Abstract
Warts are little lumps growing in the skin. You might have had a wart or know them from children’s books, typically growing on witches’ noses. Warts are quite common in children. Did you ever wonder where they come from? You might be surprised to learn that warts are caused by a virus. Viruses are germs that need cells to multiply themselves. Cells are the building blocks of all living things. The virus that causes warts, called human papillomavirus, infects skin cells and transforms them into microscopic virus-making factories. The virus has special tools to cause skin cells to grow faster and live longer. This leads to the overgrowth of skin cells, which forms the wart. Viruses spread from person to person, making them contagious, and so warts are contagious too. Good hygiene and covering the wart are strategies to avoid spreading warts to other body sites and other people.
Your Skin Renews Itself Every Month!
To understand how warts grow, we first need to understand how healthy skin grows. Your whole body is built of cells, which are the basic building blocks of every living organism and are microscopic in size. Your cells are made by following instructions written in your genes. Your genes are essentially like a book of Lego instructions to build all kinds of different cells in your body. However, genes are not an actual book of pages, but are complex chemical instructions that control the cells that you are made of. All the genes together are called the genome.
The complex human body has many different types of cells, each performing a different task. Many cells of the same type form an organ, such as your brain, your heart, or your skin. Your skin is the largest organ of your body, made up of more than 1 trillion skin cells, and it forms a watertight barrier to keep things out of your body and protect your organs inside. Healthy skin is very neatly organized, consisting of different layers of cells and a very accurate structure, resulting in a smooth, even surface (Figure 1A). This structure is created by the genes in your skin cells. Your skin consists of two main parts, the outer layer (called the epidermis) and the inner layer (called the dermis), which are connected by a membrane. Your normal skin cells are always dividing and producing new skin cells from cells called basal cells, which are located on top of the membrane between the dermis and epidermis. From there, the new skin cells travel outwards, and eventually die and shed to the environment. Did you know that your healthy skin regenerates itself every month?
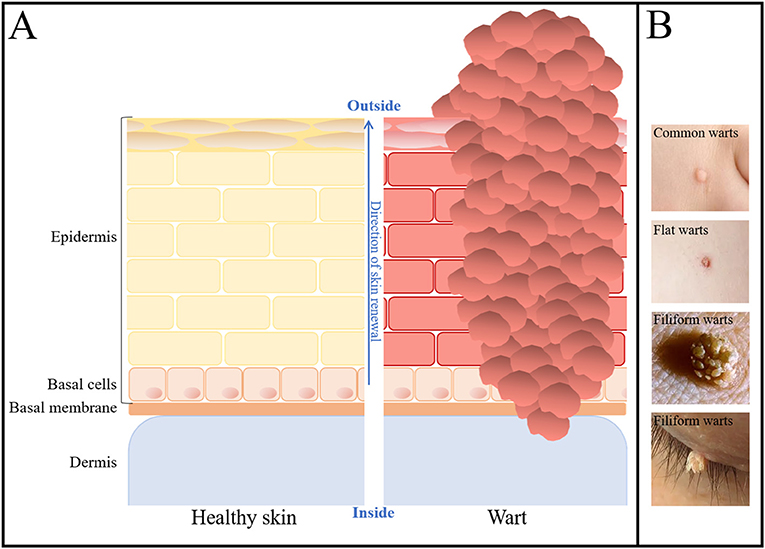
- Figure 1 - Microscopic scheme of healthy skin and warts.
- (A) The structures of healthy skin (left) and of a wart (right). The layers of healthy skin cells are neatly organized. The basal cells continuously renew the skin by dividing and moving from inside to outside. At the outer layer, skin cells die and are shed. In a wart, the neat organization of skin cells is disturbed. Skin cells grow too much and pile up, creating a bulge on the outside that reaches down into the dermis. (B) Photographs of different kinds of warts that might be found on a child’s hand, face, or eye (Source: Blog Articles, Penguin Pediatrics PLLC, WebMD, and MomJunction).
Skin Renewal Goes Wrong in Warts
Warts are small hard lumps growing in your skin. Warts are common, especially in primary school children [1]. Chances are, at some point in your young life, you might have had a wart or know someone who has. Warts most often appear on hands and feet but can really appear anywhere on your body. The medical word for wart is papilloma. Warts appear in different shapes (Figure 1B). Most of them look like hard, rough, elevated lumps, others can look like tiny cauliflowers, and still others can form long brush-like growths [2].
In warts, the neat organization of skin cells is disturbed, and the skin cells grow too much. By “grow,” we do not mean grow in size, but grow in numbers. In warts, skin cells also live longer than normal, and together these effects cause skin cells to pile up, creating the wart (Figure 1A). The very top of the wart is often covered by a callus, which consists of dead, dried-out skin cells that have not shed.
Warts tend to stay in your skin for a long time, often months and sometimes years, before they suddenly disappear. Sometimes you might need to seek medical treatment for a wart, especially if it is in a place on your body where it bothers you, such as the bottom of your foot or between your fingers where you hold a pen. There are medicines available to put on the skin, or sometimes doctors can freeze warts (known as cryotherapy), which kills the wart cells and allows healthy skin to regrow.
Warts are Caused by Papilloma Viruses
Possibly, after you had your first wart, you soon developed other warts, either close to the first wart or at a different place on your body. This is explained by the fact that warts are caused by a virus, and because the virus can spread on your body or be transmitted between people, warts are contagious.
Viruses are extremely tiny germs that only exist to make more viruses. They are lifeless on their own and can only multiply by infecting your cells, where sometimes they cause diseases, such as the common cold, influenza, or Covid-19. There are many different families of viruses, and the virus family that causes warts is called human papillomavirus (HPV). Scientists have identified more than 390 different types of HPV [3] and 10 of these can cause warts [4].
All HPV family members look very similar. The HPV virus is tiny—just 55 nm. One nanometer is one-millionth of 1 mm, which makes the HPV virus much too small to see with your naked eyes. Scientists use a special microscope called a transmission electron microscope (Figure 2A) to see the HPV virus and take photographs of it (Figure 2B, left). HPVs are made of a shell called the capsid, which wraps up and protects the genome. The HPV capsid consists of 72 blocks, each of which is made of 5 units of capsid proteins, called pentamers (Figure 2B, right top). The HPV genome (Figure 2B, right bottom) codes for everything that the virus needs to multiply itself.
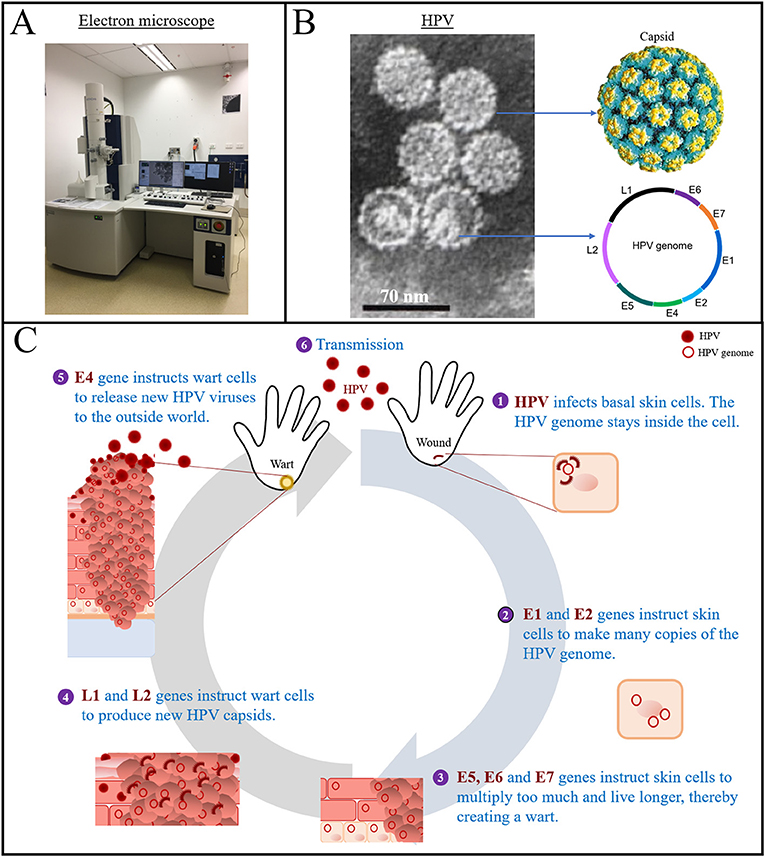
- Figure 2 - Structure and life cycle of the human papillomavirus (HPV).
- (A) A transmission electron microscope (Photo by Dr. Meihua Yu). (B) HPV as seen using an electron microscope (Source: Wiki, licensed under Attribution 3.0 Unported), and a drawing of the HPV capsid (Source: Micobewiki) and genome. The capsid is made of pentamers, in which 5 capsid units are combined. The HPV genome is a circular strand of DNA, which contains the early and late genes. (C) During the life cycle of HPV, each gene has a specific function. Together, the genes multiply the HPV genome, assemble new viruses, and help the new viruses to exit the cell.
In general, genes code for proteins, which are the molecules in all living things that do specific tasks. Proteins are essential for all life. Viruses cannot live on their own because they do not have their own protein-making factories. So, they hijack the cell’s protein-making factory to multiply themselves. To hijack the cell’s protein-making factory, viruses need to infect cells, meaning they need to get their genomes inside the cells. Viruses often prefer infecting a certain part of the body, and HPV likes to infect skin. HPV cannot infect the outer layer of the skin—it needs to get to the inner, basal cells (Figure 1A) through tiny cuts or wounds. As explained earlier, basal cells constantly restock your skin with fresh cells, so they are responsible for the ongoing renewal of your skin. The virus hijacks the multiplying machinery of the basal cells to multiply itself!
Turning Skin Cells Into Virus-Making Factories
When HPV infects the basal cells of the skin (Figure 2C), it takes apart its capsid and the virus genome goes inside the cell [5]. The HPV genome contains instructions for making new viruses. It also contains instructions to control the cells. These control instructions tell the skin cells to multiply more and live longer, allowing HPV to produce more viruses inside the cells. The HPV genome is in the form of a ring and contains eight genes, which become eight proteins (Figure 2B). The E genes (E stands for early) are translated into proteins early after infection, in the lower layers of the skin. Six E genes (E1, E2, E4, E5, E6, and E7) are needed to turn skin cells into virus-making factories. The E1 and E2 genes instruct the cell to make many new viral genomes. The E5, E6, and E7 genes instruct skin cells to multiply and live longer, and this way transform the skin into warts! The L genes L1 and L2 (L stands for late) encode the proteins of the HPV capsid. These genes are activated late in the viral life cycle, and in the upper layers of the skin. Once the wart cells contain viral protein shells and genomes, they can assemble new viruses, and the E4 gene activates the release of new viruses to the outside world. Once the skin cells die and break, they release thousands of new HPV viruses, which are now ready to infect skin of other parts of the body or travel to another person. When the new virus then finds an entry into the skin through a small wound or scratch, it will again infect basal cells and the viral life cycle starts anew.
Transmission and Treatment
The often-rough surface of the wart is made of callus, which is essentially composed of dead, dried-out skin cells. As the wart keeps growing, the number of dead cells on the surface keeps piling up, and every time a skin cell dies and breaks, it releases thousands of HPV viruses. If you have a wart on your hand, it is easy to transmit the virus to anything you touch, including other parts of your body, or other people, like your family or your friends. HPV can also be transmitted through surfaces, for example through toys or the floor at the swimming pool where many people walk barefoot. To prevent infection, it is very important to practice good hygiene the same way we do to avoid catching other germs, for example by regularly washing hands and cleaning surfaces and shared toys. If you have a wart, it is important to remain aware that you can spread HPV, so you should act responsibly to avoid this. A good strategy is to cover your wart with a band aid. If you have a wart that bothers you, you should see your doctor for treatment options.
Conclusion
Warts are caused by a virus called HPV. HPV hijacks skin cells to produce more HPVs, and manipulates skin cells to grow more than normal. This results in disruption of the neat skin cell organization and the growth of warts. HPV and therewith warts can be transmitted to other people.
Glossary
Gene: ↑ A segment of the genome that codes for a specific protein.
Genome: ↑ All the chemical instructions of an organism.
Epidermis: ↑ The outer layers of the skin.
Dermis: ↑ The inner layers of the skin.
Basal Cell: ↑ A specialized type of skin cell responsible for continuous renewal of the skin.
Papilloma: ↑ The medical term for a wart. The word is a hybrid of papilla (nipple) and -oma (growth).
Human Papillomavirus (HPV): ↑ A family of viruses that can cause warts.
Capsid: ↑ The outer shell of a virus, which is made of proteins.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ van Haalen, F. M., Bruggink, S. C., Gussekloo, J., Assendelft, W. J. J., and Eekhof, J. A. H. 2009. Warts in primary schoolchildren: prevalence and relation with environmental factors. Br. J. Dermatol. 161:148–52. doi: 10.1111/j.1365-2133.2009.09160.x
[2] ↑ Hogendoorn, G. K., Bruggink, S. C., Hermans, K. E., Kouwenhoven, S. T. P., Quint, K. D., Wolterbeek, R., et al. 2018. Developing and validating the Cutaneous WARTS (CWARTS) diagnostic tool: a novel clinical assessment and classification system for cutaneous warts. Br. J. Dermatol. 178:527–34. doi: 10.1111/bjd.15999
[3] ↑ Bzhalava, D., Muhr, L. S. A., Lagheden, C., Ekstrom, J., Forslund, O., Dillner, J., et al. 2014. Deep sequencing extends the diversity of human papillomaviruses in human skin. Sci. Rep. 4:5807. doi: 10.1038/srep05807
[4] ↑ Bruggink, S. C., de Koning, M. N. C., Gussekloo, J., Egberts, P. F., ter Schegget, J., Feltkamp, M. C. W., et al. 2012. Cutaneous wart-associated HPV types: prevalence and relation with patient characteristics. J. Clin. Virol. 55:250–5. doi: 10.1016/j.jcv.2012.07.014
[5] ↑ Hebner, C. M., and Laimins, L. A. 2006. Human papillomaviruses: basic mechanisms of pathogenesis and oncogenicity. Rev. Med. Virol. 16:83–97. doi: 10.1002/rmv.488
