Abstract
Many skin conditions are dangerous, and some can even be life threatening. However, there are also many skin conditions that are not physically harmful but can negatively impact a person’s thoughts, feelings, or self-confidence. In this article, we discuss one of those skin conditions, called lichen nitidus. This condition is more common in kids and young adults. When people have lichen nitidus, they develop many small, shiny, smooth bumps on their bodies. These bumps can sometimes be itchy. Often, doctors do not know why people develop this disease. Although there is no cure for lichen nitidus, the good news is that it tends to go away on its own, without any treatments.
What Is Lichen Nitidus?
Did you know that the skin is the largest organ of the body? Many skin conditions are dangerous, and some can even be life threatening. However, many other skin conditions are not physically harmful but can negatively impact a person’s self-confidence. Lichen nitidus is one such condition. It can severely decrease a person’s quality of life, especially if it involves skin that is easily visible to other people [1]. People with lichen nitidus develop many small, shiny, skin-colored bumps on their bodies (Figure 1). These bumps can sometimes be itchy. In people with darker skin, the bumps caused by lichen nitidus can often appear lighter than the person’s skin color, or even white (Figure 2).

- Figure 1 - Small, shiny, smooth bumps on the chest of a patient with lichen nitidus.

- Figure 2 - Lichen nitidus in a patient with a darker skin tone.
- The bumps can appear lighter than the surrounding skin.
Why Do Some People Get Lichen Nitidus?
Lichen nitidus is more common in kids and young adults, although it can also be seen in older people [1]. It is not well understood why this condition occurs more often in children than it does in adults. Lichen nitidus can last several months or several years, and there is no way for doctors to predict why some people suffer from this disease longer than others. Often, doctors cannot explain why a person develops lichen nitidus. The cause of this skin disease is not known, but doctors think that it could be due to skin irritation that occurs over a long time [1]. While lichen nitidus is often only present on a specific area of the body, some people can have large areas of skin affected, making it impossible to cover the disease with clothing. Lichen nitidus has also been linked to other medical conditions that are not related to the skin at all, including diseases of the gut, such as Crohn’s disease [2]. While this relationship is not completely understood, it probably has to do with changes in a person’s immune system that send it into “overdrive,” causing it to attack parts of the person’s own body (like the gut or the skin) [3].
How Do We Diagnose Lichen Nitidus?
At first glance, lichen nitidus can look like other common skin conditions involving the immune system, such as flat warts or eczema. When a dermatologist thinks that a person may have lichen nitidus, the doctor can choose to perform a biopsy. A biopsy is a procedure that takes a small piece of the patient’s skin, so that it can be examined under a microscope. A microscope is like a powerful magnifying glass, and it allows the doctor to see exactly what is happening in the skin. When a doctor uses a microscope to look at a skin biopsy from an area with lichen nitidus, a pattern that resembles a claw clutching a ball is often seen (Figure 3) [1]. Although, doctors do not know why this pattern occurs, it is very unique to the disease. A biopsy can often confirm that a patient has lichen nitidus, but it is not always required—especially if the patient’s dermatologist is fairly certain the patient has the disease. A dermatologist may choose to pursue a biopsy if many parts of the patient’s body are involved, or if the disease has been present for many years without going away.
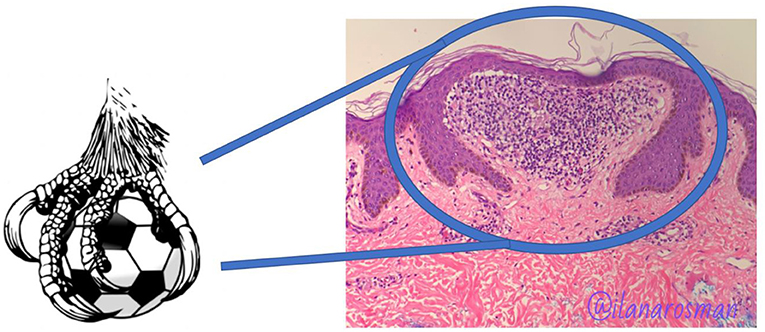
- Figure 3 - When skin biopsies taken from patients with lichen nitidus are examined using a microscope, the cells in the skin can often resemble a claw clutching a ball.
- Pathology slide courtesy of Dr. Ilana Rosman.
Treatment
Unfortunately, there is no cure for lichen nitidus. If a patient experiences lots of itchiness from the disease, a dermatologist can prescribe a special cream called a steroid [4]. Steroids can decrease itchiness by reducing inflammation and irritation. If people have lichen nitidus covering their entire bodies, special light treatments can often help [4]. The good news is that lichen nitidus usually goes away on its own, without any treatment from a dermatologist. However, until that happens, people with this disease are often very self-conscious of their skin and may be worried because they do not know when (or if!) it will get better.
In conclusion, lichen nitidus is a physically harmless skin disease, but one that can have a very significant impact on those affected by it. It is important to recognize the burden that skin diseases such as lichen nitidus can have on people, especially children [5]. If you think that you may have lichen nitidus, it is important to see a dermatologist to confirm the diagnosis and discuss treatment options.
Glossary
Crohn’s Disease: ↑ An inflammatory disease involving any part of the gut, from the mouth to the anus.
Immune System: ↑ A specialized body system designed to protect the body from infections or toxins.
Flat Warts: ↑ A common skin condition caused by a virus that involves flat bumps located anywhere on the body, but most commonly on the hands and feet.
Eczema: ↑ A common skin condition that causes a red, itchy rash to appear on the body. It is due to problems with regulation of the body’s immune system.
Dermatologist: ↑ A doctor who focuses on the skin, hair, and nails, and is trained to care for people with skin conditions.
Biopsy: ↑ A procedure that a dermatologist can perform to sample a patient’s skin, to confirm the presence or absence of a specific skin disease.
Inflammation: ↑ A condition in which a part of the body becomes irritated or painful due to a long-lasting injury or infection.
Conflict of Interest
JR is an inventor on use patents for targeting CXCR3 (0#15/851,651) and IL15 (# 62489191) for the treatment of vitiligo. WD is a consultant for Eli Lilly and TWi Biotechnology, has research funding from Pfizer, and receives licensing fees from EMD/Millipore/Sigma in unrelated work.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Dr. Ilana Rosman for allowing us to use her pathology slide in this manuscript.
References
[1] ↑ Schwartz, C., and Goodman, M. B. 2022. Lichen nitidus. In: StatPearls. Treasure Island, FL: StatPearls Publishing. Available online at: https://www-ncbi-nlm-nih-gov.neomed.idm.oclc.org/books/NBK551709/ (accessed August 20, 2022).
[2] ↑ Scheinfeld, N. S., Teplitz, E., and McClain, S. A. 2001. Crohn’s disease and lichen nitidus: a case report and comparison of common histopathologic features. Inflamm. Bowel. Dis. 7:314–8. doi: 10.1097/00054725-200111000-00006
[3] ↑ Tilly, J. J., Drolet, B. A., and Esterly, N. B. 2004. Lichenoid eruptions in children. J. Am. Acad. Dermatol. 51:606–24. doi: 10.1016/j.jaad.2003.12.012
[4] ↑ Synakiewicz, J., Polańska, A., Bowszyc-Dmochowska, M., Zaba, R. W., Adamski, Z., Reich, A., et al. 2016. Generalized lichen nitidus: a case report and review of the literature. Postepy. Dermatol. Alergol. 33:488–90. doi: 10.5114/ada.2016.63890
[5] ↑ Al-Mutairi, N., Hassanein, A., Nour-Eldin, O., Arun, J. 2005. Generalized lichen nitidus. Pediatr. Dermatol. 22:158–60. doi: 10.1111/j.1525-1470.2005.22215.x