Abstract
Lots of people think that all dentists use little mirrors and loud tools like dental drills, but there is a type of dentist who does not need these things: the oral and maxillofacial pathologist. Can you believe that oral pathologists do not actually treat the teeth or even meet the patient? The oral pathologist receives a tiny piece of tissue from the patient, usually obtained through a small surgery called a biopsy. Then, a super tiny slice of that tissue is prepared and placed on a glass slide, and the oral pathologist looks at it through a microscope to figure out what disease the patient might have. This information is important to give the patient the right treatment. Do you want to learn more about this process and about the healthcare professional who does not meet the patient face-to-face? Keep reading to find out all these answers and more!
Dentists Do Much More Than Look at Teeth!
While many people imagine dentists using mouth mirrors and noisy tools like drills and suction tubes, there is one type of dentist who does not rely on any of these items: the oral and maxillofacial pathologist. These dentists specialize in diagnosing diseases that affect the mouth, jaws, and surrounding areas through careful examination of tissue samples under a microscope. The word pathology comes from the Greek words “pathos”, which means suffering, and “logos”, which means study. In this article, we will explain how oral and maxillofacial pathologists (which we will call oral pathologist, for simplicity) are a critical part of the team of professionals that helps diagnose and treat oral diseases.
The dentists that look into patients’ mouths do not just take care of teeth—their job goes much further. They also check the health of the entire mouth, including the lips, tongue, cheeks, gums, palate, upper jaw, lower jaw, and even the salivary glands, among other parts. Various diseases can affect the mouth, showing up as lumps, swellings, unusual-colored spots, or small, painful sores. Dentists are professionals who can diagnose and treat these issues. So, the next time you visit the dental office, remember that dentists are experts on more than just teeth!
Dentists who work directly with patients are called clinical dentists, and they are trained to identify anything that looks unusual in the mouth. Clinical dentists include general dentists (dentists who can handle many basic dental issues) and specialists (dentists who focus on specific areas and have extra training for more complex problems), as orthodontists (who straightens teeth using braces or aligners), periodontists (who treats gum diseases), oral surgeons (who performs complex surgeries in the mouth), oral medicine specialists (who received additional training in the clinical diagnosis and management of oral problems and their relationship with systemic diseases), and others.
Exploring How Oral Diseases are Diagnosed
The process of diagnosing an oral disease usually begins in the clinical dentist’s office. The patient explains their concern while the dentist asks questions and examines the patient. During the questioning, the dentist asks about the patient’s medical history and about the history of the problem the patient is experiencing. Sometimes, just by talking to the patient and observing characteristics like age, race, gender, and habits, as well as details about the lesion (like location, size, color, texture, how long it has been there), the dentist can make a diagnosis and suggest treatment. However, additional tests are sometimes needed, such as blood tests, imaging tests (like X-rays and other types of medical imaging) and microscopic examinations. In these situations, making a diagnosis becomes a team effort involving various dental or medical specialties (Figure 1).
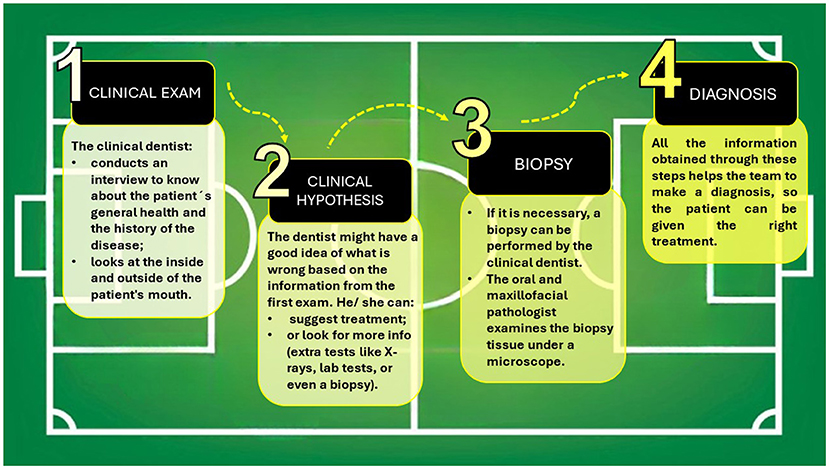
- Figure 1 - Diagnosing dental problems begins at the clinical dentist’s office.
- This dentist asks about the patient’s medical history and any mouth problems they are experiencing, and also does an exam. Sometimes, just by looking and asking questions, the dentist can figure out what is wrong and suggest treatment. Other times, the dentist asks for extra tests, and performs a biopsy. The oral pathologist examines the biopsy tissue under a microscope, helping to reach the diagnosis and guide the best treatment. The right diagnosis and treatment are the goals. The championship is won when the patient receives the best care.
The radiologist plays a crucial role in analyzing imaging tests, which are vital for understanding the exact location of a lesion, especially when it is inside the bone or below the surface where it cannot be seen directly. Many different kinds of lesions can look similar to the naked eye and on imaging exams. So, to accurately determine what is happening and reach the correct diagnosis, it is essential to understand the types of cells that are in the lesion, at the tiniest level. This is where a biopsy comes in [1].
A biopsy involves surgically removing part or all of the lesion to examine its microscopic structure. Biopsies can be performed by any clinical dentist. The tissue removed during surgery is placed in a special liquid to prevent it from breaking down, and then it is sent to the laboratory. In the lab, an oral pathologist examines the tissue sample to determine its composition and characteristics, helping to reach the diagnosis and guide the appropriate treatment.
The Microscope as an Oral Pathologist’s Tool
Oral and maxillofacial pathology is a special area of dentistry that focuses on understanding, identifying, and managing diseases in the mouth and face (https://ncrdscb.ada.org/recognized-dental-specialties). It is a bit different from other dental specialties [2]. The oral pathologist does not usually talk to patients directly or examine them like clinical dentists do. Instead, these dentists receive the biopsy samples from clinical dentists, which must be examined. In the lab, the biopsy fragment has to be prepared to be looked at under a microscope, which is like a super magnifying glass. Microscopes work by shining light through an object and making it bigger so it can be seen more clearly. If the object is too thick, the light cannot get through. That is why the biopsy tissue must be prepared by creating a glass slide with a very thin slice of the biopsy material, colored with special dyes. These dyes help the oral pathologist see tissues and cells that cannot be seen with the naked eye (Figure 2).
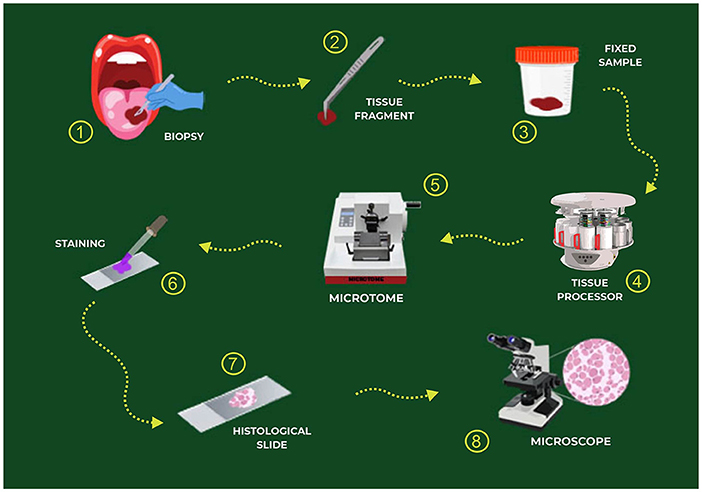
- Figure 2 - The steps of diagnosis, from the dental office to the oral pathology laboratory.
- The tissue from the biopsy (1, 2) is first fixed (3) so that it will not break down. Then, in the lab, the tissue is soaked in different substances in the tissue processor (4) to make it harder and easier to cut into very thin slices using a microtome (5). The transparent tissue slices are stained with special dyes (6) so that the cells and tissues can be seen (7). Finally, the sample can be examined under the microscope by the oral pathologist (8).
When oral pathologists look at tissues under a microscope, they are looking for specific signs that are different from those of healthy tissue. First, the oral pathologist must know what normal tissue looks like. Here are some things they check for: cell shape and size, the presence of unusual-looking cells, cell arrangement (such as disorganized cells) and color and staining (abnormal cells might stain differently with dyes than normal cells do). After examining the tissue’s cells and figuring out what is going on, the oral pathologist writes a report with the diagnosis. This report helps the clinical dentist decide on the best way to help the patient, kind of like putting together all the pieces of a puzzle to find the right treatment.
Communication is Key
Making a diagnosis is a team effort that involves clinical info and all the other tests we mentioned, so good communication is extremely important for success [3]. Since the oral pathologist does not meet the patient, all the info the dentist shares with the oral pathologist is valuable. This info includes the patient’s name, medical history, details about the problem, and what the dentist thinks might be going on. Likewise, the oral pathologist must talk clearly with the clinical dentist, giving them clear reports to help choose the best treatment. It is really important to avoid any confusion in this communication. Sometimes just a quick phone call can fix things. The oral pathologist does not have a crystal ball to predict the future, but they can see the disease through the crystal lens of the microscope! The patient’s future, like the diagnosis and treatment, depends on teamwork [3].
Imagine that oral health is like playing soccer, and healthcare professionals are the players on the team (Figure 3). Just like a soccer team works together to win, these healthcare professionals join forces as a team to figure out the problem, treat it, and help the patient get better. The oral pathologist plays a critical role in this process by helping to accurately diagnose the patient’s condition. Each professional has a special job on the team, but when they work together, they make a big difference in taking care of the patient!

- Figure 3 - The oral health team.
- Many kinds of professionals can be part of this special team, and each one brings their own skills to help diagnose, treat, and heal the patient. The team is put together based on the specific needs of each patient. Usually, the clinical dentist (a general dentist or a specialist, as an oral medicine specialist) acts as the coach, organizing the team and making sure everyone works together smoothly.
Glossary
Oral and Maxillofacial Pathologist: ↑ A dentist who specializes in diagnosing oral diseases through careful examination of tissue samples under a microscope.
Diagnosis: ↑ Figuring out exactly which sickness or condition a person has.
Clinical Dentist: ↑ A dentist who practices in a clinical setting, meaning they provide direct patient care. A clinical dentist can be a general dentist or a specialist.
Lesion: ↑ Anything that looks unusual, such as a spot or area in the body that hurts or looks different from the rest of the tissue.
Radiologist: ↑ A professional who uses X-rays and other imaging tools to see inside the body and help diagnose diseases.
Biopsy: ↑ A surgery to remove a small piece of tissue from the body to be examined under a microscope to check for disease.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AI Tools Statement
The English grammatical review of this article was assisted by ChatGPT, developed by OpenAI. The final content reflects the authors’ interpretation.
Acknowledgments
The authors would like to thank the São Paulo Research Foundation FAPESP (2021/097260) for the scholarship provided to LSB.
References
[1] ↑ Kumaraswamy, K. L., Vidhya, M., Rao, P. K., and Mukunda, A. 2012. Oral biopsy: oral pathologist’s perspective. J. Cancer Res. Ther. 8:192–8. doi: 10.4103/0973-1482.98969
[2] ↑ Chatterjee, K. 2018. Private practice of oral and maxillofacial pathology: a career option. J. Oral. Maxillofac. Pathol. 22:290–1. doi: 10.4103/jomfp.JOMFP_263_18
[3] ↑ Pérez-de-Oliveira, M. E., Heerden, W. V., Motta, A. C. F., Rodrigues-Fernandes, C. I., Romañach, M. J., Agostini, M., et al. 2022. The need for communication between clinicians and pathologists in the context of oral and maxillofacial diseases. Braz. Oral Res. 36:e008. doi: 10.1590/1807-3107bor-2022.vol36.0008