Abstract
Bacteria are tiny living things that like to attach to surfaces. Most bacteria are harmless, but if the harmful bacteria get into the human body where they do not belong, they can cause an infection. Infections make the human body very sick. Most infections with bacteria can be cured by antibiotics, but not infections caused by biofilms! Biofilms are communities of bacteria living together and covered in protective sticky goo, and most antibiotics do not work against them. Here, we explain how biofilms protect bacteria from antibiotics, and what we can do to fight with these long-term infections.
Bacteria are Everywhere!
We are surrounded by living things that are so tiny, we cannot see them with our eyes alone. These tiny living things are called bacteria, and they are on almost every surface you can think of, including your own body! There are bacteria on your keyboard, on your pillow, in soil, and in the water that comes out of the tap! In your intestines, there are billions of bacteria helping to break down the food you eat. In lakes, rivers, and oceans, bacteria use the power of sunlight to take up carbon dioxide and release oxygen for us to breathe. Most of the bacteria that live in, on, and around us are not dangerous. But, there are some bacteria that can make us very sick.
What is an Infection?
If you were able to look at the surface of your skin using a microscope, you would find a kind of bacteria called Staphylococci. These bacteria are round like a basketball (but four million times smaller!) and like to stick together in clumps (Figure 1). Staphylococci are on everyone’s skin (they are on you right now!), and many of them act like guards that help to keep away harmful bacteria that could make us sick. Sometimes, though, even these helpful Staphylococci bacteria can become a problem. When bacteria, including Staphylococci, enter the human body where they do not belong, they can create an infection, which means the bacteria are harmful to the body. Symptoms of infection are pain, redness, swelling, fever, aches, and in the worst case, death.
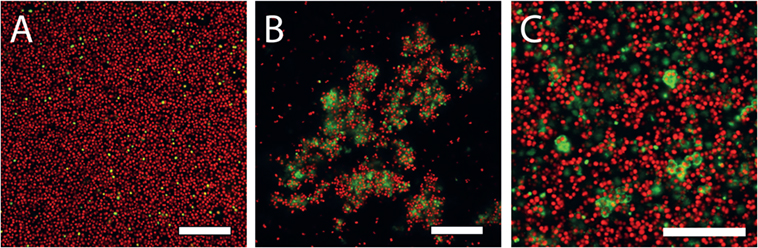
- Figure 1 - Images of Staphylococci bacteria in a biofilm seen under a microscope.
- Bacteria are shown in red, and one component of the extracellular polymeric substances that they make is shown in green (in this case, that substance is DNA). A. shows the biofilm bacteria that are closest to the surface. This is the lowest layer of biofilm cells. B. shows the top of a biofilm, where cells have become stuck together by extracellular polymeric substances. C. shows a close-up of cells deep within the biofilm, some of which appear to be producing extracellular polymeric substances. The length of white bars is 0.02 mm, which is 50 times smaller than the tip of a pencil!
So, how do bacteria get into the body? Bacteria can enter the body through minor damage to the skin like a scraped knee or a cut finger, or when a person is cut open during surgery in a hospital. Sometimes, people have new parts put into their bodies during surgery, like a new valve in the heart, or a metal screw to hold together broken bones. These new parts are called implanted medical devices. If bacteria get in along with these new parts, they can grow and reproduce inside the body. Staphylococci bacteria are the most common cause of infections on implanted medical devices, but other kinds of bacteria can be involved as well, such as Streptococcus, Enterococcus, or Escherichia coli. Infection can occur in the blood, bone, or soft tissue like the heart or skin [1]. Infections are very common on implanted medical devices because the implanted part becomes coated in fluids from our bodies, which the bacteria can eat, but the implanted medical device does not have its own immune system with which to protect itself. Often, our bodies can fight off an infection on their own, or a doctor might prescribe a special medicine against bacteria called an antibiotic, to help get rid of an infection. But sometimes, even antibiotics do not work! An infection might seem to be getting better, and then get worse again, and drag on for weeks or even months or years. This kind of long-term infection is called a chronic infection, and it can be caused by a bacterial biofilm.
What is a Biofilm?
Sometimes, bacteria swim or float freely in liquids – in the water in your tap, in juice left sitting on the counter, or, if a person has a blood infection, even in human blood. Swimming allows bacteria to move around to find food, or move away from things they do not like, such as bright sunlight, or cells from the human body that want to eat bacteria. But, most bacteria would rather sit still than swim around. Sitting still takes less energy, and bacteria that sit in the right spot can wait for food to come to them. Sitting still is the first step in making a bacterial biofilm (Figure 2). The first bacterium that sits still might be joined by others, or it might reproduce and make many more bacteria that are copies of itself. When more and more bacteria get together, they start to make sticky substances called extracellular polymeric substances, that they cover themselves with. This sticky community of bacteria is called a biofilm. The bacteria in a biofilm live happily eating whatever food comes along and can communicate with each other by releasing special molecules. Biofilms are very common [2]. The icky gunk in the bathroom drain is a biofilm. Scum covering a rock in a river is a biofilm. The mossy feeling your teeth get when you have not brushed them in a while? That is a biofilm on your teeth! Biofilms form on any surface that is wet and that has food for bacteria to eat.
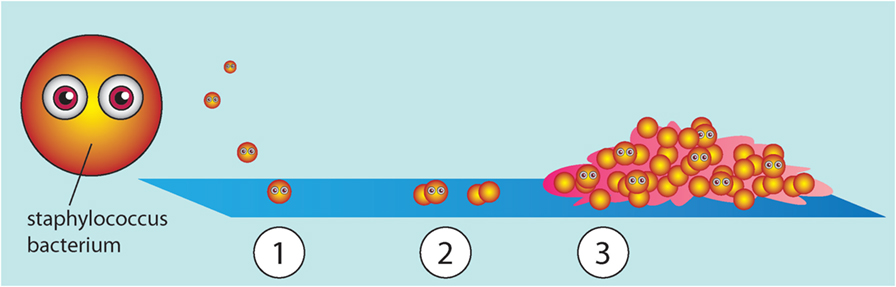
- Figure 2 - How a biofilm is formed.
- (1) A single bacterium attaches to a surface, such as your teeth or an implanted medical device. (2) This bacterium reproduces by making copies of itself. (3) The bacteria make extracellular polymeric substances to cover themselves with (shown in pink).
Biofilms Protect Bacteria from Attack
The human body makes special cells that find and destroy bacteria. These special cells, as well as antibiotics prescribed by a doctor to fight an infection, are very good at fighting bacteria that are swimming around inside your body. If these bacteria are exposed to an antibiotic for long enough, the bacteria will die, and you will be cured of the infection. On the other hand, bacteria living in a biofilm cannot be killed by antibiotics. Imagine a community of bacteria living on the outside of a metal screw implanted in a person’s leg bone. These bacteria are safe inside their protective biofilm. When the antibiotic comes along, it gets caught up in the sticky extracellular polymeric substances, and does not even reach the bacteria! Some bacteria on the outside of the biofilm may be killed by the antibiotic, but the bacteria on the inside of the biofilm are safe. The bacteria inside the biofilm are not all exactly the same, even if they are all copies of the first bacterium to settle down. When the bacteria get together, they communicate with each other about when they should start to attack the person’s body, and they take on different roles depending on where in the biofilm they are. Bacteria at the bottom of the biofilm may be in a dormant, “sleeping” state, which makes them resistant to some kinds of antibiotics. This means, even if antibiotic gets inside a biofilm, it does not kill all the bacteria. In fact, it would take 1000 times more antibiotic to kill all the bacteria in a biofilm community than is needed to kill bacteria while they are swimming on their own [3]. That would be so much antibiotic that it would kill the patient along with the bacterial infection! So, if antibiotics do not work, what can we do about chronic infections?
How Do We Treat a Chronic Infection?
The best way to get rid of a biofilm is to scrub it off. That is why we like to brush our teeth so much! Unfortunately, if the biofilm is on an implanted medical device, it is not easy to reach inside a person’s body to scrub away the biofilm. Often, treating a chronic infection requires more surgery, so the infected part can be removed and replaced with a new one. But having surgery always runs the risk of new infection, and surgery is not very nice for the person getting operated on. That is why scientists are looking for new ways to fight chronic infections. One way to fight a biofilm that cannot be removed from the body is to target the sticky goo holding the bacteria together. Some types of medicine destroy this goo and expose the bacteria to antibiotic treatment again [4]. For example, people with a disease called cystic fibrosis have chronic infections in their lungs. Part of the treatment for cystic fibrosis is to inhale a medicine that targets the sticky substances holding the biofilm together. This, coupled with antibiotics, can make cystic fibrosis patients breathe more easily, but it is not a permanent cure, because it does not completely remove the biofilm. Some scientists imagine that in the future we might have a medicine for chronic infections. These scientists are working on finding out what makes biofilm bacteria unique, so that this unique factor can be used as the target of a new anti-biofilm medicine.
Glossary
Bacteria: ↑ Tiny living things too small to be seen with the naked eye, sometimes called “germs.”
Staphylococci: ↑ A kind of bacteria that lives on our skin.
Infection: ↑ Bacteria that do not belong, living and growing inside the human body.
Implanted medical device: ↑ An artificial body part put in during surgery, to take over the role of a body part that does not work well anymore.
Antibiotic: ↑ Medicine against bacteria.
Chronic infection: ↑ An infection that lasts a long time and cannot be cured with antibiotics.
Biofilm: ↑ A community of bacterial cells protected by sticky goo.
Extracellular polymeric substances: ↑ Long molecules made of sugars, fats, and/or DNA, that biofilm bacteria cover themselves with.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ von Eiff, C., Jansen, B., Kohnen, W., and Becker, K. 2005. Infections associated with medical devices pathogenesis, management and prophylaxis. Drugs 65(2):179–214. doi:10.2165/00003495-200565020-00003
[2] ↑ Hall-Stoodley, L., Costerton, J. W., and Stoodley, P. 2004. Bacterial biofilms: from the natural environment to infectious diseases. Nat. Rev. Microbiol. 2(2):95–108. doi:10.1038/nrmicro821
[3] ↑ Stewart, P. S., and Costerton, J. W. 2001. Antibiotic resistance of bacteria in biofilms. Lancet 358(9276):135–8. doi:10.1016/S0140-6736(01)05321-1
[4] ↑ Okshevsky, M., Regina, V. R., and Meyer, R. L. 2015. Extracellular DNA as a target for biofilm control. Curr. Opin. Biotechnol. 33:73–80. doi:10.1016/j.copbio.2014.12.002