Abstract
Do you get red and itchy rashes that just do not seem to go away? You may have atopic dermatitis, sometimes called eczema, the most common skin disease in children and teenagers. In this article, we describe how to recognize eczema and what causes it. Then we discuss the various treatments for eczema and strategies to help prevent it. Finally, we discuss the impact eczema can have on a person’s life.
What Is Eczema and What Are the Symptoms?
Eczema, or what doctors call atopic dermatitis, is a disease in which the skin is dry and itchy, with a red, bumpy rash. This disease affects children and teens much more often than adults. In the United States, almost 10 million children have eczema. That is 13% (or 13 in 100) of American kids! Most children get eczema before they are 5 years old [1]. The good news is that, in more than half of the kids who get it, eczema goes away or gets much better by the time they are teenagers.
The symptoms of eczema can vary between people. Symptoms most often include dry, itchy skin with redness, blisters, or sores. The skin can also be scaly, which means that the skin is so dry that it cracks and flakes off. Eczema can happen on any part of the body. It usually occurs on the hands, feet, folds of the elbows, the backs of the knees, and on the face, neck, and chest. Sometimes, people are so itchy that they scratch a lot. This causes the skin to become thick and rough, a process called lichenification. Eczema is a chronic condition, meaning that it comes and goes, but people can have it for a long time.
What Causes Eczema?
Healthy skin protects the body from the outside world. When people have eczema, their skin is dry, and sometimes the skin gets cracks and breaks in it. Germs or other irritating things from the environment can then get into the skin. This activates the immune system, which is the part of the body that fights against diseases. The immune system fights back, but sometimes it fights back too much! When this happens, it can make the skin red and itchy, a process called inflammation (Figure 1).
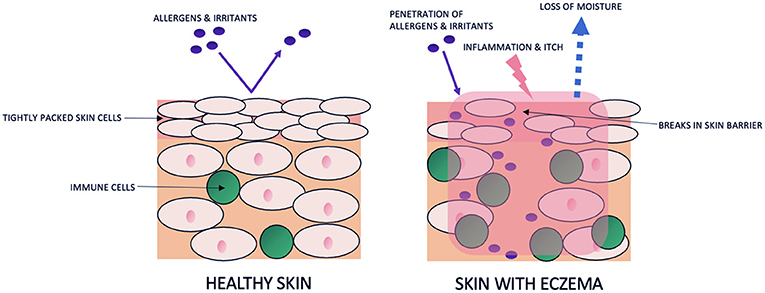
- Figure 1 - Healthy skin vs. skin with eczema.
- The top layer of the skin is made of tightly packed cells that keep allergens and irritants out and moisture in. When skin has eczema, the tightly packed cells are damaged, and the skin barrier is broken. Allergens and irritants get into the skin, and moisture is lost. The number of immune cells increases in response to the allergens and irritants. The skin becomes red, dry, and itchy though the processes of inflammation and water loss (original figure by authors).
Why do people get eczema? Your genes, which carry the information that determines your traits and characteristics, and factors in the environment can both play a part. Some people with eczema have a permanent change, or mutation, in their genes, which makes their bodies unable to form a healthy skin barrier [2]. When people have this mutation, eczema can develop earlier and be more severe. Eczema is also a part of a family of diseases called atopic diseases, which also includes asthma and food and environmental allergies. Some people are more likely to get eczema than others. Doctors found that, if both parents have an atopic disease, their child is 3–5 times more likely to have one as well [3]. Also, some doctors have found that kids who live in cities may get eczema more than kids who live in rural areas [1]. Other causes of eczema include types of soap, sweaty skin, dry wintertime air, scratchy fabrics, and other things that irritate skin. If you have eczema, it is important to avoid the specific products, clothes, and other things that can trigger it!
How Can We Treat and Prevent Eczema?
Moisturizers—like lotions, creams, and ointments—are the most important things to use when you have eczema. They keep the skin from getting dry and protect it from cracking. Scientists and doctors have proven that moisturizers can help with the itchiness and redness of eczema. Sometimes lotions and creams can cause stinging if applied to cracked skin. If that is the case, an ointment will work without stinging. The good news is that it does not matter what moisturizer you use. They all work great! So, you can pick your favorite. The important thing is to make sure you use enough. Dermatologists, or skin doctors, came up with a clever way to measure moisturizer. It is called the fingertip unit (FTU) [4]. The FTU is the amount of moisturizer produced from a tube that covers from the tip of an adult’s pointer finger to the closest skin crease (Figure 2). The amount of fingertip units needed to cover the entire body with moisturizer are displayed in Figure 2. Newborn babies only require 5 FTUs per application of moisturizer on their whole body. Children ages 1–2 need 10 FTUs, children ages 3–5 need 13 FTUs, children ages 6–11 need 17.5 FTUs, and teenagers who are almost at their adult size need 21.5 FTUs or more.
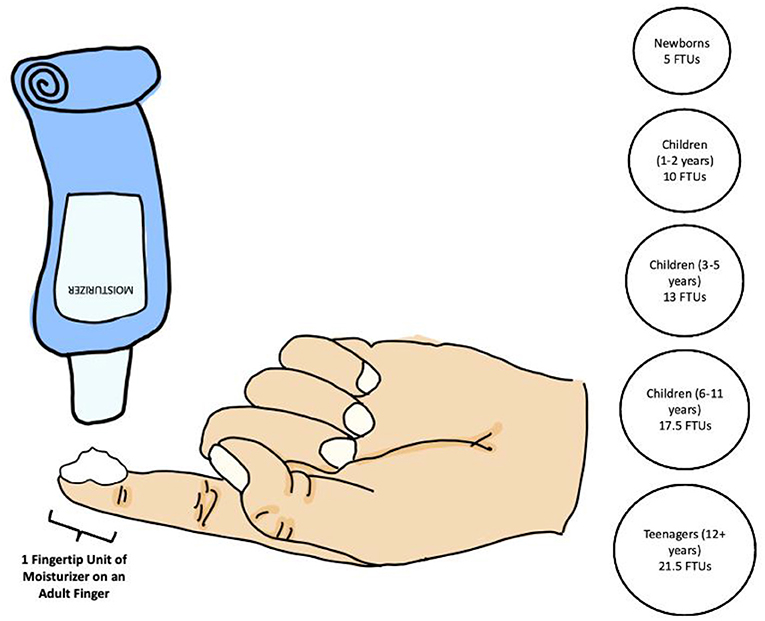
- Figure 2 - What is a fingertip unit?
- The fingertip unit (FTU) is the amount of moisturizer produced from a tube that covers the tip of an adult’s pointer finger to the closest skin crease. An adult’s finger should always be used to measure FTUs. The number of FTUs recommended by age is shown in the circles [4] (original figure by authors).
Moisturizing is also a part of an eczema treatment called wet-wrap therapy. This technique consists of first putting on moisturizer and then covering the skin with damp clothing or bandages. Then a dry layer of clothing or bandages goes on the outside. Some children do this before going to bed, to help make their skin less itchy while they sleep. Wet-wrap therapy helps the moisturizer get deep into the skin and helps prevent scratching.
If moisturizer is not enough, a doctor may prescribe medicines to help with eczema. Corticosteroids are medicines that can help calm down inflammation. There are many different kinds of corticosteroids that range from mild to strong, and a doctor can decide which one is best for each patient. There are other types of drugs that also work to stop the immune system from going into overdrive. These medicines are applied to the skin like moisturizers, as creams or ointments. If medicines applied to the skin and moisturizer do not control the eczema enough, doctors might recommend other treatments like phototherapy. Phototherapy, also called light therapy, uses a special machine that produces specific waves of light that can help treat widespread eczema. In severe cases, doctors may also consider medications that people can take by mouth or as a shot. Scientists recently created a new medicine called dupilumab that has helped kids with severe eczema. It is an injection, or shot, given every few weeks and it works by blocking the part of the immune system that causes eczema. Teens and children 6 years or older can use it, and it has helped a lot of people keep their eczema under control [5].
There are ways to prevent eczema or to keep it from getting worse. First, it is important to moisturize your skin often. Avoid hot showers and baths to help keep the skin from getting itchy. Also, avoid scratchy materials like wool. Finally, ask the people who take care of you at home not to use harsh and smelly soaps or laundry detergents.
How Does Eczema Impact a Person’s Life?
Eczema can have a large impact on a person’s life. The itchiness of eczema is severe. It can be so itchy that it keeps people awake at night. Many patients suffer from sleep loss and sleep disruption, which makes them more tired and distressed during the day. The itchiness can also make it hard to concentrate on work or school. Also, if bacteria or viruses get under the skin, sometimes they can cause an infection. People with eczema are more likely to get skin infections than people with healthy skin. If infection happens, a doctor will treat the infection with antibiotics. Eczema is a chronic condition, which means it usually lasts more than 1 year and requires ongoing medical attention. It can cycle between getting better and getting worse. Luckily, most kids with eczema usually do not have it anymore by the time they are teenagers. However, some people have eczema when they get older. This means that they need to continue seeing the doctor to help them take care of their skin. Finally, people with eczema can also suffer from loss of confidence because of their skin. They can be nervous or sad because they are in pain or feel badly about looking different [6]. Keep this in mind if someone you know has eczema and be kind to them.
If you live with eczema, there is good news! Your self-esteem does not have to suffer because of your eczema. Many children and teens have eczema. There are support groups that help people with eczema, and you can get involved with them in person or on social media. Also, chances are you may know someone else in your life with eczema. That person can relate to what you are experiencing. Doctors are here to help people with eczema, and scientists are working hard to discover new treatments. Understanding the basics of eczema and how to prevent it can keep your skin healthy, and now you can help others learn about eczema too!
Glossary
Lichenification: ↑ The process of skin becoming thick and leathery after being scratched or rubbed repeatedly.
Chronic Condition: ↑ A disease or illness that lasts more than 1 year, can cycle between getting better and getting worse, and requires ongoing medical attention.
Inflammation: ↑ A bodily response to injury or disease in which heat, redness, and swelling are present.
Atopic: ↑ Sensitive to allergens and irritants in the environment.
Dermatologist: ↑ A doctor that specializes in conditions involving the skin, hair, and nails.
Fingertip Unit: ↑ The amount of moisturizer produced from a tube that covers the tip of an adult’s pointer finger to the closest skin crease. An adult’s finger should always be used to measure FTUs. FTUs are a useful way to explain how much of a cream or ointment should be used on the skin.
Corticosteroid: ↑ Medicines that can help calm down inflammation.
Phototherapy: ↑ Also called light therapy, it uses a special machine that produces specific waves of light that can help treat widespread eczema and other skin conditions.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Shaw, T. E., Currie, G. P., Koudelka, C. W., and Simpson, E. L. 2011. Eczema prevalence in the United States: data from the 2003 National Survey of Children’s Health. J. Invest. Dermatol. 131:67–73. doi: 10.1038/jid.2010.251
[2] ↑ Palmer, C. N. A., Irvine, A. D., Terron-Kwiatkowski, A., Zhao, Y., Liao, H., Lee, S. P., et al. 2006. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat. Genet. 38:441–6. doi: 10.1038/ng1767
[3] ↑ Kuster, W., Petersen, M., Christophers, E., Goos, M., and Sterry, W. 1990. A family study of atopic dermatitis: clinical and genetic characteristics of 188 patients and 2,151 family members. Arch. Dermatol. Res. 282:98–102. doi: 10.1007/BF00493466
[4] ↑ Eichenfield, L. F., Boguniewicz, M., Simpson, E. L., Russell, J. J., Block, J. K., Feldman, S. R., et al. 2015. Translating atopic dermatitis management guidelines into practice for primary care providers. Pediatrics. 136:554–65. doi: 10.1542/peds.2014-3678
[5] ↑ Cork, M. J., Thaçi, D., Eichenfield, L. F., Arkwright, P. D., Sun, X., Chen, Z., et al. 2021. Dupilumab provides favourable long-term safety and efficacy in children aged ≥ 6 to < 12 years with uncontrolled severe atopic dermatitis: results from an open-label phase IIa study and subsequent phase III open-label extension study. Br. J. Dermatol. 184:857–70. doi: 10.1111/bjd.19460
[6] ↑ Yaghmaie, P., Koudelka, C. W., and Simpson, E. L. 2013. Mental health comorbidity in atopic dermatitis. J. Allergy Clin. Immunol. 131:428–33. doi: 10.1016/j.jaci.2012.10.041