Abstract
Some people may experience an unusual and dramatic skin response to light exposure. This is called photosensitivity. Patients with photosensitivity may develop a rash, or symptoms such as swelling, itch, numbness, or pain after exposure to light. Symptoms usually follow exposure to sunlight, but artificial light sources such as light bulbs may also cause skin reactions. While photosensitivity is more common in adults, it also affects children, and certain photosensitivity conditions can begin in childhood. In this article, we discuss ways that kids can be sensitive to sunlight and the negative impact this can have on the mental health of affected individuals.
Can Kids Be Allergic To The Sun?
In most people, too much sun exposure can cause a sunburn. But some kids and adults may experience unusual and dramatic responses to light, beyond a typical sunburn. This is called photosensitivity. After exposure to light, patients with photosensitivity can develop a rash or symptoms such as swelling, itch, blisters, numbness, or pain. Symptoms usually follow exposure to sunlight, but artificial light sources such as light bulbs may also cause skin reactions [1]. While photosensitivity is more common in adults, it also affects children, and some types of photosensitivity specifically begin in childhood.
What Causes Photosensitivity In Children?
There are many causes of photosensitivity in children. Sometimes certain medications, like some antibiotics and a type of acne treatment, can cause a patient’s skin to be more sensitive and reactive to light. This is because chemicals in the medication reach the skin and are activated by light, leading to skin damage that can look and feel like a sunburn (Figure 1A) [1].
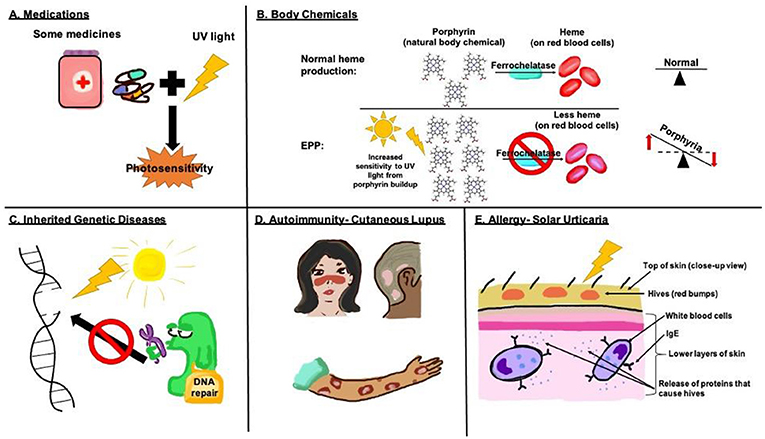
- Figure 1 - Causes of photosensitivity in kids.
- (A) Chemicals from certain medications can be activated by light and cause severe sunburns. (B) In erythropoietic protoporphyria, proteins called porphyrins build up in cells, resulting in photosensitivity. (C) Xeroderma pigmentosum is caused by problems with DNA repair following sunlight damage. This can result in blisters and skin cancer. (D) In cutaneous lupus, the immune system attacks skin tissue by mistake, resulting in various types of skin rashes. (E) Solar urticaria happens when UV light activates IgE proteins on white blood cells, producing itchy red hives on the skin.
In addition to external chemicals from medications, chemicals coming from inside the body can also cause photosensitivity. Some patients have a rare disorder caused by an abnormal buildup of certain chemicals, called porphyrins, in the body. The most common type of this disorder seen in childhood is called erythropoietic protoporphyria (EPP). It is caused by a deficiency in a special protein, called ferrochelatase, which is responsible for helping to convert porphyrins into heme, the substance that gives blood its red color (Figure 1B) [2]. Without enough ferrochelatase, porphyrins are not fully converted into heme, which results in excessive amounts of porphyrins in the body. These porphyrins build up under the skin and are highly sensitive to sunlight. When they absorb sunlight, this results in a reaction that causes severe pain. Patients may complain of a burning or stinging sensation within minutes of sun exposure. The average age at which patients with EPP develop symptoms is 4 years old [1]. These young children may cry when exposed to sunlight.
Photosensitivity in children is also caused by inherited disorders, which involve DNA damage and can be passed on from parents to children. DNA is an important molecule that acts like a blueprint that tells our bodies how to build cells and tissues. Sunlight contains a very high amount of energy and can cause DNA damage. Luckily, our cells are usually good at repairing the damage caused by sunlight. However, some patients have diseases in which DNA damage is not repaired properly after sun exposure because their cells lack the tools needed to fix this damage (Figure 1C). One example is xeroderma pigmentosum (XP). Kids with XP are extremely sensitive to the sun and can develop blisters, a rash, and eye problems after very minimal exposure to light [1]. Because they are unable to fix any DNA damage caused by light, problems like skin cancer can eventually happen.
Irregularities in the immune system can also cause photosensitivity in kids. The immune system is like the military, in that it is designed to protect the entire body from harmful invaders, or germs. Sometimes, instead of only killing germs, something goes wrong, and the immune system mistakenly begins to attack healthy cells in the body. This is called an autoimmune response. Cutaneous lupus erythematosus (CLE) is an example of an autoimmune disease in which the immune system attacks its own healthy skin. “Lupus” is the Latin word meaning wolf, and the disease has this name because the rash it causes sometimes resembles a wolf’s bite. Girls are almost three times as likely as boys to have CLE, with women between ages 15–44 being at greatest risk [3]. Sunlight plays a role in triggering or worsening CLE. There are different types of CLE, based on the location and appearance of the skin damage and how long that damage lasts. Some lupus rashes occur on the face and are butterfly shaped, others appear on sun-exposed areas as ring-shaped red sores with scaly edges, and still others occur on the scalp and can lead to hair loss (Figure 1D).
True sun allergy, called solar urticaria, is another cause of photosensitivity in kids. These kids develop hives, which are very itchy circular bumps, within 5 to 10 min of exposure to light [1]. Hives usually develop on areas that are directly exposed to the sun, such as the face and hands. Solar urticaria happens because the immune system overreacts to light, treating it as an invader and making an antibody protein called IgE, in a misguided attempt to protect the body. IgE causes immune cells to release chemicals into the bloodstream to defend against the “invader.” The release of these chemicals causes hives to develop (Figure 1E).
How Does Photosensitivity Affect Children?
Photosensitivity can affect children in different ways. Coping with the skin rashes may be difficult and children might feel embarrassed about their appearance, especially if they are teased or bullied. Patients with photosensitivity may also feel anxious about going out in the sun because they are worried about developing skin rashes. This anxiety can restrict their daily activities, limiting their time spent on outdoor hobbies or sports. Restricted activities may cause some patients to feel socially isolated and depressed [4]. It can be helpful for children with photosensitivity conditions to join support groups that can help strengthen their coping skills and reduce their anxiety levels. You can help your friends, peers or classmates who experience photosensitivity by being understanding and finding activities you can enjoy together.
How Do Doctors Help Patients With Photosensitivity?
Unfortunately, there is no permanent cure for photosensitivity. Doctors can help patients feel more comfortable when they have rashes, and can help prevent new skin rashes from developing.
First, it is especially important for patients with sun sensitivity to protect their skin from the sun, to avoid skin rashes [1]. Doctors encourage patients to use sunscreen with a sun-protection factor (SPF) of at least 30. SPF 30 means that it would take patients 30 times longer to burn than if they were not wearing sunscreen. Patients with photosensitivity are also recommended to wear protective clothing, such as hats and long sleeves. However, the skin produces vitamin D when it is exposed to sunlight, and vitamin D is essential for keeping our bones strong, among other functions. Avoiding the sun can lead to low vitamin D levels, so patients with sun sensitivity who avoid direct sunlight should have their vitamin D levels monitored by their doctors, and take supplemental vitamin D if their levels are too low [5].
Treatment of photosensitivity depends on the condition that is causing it. In patients who develop photosensitivity after using a certain medication, it is important to stop taking the medication whenever possible [1]. There are medications called corticosteroids that can be helpful in several types of photosensitivity disorders. Corticosteroids help weaken the immune system, to prevent it from causing skin irritation. In less severe cases, corticosteroid creams, ointments, and injections can be applied to the affected skin areas. For patients with more severe photosensitivity, corticosteroids can be taken by mouth, which affects the entire immune system, not just a particular area. For some forms of lupus, researchers have found that a drug originally created to treat a disease called malaria can be helpful, because of its effect on the immune system [5].
For patients with solar urticaria who develop hives after sun exposure, doctors might help them to gradually get their skin more used to sunlight, so that the body learns how to encounter sunlight without an overreaction of the immune system [1]. This is similar to the way allergy doctors help patients who are allergic to things like peanuts or cat dander: a small amount of the allergy-causing substance is given and, over time, the amount is slowly increased, so the immune system is trained not to react to the allergen. There are additional treatments for photosensitivity that are still being researched, including gene therapy to correct problems in DNA.
Summary
Photosensitivity can occur because of a variety of reasons. It can be triggered by medications, or conditions like lupus and rare genetic disorders like EPP or xeroderma pigmentosum, or a true sun allergy like solar urticaria. In children, photosensitivity can make play, education and daily life difficult since they may not be able to take part in regular outdoor activities. This may cause them to feel isolated, embarrassed and depressed. For some photosensitivity conditions, there are treatments available that can help reduce sensitivity to the sun. Sun protection is extremely important and can help prevent a reaction. Support groups may also be helpful to provide a safe and understanding environment where kids with photosensitivity disorders can come together and help each other. Ultimately, it is important to be supportive and understanding of anyone who has photosensitivity, and we hope you have learned about the many ways kids can be sensitive to the sun!
Glossary
Photosensitivity: ↑ Any condition that causes an unusual and dramatic skin response to light exposure.
Porphyrin: ↑ Natural body chemicals that help produce the red pigment in blood cells.
Erythropoietic Protoporphyria: ↑ A condition that causes painful photosensitivity due to a build-up of porphyrins in the skin.
Xeroderma Pigmentosum: ↑ A condition in which DNA damage is not repaired properly after sun exposure resulting in extreme photosensitivity.
Autoimmune Response: ↑ A condition in which the immune system mistakenly begins to attack healthy cells in the body.
Cutaneous Lupus Erythematosus: ↑ An autoimmune response in which the immune system in the skin is triggered by sunlight to cause a rash that sometimes resembles a wolf’s bite.
Solar Urticaria: ↑ Condition in which the skin forms very itchy circular bumps within 5–10 min of exposure to light; caused by IgE antibodies.
Corticosteroids: ↑ Medications that doctors prescribe to help control the immune system and relieve symptoms of many conditions, including lupus.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Chantorn, R., Lim, H. W., and Shwayder, T. A. 2012. Photosensitivity disorders in children. J. Am. Acad. Dermatol. (2012) 67:1093.e1–18. doi: 10.1016/j.jaad.2012.07.033
[2] ↑ Jensen, J. D., and Resnick, S. D. 1995. Porphyria in childhood. Semin. Dermatol. 14:33. doi: 10.1016/S1085-5629(05)80037-9
[3] ↑ AlKharafi, N. N., Alsaeid, K., AlSumait, A., Al-Sabah, H., Al-Ajmi, H., Rahim, J. A., et al. 2016. Cutaneous lupus erythematosus in children: experience from a tertiary care pediatric dermatology clinic. Pediatr. Dermatol. 33:200–8. doi: 10.1111/pde.12788
[4] ↑ Rizwan, M. 2008. Impact of Photosensitivity on the Lives of Children and Adults and Potential for Photoprotection. The University of Manchester.
[5] ↑ Okon, L. G., and Werth, V. P. 2013. Cutaneous lupus erythematosus: diagnosis and treatment. Best Pract. Res. Clin. Rheumatol. 27:391–404. doi: 10.1016/j.berh.2013.07.008