by other senses, for example by what you feel in your mouth or by what you see with your eyes. Try a simple experiment with a friend or family member: pour some apple juice into two clear glasses. Add a few drops of food coloring to each glass: green to one and red to the other. Give the two glasses to your friends, without telling them that it is apple juice, and give them a glass of water to drink between sips. Ask them what they think of the drinks: which one do they prefer? What do they think they are drinking? Humans rely heavily on vision, and what we see creates expectations about what we will sense in our mouth. This is why most people will find that the two colored drinks do not have the same flavor. You can then repeat the experiment with the eyes closed to see how it affects the result.
Flavor Sensations During Sickness
Let us return to when we experience illness due to pathogens, tiny harmful organisms causing for example the common cold or COVID-19. Now you know that when food lacks flavor, it must be because something is going wrong with your sense of taste and/or your sense of smell. But what exactly is going on? We will explore some of the things that might be happening with your sense of smell, as it plays a dominant role in flavor [6]. However, keep in mind that pathogens can also attack the mouth and interfere with the function of taste cells.
First, the olfactory receptors can be harder to reach for the odor molecules. If you could take a close look at the inside of the nose, you would see that it contains folded structures called turbinates (Figure 3A). The turbinates contain bone tissue and blood vessels, and they are covered by a layer of mucus. Mucus is the substance that comes out of your nose when you have a cold, but it is also present in other parts of your body. Mucus filters the air and protects us from pathogens. But sometimes, pathogens manage to get into our bodies. Fortunately, we have an internal defense system (the immune system) with specialized cells that fight these intruders and eliminate them. To make it easier for the “defense cells” to reach the nose, the blood vessels in the turbinates become wider and more leaky (this is called the inflammatory response). As a side-effect, the swelling of the turbinates can block air circulation (Figure 3A), and fewer odor molecules can reach the olfactory epithelium. More mucus is also produced to trap more pathogens, and the composition of the mucus changes. But again, this makes the molecules’ journey up to the olfactory receptors more difficult.
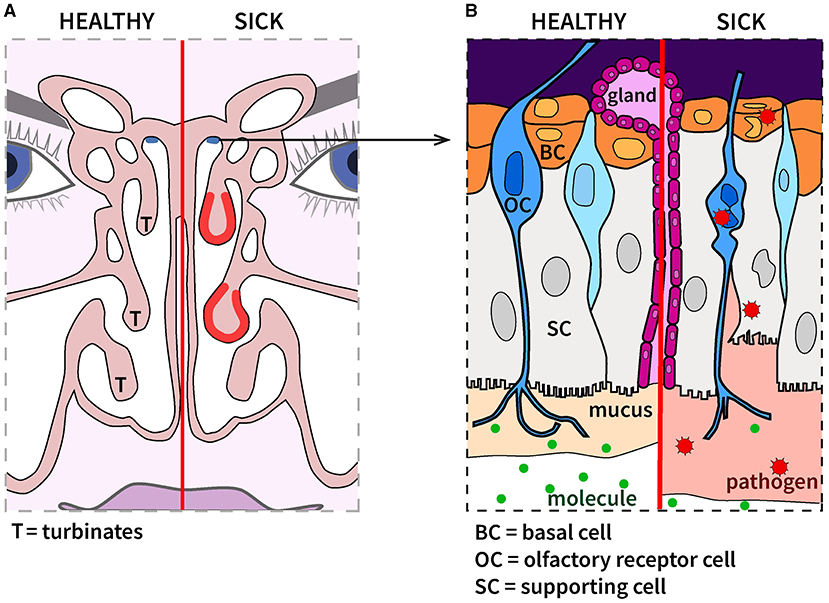
- Figure 3 - (A) During sickness, turbinates in the nose can become swollen, blocking the circulation of odor molecules.
- (B) Invading organisms (pathogens) can damage the olfactory epithelium, impairing the detection of odor molecules. Luckily, basal cells can produce new cells and repair the damage.
Second, pathogens can infect the cells within the olfactory epithelium. This can lead to the damage and/or death of these cells and temporarily impair your sense of smell (Figure 3B). In addition to the olfactory receptor cells described above, there are two other important types of cells in the olfactory epithelium: the supporting cells and the basal cells. The supporting cells are essential for the proper functioning of the olfactory epithelium, and one of their roles is to produce mucus together with gland cells. The basal cells belong to the family of stem cells and have the amazing ability to transform into supporting cells or olfactory receptor cells within weeks. That is why you can recover your sense of smell. Thanks to the basal cells, cells damaged by pathogens are replaced!
Take-Home
In conclusion, the next time you are ill and cannot really tell what you are eating (or drinking), remember the following:
• Some food molecules are detected by taste receptors on the tongue, and some reach the back of the nose where they are detected by olfactory receptors.
• Our perception of flavor is the result of our brain combining information from several senses.
• Pathogens can affect our sense of smell and/or taste, for example by altering the interaction between receptors and food molecules.
Glossary
Molecule: ↑ The building blocks of all matter are atoms, which combine to form molecules.
Receptor: ↑ A molecule or combination of molecules that can interact with a specific set of molecules, and the interaction triggers some changes in the cell where the receptor is located.
Cell: ↑ The smallest building block of living things such as animals and plants. Different cell types have different shapes and play different roles.
Olfaction: ↑ Also known as the sense of smell, it is the ability to gather information about odors in the environment. Odors are composed of odor molecules.
Retronasal Olfaction: ↑ Smelling while breathing out. The odor molecules which originate from the food in the mouth reach the nose through the respiratory tract.
Olfactory Epithelium: ↑ A group of cells located in the back of the nose, specialized in the detection of odor molecules.
Pathogens: ↑ Tiny organisms which can invade the body and alter its proper functioning.
Stem Cell: ↑ Cells that can generate new stem cells and become specific types of cells when needed.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Véronique Bernard and Ava Fleischmann for feedback on the manuscript.
References
[1] ↑ Rozin P. 1982. “Taste-smell confusions” and the duality of the olfactory sense. Percept. Psychophys. 31:397–401. doi: 10.3758/BF03202667
[2] ↑ Buck, L., and Axel, R. 1991. A novel multigene family may encode odorant receptors: a molecular basis for odor recognition. Cell. 65:175–87 doi: 10.1016/0092-8674(91)90418-X
[3] ↑ Shepherd, G. 2011. Neurogastronomy - How the Brain Creates Flavor and Why it Matters. New York: Columbia University Press.
[4] ↑ Malnic, B., Hirono, J., Sato, T., and Buck, L. B. 1999. Combinatorial receptor codes for odors. Cell. 96:713–23. doi: 10.1016/S0092-8674(00)80581-4
[5] ↑ Adler, E., Hoon, M. A., Mueller, K. L., and Zuker, C. S. 2000. A novel family of mammalian taste receptors. Cell. 100:693–702. doi: 10.1016/S0092-8674(00)80705-9
[6] ↑ Rebholz, H., Braun, R. J., Ladage, D., Knoll, W., Kleber C., and Hassel, A. W. 2020. Loss of olfactory function—early indicator for Covid-19, other viral infections and neurodegenerative disorders. Front. Neurol. 11:569333. doi: 10.3389/fneur.2020.569333
