Abstract
Superbacteria are an important health issue. That is because they survive treatment with several bacteria-killing drugs, called antibiotics. When antibiotics do not kill bacteria, it is harder to treat infections, and even simple infections can become fatal. Although superbacteria are widely studied in hospitals, their presence in the environment remains underexplored. In this article, we will tell you about a type of bacteria called Shewanella, which we found in sea urchins. Sea urchins are often eaten in many countries. We found that some samples of Shewanella from sea urchins could survive antibiotics. The presence of antibiotic-resistant bacteria in seafood tells us that these superbacteria do not only exist in hospitals, and our finding highlights the need to address the serious health issue posed by superbacteria.
What Are Antibiotics?
In the past, sicknesses caused by bacteria used to kill many people. Even simple infections, like sore throats, could be fatal. That is because people did not know what caused infections, nor how to treat them. Without treatment, infections could quickly get worse and spread to other body parts, leading to serious health problems and even death. Eventually, scientists started to identify microorganisms, and only then were those tiny creatures discovered to be the cause of many infections.
In 1928, a scientist named Alexander Fleming was studying a type of bacteria that causes infections in humans. In one of his experiments, a fungus accidentally grew next to the bacteria. He observed that the bacteria could not grow in the area surrounding the fungus. In other words, he found out that a specific fungus inhibited bacterial growth. This was important because what Fleming saw led to the discovery of substances that we now call antibiotics. He later found out that some fungi are able to produce penicillin, the first antibiotic to be discovered. Penicillin made it possible to treat many infections and save millions of lives. Because of this huge discovery, Fleming received a Nobel Prize in 1945 [1].
What Does Antibiotic Resistance Mean?
We use antibiotics to treat infections caused by many bacteria. These medicines help to save millions of lives all around the world. Yet, antibiotics have often been used in an excessive manner, both in humans and other animals. Sometimes these drugs are used when they do not need to be. For example, since they only kill bacteria, antibiotics do not work on infections caused by other microorganisms, such as viruses. Overuse and misuse of antibiotics can trigger antibiotic resistance. But how?
When we use antibiotics to treat infections, we hope that the bacteria will die and that we will recover. But because we have been using the same antibiotics over and over again, sometimes unnecessarily, some bacteria have found ways of surviving in the presence of antibiotics, even when those drugs are used in large amounts! Scientists call bacteria that can survive the effects of antibiotics antibiotic-resistant bacteria [2]. Bacteria become antibiotic resistant because of changes that happen in their DNA. For example, these changes may prevent the antibiotic from getting inside the bacterial cells and destroying them. Other changes may allow the antibiotic inside the cells but pump it out before it causes the bacteria harm.
Antibiotic resistance is a helpful feature for bacteria, like a superpower! Bacteria have evolved in such a way that the parts of their DNA containing resistance instructions can be transferred from one bacterium to another. For example, some bacteria can store such instructions in small, circular pieces of DNA called plasmids. Bacteria can exchange plasmids with other bacteria. Not all bacteria have plasmids, but when they do, it sure helps them survive more easily!
How is this related to human health? The misuse of antibiotics has resulted in the survival of bacteria that are antibiotic resistant and therefore better at continuing to cause infections. Over the years, scientists have been noticing that some bacteria have become resistant to several antibiotics. In some countries, there are even bacteria that can survive all available antibiotics! Scientists call them superbacteria. Superbacteria are becoming more common each year, which is dangerous because the infections they cause cannot be treated by most antibiotics.
Could Water be a Source of Antibiotic Resistance?
Bacteria are living beings that can change to fit ever-changing environmental conditions. Superbacteria are common in hospitals, because that is where people go to have infections treated. Yet, bacteria can spread quickly and easily into other environments. For example, superbacteria from hospitals can travel through sewage pipes and end up in rivers, lakes, and oceans. But what happens when they reach these places?
Bacteria are natural residents of almost all places on Earth, including bodies of water, where there are billions of them. These bacteria are important to keep the environment in balance. For instance, some produce oxygen while others break down material from dead plants and animals. When antibiotic-resistant bacteria arrive in aquatic environments, they encounter other bacteria that do not carry the valuable genetic information necessary to survive antibiotics. When this happens, superbacteria may pass on their superpower, via plasmids. By doing that, the natural bacteria in the water may also become antibiotic resistant. But how can this affect us?
In aquatic environments, we can find bacteria free-living in the water or living in or on marine animals. Some aquatic bacteria may make us sick after we go swimming or eat seafood. These infections usually do not spread or cause long-term effects, so they are not generally a threat to healthy people. However, with the spread of superbacteria, infections may become much harder to treat with antibiotics, even in healthy patients! This means that common activities, such as eating seafood, could eventually lead to greater health risks (Figure 1) [3].
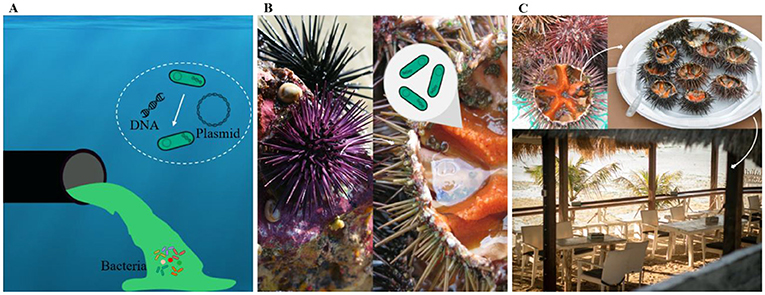
- Figure 1 - Antibiotic-resistant bacteria are found in the water and in seafood.
- (A) Bacteria can arrive in aquatic environments by traveling through sewage pipes. They can transfer the genetic information encoding their antibiotic-resistant “superpower” to other bacteria, using plasmids. (B) We studied a type of bacteria called Shewanella, isolated from the guts of sea urchins. (C) Some people eat sea urchins, so the presence of antibiotic-resistant Shewanella in these animals is a risk to human health.
What Kind of Superbacteria Are Found in Seafood?
To find out if seafood can carry superbacteria and how this can be a risk to human health, we studied a very peculiar animal: the sea urchin, collected in the waters of the Crozon peninsula in France. This area is famous for its beaches and fresh seafood, and it attracts many visitors, especially in the summer. Sea urchins are commonly eaten in Europe, and many people do not think that eating them could be a risk to their health. We studied a type of bacteria called Shewanella, which are commonly found in water or living in the guts of marine animals. Although generally harmless to humans, Shewanella can sometimes lead to infections of the intestines, blood, or existing wounds [4]. We asked if Shewanella could survive antibiotics and, if so, whether they carry plasmids that could be passed on to other bacteria (Figure 2).
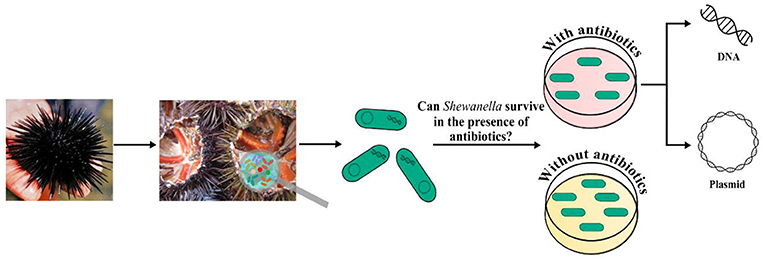
- Figure 2 - We tested Shewanella found in the guts of sea urchins to find out if the bacteria could survive in the presence of antibiotics.
- Then, we investigated antibiotic-resistant Shewanella by looking for the presence of DNA (including plasmids) containing information that could help them survive antibiotics.
Shewanella are not usually considered superbacteria, but, to our surprise, most of the Shewanella that we tested survived the antibiotics used to treat infections, meaning they were resistant (superpowers detected!) [5]. Curiously, four samples of bacteria survived even when we used three or more different antibiotics, meaning that some Shewanella are superbacteria, and any infection they cause would be challenging to treat. When we investigated Shewanella’s DNA, we found pieces of information that help bacteria survive antibiotics. We also noticed that many bacteria were carrying plasmids. Some could carry up to eight plasmids in just one tiny bacterial cell! That is a lot of plasmids, especially when we know that some bacteria do not have any. The presence of plasmids means that super-Shewanella can pass their resistance superpowers to other bacteria.
What Can We Do?
In summary, antibiotic resistance is a threat to human health, and aquatic bacteria can help to spread it. Although most Shewanella are harmless, our experiments showed that some can survive antibiotics and even spread antibiotic resistance. Most people do not realize that seafood can be a source of superbacteria, or that if someone eats sea urchins containing Shewanella, they might also be consuming antibiotic-resistant bacteria. This might also be true for other microbes and other kinds of seafood. These superbacteria can cause infections that are extremely difficult to treat, because many drugs will no longer be useful to fight the infections. Superbacteria are especially dangerous for people whose bodies already have trouble fighting off infections, like the elderly and people with certain chronic diseases like diabetes and asthma.
So, what can we do to tackle this problem? It is becoming more difficult to find new antibiotics, so instead we must do our best to slow down the spread of superbacteria. One of the most important ways to do this is to use antibiotics properly—only when it is necessary and when prescribed by a doctor. Good hygiene habits and basic sanitation also prevent superbacteria from reaching aquatic environments and causing infections. Together, these actions can help us control the spread of superbacteria in humans, animals, and the environment.
Funding
This work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, 306395/2020-7), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, 88887.613830/2021-00, Financial Code 001), and Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (E-26/200.948/2021, E-26/211.284/2021; E-26/201.191/2020).
Glossary
Infections: ↑ Invasion of the body by microorganisms, such as bacteria, that can escape the body’s defense system and cause disease.
Antibiotics: ↑ Medications used to treat bacterial infections by killing or preventing the growth of bacteria.
Antibiotic-Resistant Bacteria: ↑ Bacteria that can survive in the presence of certain antibiotics.
Plasmids: ↑ Circular DNA molecules that can be found in some bacteria and be transferred between bacteria. Sometimes plasmids carry genetic information about ways to survive in the presence of antibiotics.
Superbacteria: ↑ Bacteria that can survive in the presence of several antibiotics, causing infections that are extremely difficult to treat.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Original Source Article
↑da Costa, W. F., Giambiagi-de Marval, M., and Laport, M. S. 2020. Shewanella harboring antimicrobial and copper resistance genes in sea urchins (Paracentrotus lividus) from the Crozon peninsula (Brittany, France). Infect. Genet. Evol. 85:104437. doi: 10.1016/j.meegid.2020.104437
References
[1] ↑ Aminov, R. I. 2010. A brief history of the antibiotic era: lessons learned and challenges for the future. Front. Microbiol. 1:134. doi: 10.3389/Fmicb.2010.00134
[2] ↑ Nadeem, S. F., Gohar, U. F., Tahir, S. F., Mukhtar, H., Pornpukdeewattana, S., Nukthamna, P., et al. 2020. Antimicrobial resistance: more than 70 years of war between humans and bacteria. Crit. Rev. Microbiol. 46:578–99. doi: 10.1080/1040841X.2020.1813687
[3] ↑ Elbashir, S., Parveen, S., Schwarz, J., Rippen, T., Jahncke, M., and DePaola, A. 2018. Seafood pathogens and information on antimicrobial resistance: a review. Food Microbiol. 70:85–93. doi: 10.1016/j.fm.2017.09.011
[4] ↑ Yousfi, K., Bekal, S., Usongo, V., and Touati, A. 2017. Current trends of human infections and antibiotic resistance of the genus Shewanella. Eur. J. Clin. Microbiol. Infect. Dis. 36:1353–62. doi: 10.1007/S10096-017-2962-3
[5] ↑ da Costa, W. F., Giambiagi-De Marval, M., and Laport, M. S. 2020. Shewanella harboring antimicrobial and copper resistance genes in sea urchins (Paracentrotus Lividus) from the crozon peninsula (Brittany, France). Infect. Genet. Evol. 85:104437. doi: 10.1016/j.Meegid.2020.104437
