Abstract
When we think of microbes that can make us sick, it is usually bacteria that cross our minds first. We tend to forget about another major microbial type that can also cause severe diseases: the fungi. Yeasts and molds make up the majority of microscopic fungi and both types can cause various infections in humans, from mild skin rashes to deadly blood infections. These fungi have found several ways to cause us harm, such as using the body’s nutrients, escaping the surveillance of the immune system, or hijacking and destroying our cells. On cellular level, we have a lot in common with fungi. These common features between human cells and fungal cells makes the development of antibiotics and vaccines to treat fungal infections very difficult. In this article, we will describe some fungal infections and explain current options for their treatment.
Fungi Among Us: Friends and Foes
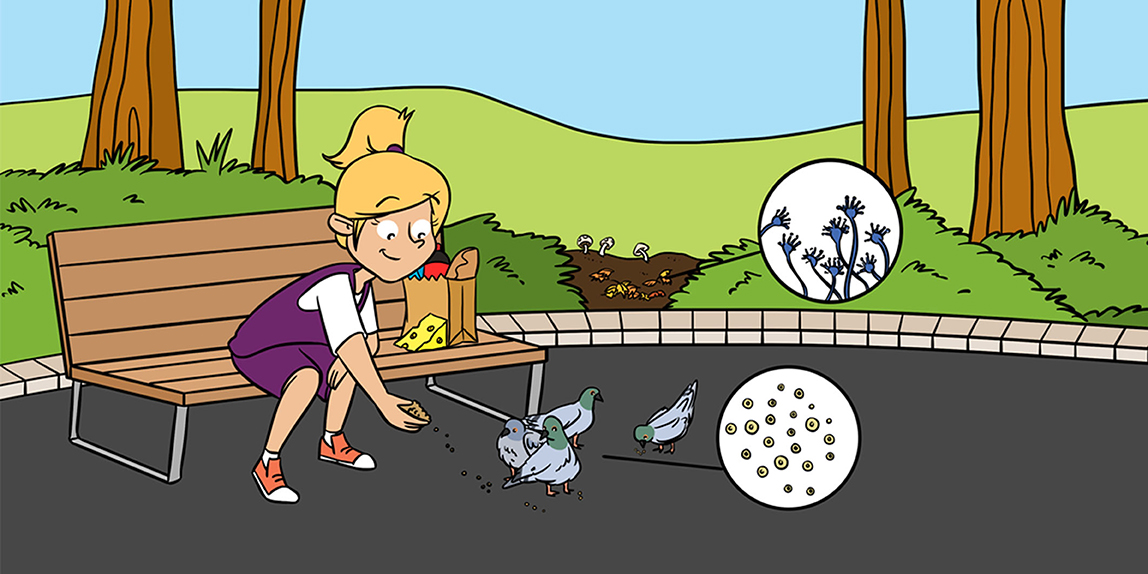
In the tree of life, fungi are classified in their own kingdom. They are different from bacteria, plants, or animals. “Fungus” in Latin means mushroom. That is why we tend to think only about mushrooms as the fungi among us. However, the fungal kingdom is very diverse and there are thousands of fungi that we find only when we dive into the microbial world, where organisms are so tiny that they can only be seen under a microscope. The microscopic fungi come in many different shapes and forms (Figure 1), and can be found everywhere in nature, like in the soil or attached to living creatures. They play many important roles in our lives, such as decomposing organic matter in the compost pile or bringing nutrients to plants. For thousands of years, we have been using fungi to produce foods and beverages like bread, cheese, soy sauce, and beer. Fungi are also used to make the antibiotic penicillin, which kills bacteria, and to produce citric acid, which is what gives juices and sodas a sour note.
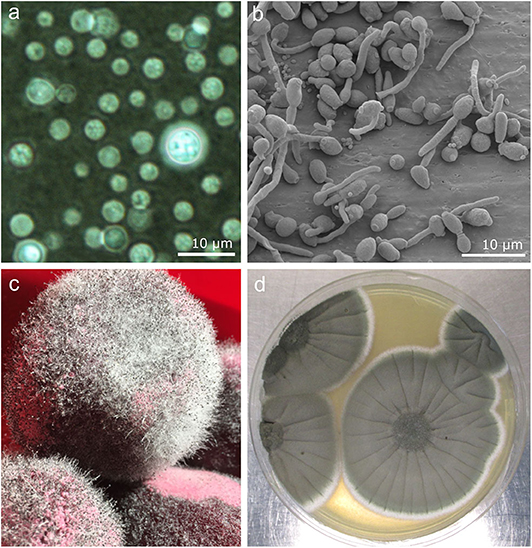
- Figure 1 - Images of fungi that infect humans.
- (a) Microscopic image of Cryptococcus neoformans stained with ink. (b) Seen through a scanning electron microscope, Candida albicans starts to form mycelium. (c) Rhizopus species growing on cooked beetroot. The fur-like substance is the mycelium and the tiny black dots on top contain the spores. (d) Aspergillus fumigatus, isolated from soil, as seen with the naked eye as it grows in the lab.
Some fungi even live in our bodies. Together with more than 10,000 other microbial species found in our guts and on our skin, fungi make up our microbiota. The microbiota is composed of millions of harmless microorganisms that inhabit the human body. Usually we live happily together. We can come into contact with other fungi from the environment by breathing them in, for example. But we almost never notice them, as the mucus that covers our airways usually clears them out. However, sometimes this is not the case: both types of fungi—the ones living in harmony inside us and the kinds in the environment—can cause infections.
Interestingly, only a few hundred fungal species of the almost 5 million that inhabit the Earth can cause infections in humans [1]. In contrast, about 50,000 species of fungi infect insects. Why is the number for humans so low? First, the relatively high and always stable body temperature of ~37°C keeps them away. Most of the fungi favor much lower temperatures [2]. Next, most fungi are successfully fought off by the human immune system, which does a very good job of eliminating fungi when they infect healthy people.
Fungi can cause a range of infections in humans, from unnoticeable to deadly. We barely notice the fungus that can cause dandruff, for example. This condition is annoying and embarrassing, but rarely causes us harm. Other fungi can cause life-threatening infections that shut down the entire body. Typically, people with disturbed or defective immune systems, such as patients being treated for cancer, organ transplant recipients, or the elderly, suffer the most. Such infections are very difficult to treat.
Which Fungi Are the Most Dangerous and How Do They Make Us Sick?
Cryptococcus
Cryptococcus species, and particularly Cryptococcus neoformans, are like kryptonite for humans. Normally, this fungus lives on plants or in animals worldwide. Pigeons, for example, have a lot of Cryptococcus neoformans in their droppings, and although this does not bother them, it can bother us. The dust from pigeon droppings is spread in the air that we breathe. In healthy people, if Cryptococcus enters the lungs it is defeated by the immune system, but in people with immune defects it can survive, grow, and reach other parts of the body, such as the brain. If left untreated, it can cause death [3].
Candida
Candida species, particularly one called Candida albicans, are the most common fungi that cause diseases in humans. Candida albicans is normally part of our microbiota, but can, if given the chance, turn against us. C. albicans can cause infections of the skin or the mouth and can even enter the bloodstream and cause a life-threatening blood infection called sepsis. Candida cells can transform from a rounded shape into a long filament called a mycelium. The mycelium can easily grow deep into the tissue or form complex structures that can resist the immune system’s attack or drug treatment. Scientists do a lot of research to figure out what allows Candida to switch from one form to the other, because the switch could be a potential target for new drugs [3].
Molds
Molds usually live in soil and on dead, decaying matter. They produce mycelium with thousands of tiny spores on top. These spores function as seeds as they can be used for reproduction or to withstand harsh conditions. The spores are easily spread by air and enter our lung when we breathe. As mentioned above, this is typically problematic only for people with weak immune systems. The most important molds that cause disease are Aspergillus species, mostly Aspergillus fumigatus, and the Mucorales species Rhizopus, Lichtheimia, and Mucor. In the lungs of vulnerable individuals, Aspergillus fumigatus spores can grow into a mature fungus, enter the bloodstream, and spread around the body to cause a severe, and often fatal, infection called invasive aspergillosis. Mucorales species cause a similar course of infection: once in the body they can breach the immune barriers, spread, and become potentially deadly. Mucorales are fast-growing fungi that resist many drugs, so immediate diagnosis and treatment are necessary [3, 4].
How Do Antifungal Drugs Fight the Fungi?
On the cellular level, we have much in common with fungi. So, it is likely that a substance directed against fungi could also harm us. Therefore, it is quite difficult to design drugs that kill only the fungi. Any potential antifungal drugs have to pass toxicity tests on human cells and other rigorous tests to make sure they are safe for human use.
So far, only three fungus-specific vulnerable spots are targeted by drugs (Figure 2). First is the cell membrane. The cell membrane of fungal cells has a certain type fat called ergosterol, which is only produced by fungal cells. Without ergosterol the fungus cannot survive. Two antifungal drugs successfully target this molecule: Amphotericin B targets ergosterol itself, while drugs called azoles disturb its production. Amphotericin B is used only as a last-resort drug, because it is somewhat toxic to human cells.
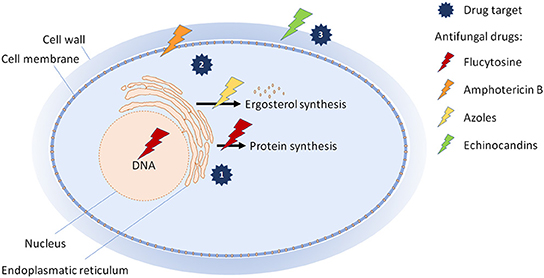
- Figure 2 - How common antifungal drugs work.
- Currently, antifungal drugs are directed against three different targets in the fungal cell: (1) The drug flucytosine disturbs the production of DNA and proteins in the fungal cell; (2) amphotericin B and azoles target the cell membrane by interfering with a fat called ergosterol; and (3) echinocandins block the building of the sugar molecule glucan, which is an essential brick of the fungal cell wall.
Another way to eradicate fungi is with a substance called flucytosine, which targets essential for fungal survival processes, such as production of DNA and building of proteins. But this medicine also leaks into human cells and has many severe side effects. So, this drug is used mainly in combination with Amphotericin B and only for very serious cases.
The third drug target is the fungal cell wall. In contrast to human cells, fungal cells are surrounded by a thick wall made from a substance called chitin, as well as sugars and proteins. A class of drugs called echinocandins interferes with the building of a sugar molecule called glucan, an essential brick of the cell wall. Echinocandins are very safe for humans, but they work only when injected into the bloodstream, which is not very practical.
So, with only three types of drugs, each with some disadvantages, doctors are facing a problem choosing the most effective and safe treatment for fungal infections. Therefore, there is an urgent need to find new targets and treatment strategies for these infections [5].
New Antifungal Therapies on the Horizon
One way to fight drug-resistant fungi is to combine several medicines. In this way therapy could be much more powerful. This has already worked to fight other deadly diseases. Combining two antifungal drugs has also proven successful for Cryptococcus infections [5]. Other attempts aim at inhibiting the infectious properties of these fungi. But what if we could prevent humans from getting fungal infections in the first place? We could protect ourselves by keeping our immune systems healthy, or by vaccination. While there are numerous vaccines against viruses and bacteria, no vaccine can protect us from fungal diseases. Fortunately, many attempts to design vaccines against fungal infections are in progress.
Conclusion
Even though our body temperature and powerful immune system keep infections away, fungi can still cause us harm (Figure 3). Patients with weak immune systems are particularly prone to invasive fungal infections. The number of patients at risk is continuously increasing. At the same time, treatment of these infections is complicated because of the limited number of drugs and the increase in drug-resistant fungal species. Doctors urgently need more safe and effective medicines against fungal infections. Fungi are not only dangerous for humans: plants, insects, and cold-blooded animals like fish and amphibians get infected too. For example, the fungus Batrachochytrium dendrobatidis has already caused the extinction of over 100 frog species worldwide [1]. Therefore, researchers must keep working to find out more about how fungi cause infections and how to fight these potentially dangerous organisms.
- Figure 3 - The immune system fights fungal invaders.
- FunGal (a.k.a. fungus) lives in the environment or associated with the human body, but sometimes can invade the human to cause infection. The powerful Immuna (a.k.a. human immune system) attacks and defeats FunGal. However, in some people, Immuna is weakened, so FunGal can cause infection and antifungal drugs are urgently needed to stop FunGal’s attack.
Glossary
Microbiota: ↑ All the millions of harmless microorganisms that inhabit the human body.
Sepsis: ↑ The most severe form of an infection, which can lead to organ failure and often death.
Mycelium: ↑ Thread-shaped cells of a fungus.
Spores: ↑ Round-shaped reproduction units of a fungus, similar to seeds, which can grow into a mature mycelium.
Ergosterol: ↑ A type of fat found in cell membranes of fungi. Ergosterol serves similar functions as cholesterol serves in human cells.
Chitin: ↑ A sugar that is the major part of the fungal cell wall. Chitin also forms the exoskeleton of insects and other arthropods.
Glucan: ↑ A complex sugar molecule that composes the fungal cell wall, a structural layer that surrounds the cell and provides support and protection.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank our colleagues Grit Walter from the National Reference Center for Invasive Fungal Infections and Amelia Barber from Leibniz Institute for Natural Product Research and Infection Biology–Hans Knöll Institute for providing us images of Cryptococcus neoformans and Aspergillus fumigatus, respectively. Special thanks for the young in house reviewer Boris B. Tsenov for his insightful comments and help in figure design. This work was supported by the Federal Ministry of Education and Research (BMBF 03Z22JN11 and 01EO1502) to SV.
References
[1] ↑ Köhler, J. R., Hube, B., Puccia, R., Casadevall, A., and Perfect, J. R. 2017. Fungi that infect humans. Microbiol. Spectr. 5:FUNK-0014-2016. doi: 10.1128/microbiolspec.FUNK-0014-2016
[2] ↑ Robert, V. A., and Casadevall, A. 2009. Vertebrate endothermy restricts most fungi as potential pathogens. J. Infect. Dis. 200:1623–6. doi: 10.1086/644642
[3] ↑ Brown, G. D., Denning, D. W., Gow, N. A., Levitz, S. M., Netea, M. G., and White, T. C. 2012. Hidden killers: human fungal infections. Sci. Transl. Med. 4:165rv13. doi: 10.1126/scitranslmed.3004404
[4] ↑ Prakash, H., and Chakrabarti, A. 2019. Global epidemiology of mucormycosis. J. Fungi (Basel). 5:26: doi: 10.3390/jof5010026
[5] ↑ Robbins, N., Wright, G. D., and Cowen, L. E. 2016. Antifungal drugs: the current armamentarium and development of new agents. Microbiol. Spectr. 4:FUNK-0002-2016. doi: 10.1128/microbiolspec.FUNK-0002-2016