Abstract
We all experience pain at one time or another. Pain is an essential “alarm bell” that tells us that something is wrong, and a “teacher” that reminds us not to do that same thing again. Usually, pain is felt when a stimulus, such as a pinch or an injury, causes electrical pulses to run along one of the cables of nerve fibers in our body and into the brain where they generate an unpleasant sensory and emotional experience. Sometimes pain occurs without any actual stimulus, such as when nerve fibers have been damaged. An example is the phantom pain that amputees sometimes feel in their missing limb. Certain drugs can stop pain by blocking the electrical pulses before they reach the brain. Other drugs stop pain in a different way, by preventing the brain from reading the pain message carried by the electrical pulses. This article explains what happens in the body when we are hurt, how the brain causes this to be felt as pain and how certain drugs can stop pain.
Pain Hurts!
Have you ever fallen off your bicycle and scraped your knee? It was probably pretty painful at first, and maybe you even cried. But, in a day or two, your knee probably stopped hurting. You may also have banged your elbow (“funny bone”) on the edge of a table. If you did, you probably felt a very different kind of pain, strong, sharp, and a little like an electric shock, but with no skin damage or bleeding. This second kind of pain probably disappeared in just a few minutes. How does a scrape on the knee or a bang on the elbow cause the feeling of pain to start, and what eventually stops the pain? Why do these different types of pain feel so different? Where was the pain actually felt, in your knee or in your brain? And why does pain sometimes make us cry?
Your Knees and Elbows Are Connected to Your Brain by Nerves
When you fell off your bike and hurt your knee, a signal was generated in the knee that traveled to your brain (Figure 1). Such signals are carried in the form of electrical pulses that run along nerves inside your body. Nerves are long, white bundles, like internet cables, that contain large numbers of individual nerve fibers. Each nerve fiber is an extension of an individual nerve cell (or neuron). The pain message begins in the injured part of the knee where the skin was scraped. Electrical pulses are generated at specialized branches at the end of each nerve fiber and from there they travel up along the nerve toward the brain. Endings of some nerve fibers generate electrical pulses when the skin is touched lightly. Others make pulses when they are exposed to heat, cold, or strong forces like when your knee scraped the ground. When the sensory signals generated in your knee reach your brain a sensation of touch, heat, cold, or pain is created. Which sensation you feel depends on which types of nerve fibers generated the electrical pulses and where exactly the signals ended up in the brain. When you fell off your bike and scraped your knee many nerve fibers that respond to strong forces were activated and they arrived in a part of your brain that is specialized for pain sensation. That’s why the resulting sensory signal caused scraping pain to be felt.
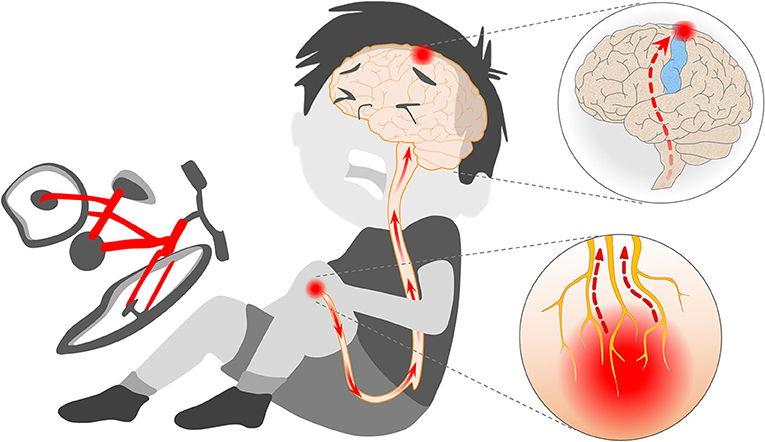
- Figure 1 - When you fall off your bike and scrape your knee, strong forces and torn skin cause the endings of nerve fibers in the skin (yellow branches in the red cloud) to generate a flow of electrical pulses (red arrows).
- The sensory signal carried by these pulses travels along the nerves of your leg, up your spinal cord and into the parts of the brain responsible for creation of the experiences of touch, temperature and (perhaps) pain that you feel in your body (blue), and specifically in your knee (red). This signal also activates additional brain areas that cause suffering, sadness and tears.
When you banged your elbow, different nerve fibers were activated. What happened is that a whole nerve was pinched between the table edge and the bone of your elbow. This damaged some of the nerve fibers within the nerve and activated them briefly. Electrical pulses were created all at once in many different types of sensory nerve fibers, not just the kind sensitive to skin scraping. The only other time this happens is when you get an electric shock. That is why the sensation you felt upon banging your elbow probably felt like an electric shock.
Pain Is in the Brain
The brain is the body’s “command central.” It is where all sensations are experienced, not in the knee and not in the elbow. One way we know this is from amputees, people who have suffered the loss of a leg or an arm because of an injury or a disease. Amputees almost always continue to feel their missing limb as if the limb were still there. This phantom limb sensation may be tingling, electric shock-like, burning, or stabbing. Where do the electrical pulses come from when the limb itself is actually missing? Some scientists think they originate from within the brain, like the impulses that cause dreams. We believe they originate in injured nerves in the remaining parts of the limb (Figure 2). This is a little like your banged elbow except that the injury is much more severe, and the electrical pulses and the pain, often last for the remainder of the amputee’s life [1].
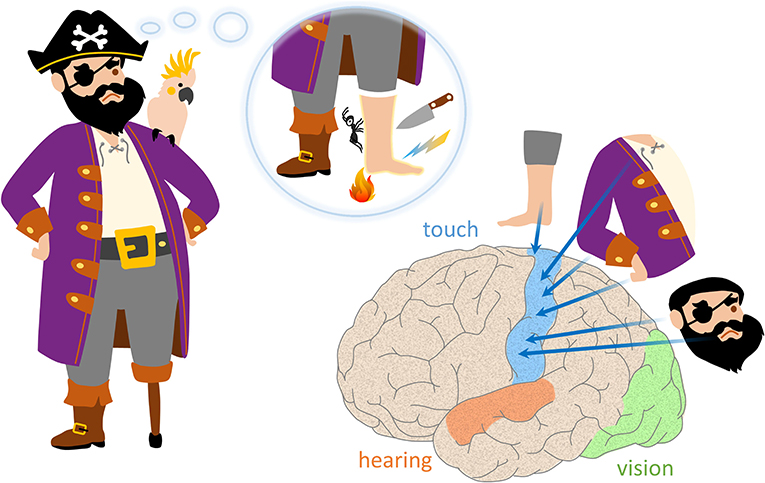
- Figure 2 - People who are missing a leg or an arm because of injury or disease almost always feel the limb as if it were still present.
- The so-called “phantom limb” may feel like ants are crawling on it, or the sensations might resemble electrical shocks, burning, or stabbing. What causes these abnormal sensations? Scientists believe that these sensations are felt because nerve cells in the touch, temperature and pain areas of the brain (blue), particularly the areas related to the missing limb, the foot in this drawing, become active. The brain activity is probably driven by electrical pulses that come from the remainder of the injured nerve still present in the stump of the leg still attached to the body. Other sensory experiences are created in other parts of the brain (vision–green, hearing–orange).
There are also many other ways we know that sensation happens in the brain. For example, in some surgical operations the patient’s skull is opened, exposing the brain. When the surgeon applies electric pulses directly to the brain the patient says he feels things, depending on where the brain was stimulated. When the back of the brain is stimulated, for example, the patient sees lights even when his eyes are closed (Figure 2). Stimulation of the side of the brain causes the patient to hear sounds, sometimes recognizable tunes! And stimulation on the top of the brain generates tingling in the foot, arm, or face, a little like the phantom limb sensation. We do not know yet for sure where the sensation of pain is created.
Amazingly, electrical activity in other areas of the brain creates emotions like anger, sadness, and love [2]. The reason you might have cried when you scraped your knee is that, in addition to activating pain areas in the brain, the electrical pulses that came from your knee also activated the parts of your brain that generate emotions, creating a feeling of unhappiness and releasing tears from your eyes (Figure 3). The brain is also where motivations like hunger, thirst, and wanting things happen. And, most importantly, the brain is what gives us the feeling that we exist, that we are conscious and not in a deep dreamless sleep.
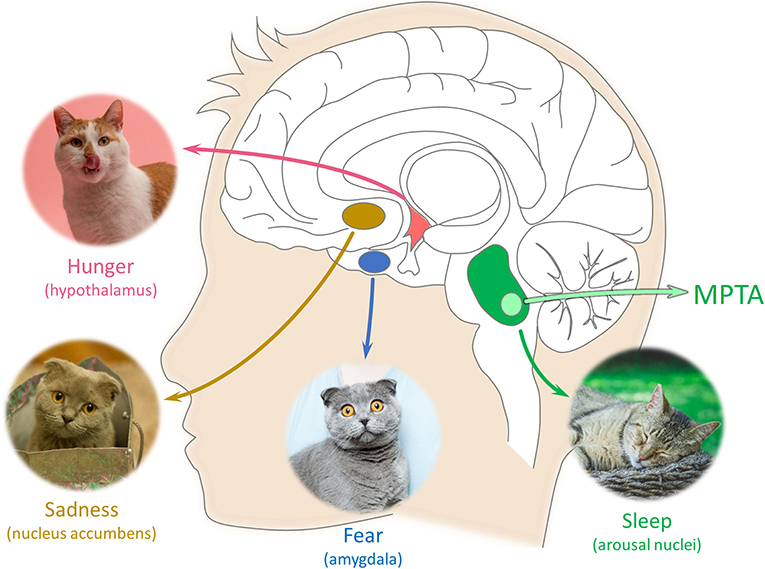
- Figure 3 - Feelings of sadness and fear, and states like wakefulness, sleep and anesthesia are controlled by other specific parts of the brain.
- The same is true for motivations like wanting to eat (hunger). The scientific names of these brain areas are given in the drawing. The MPTA (green) is an area deep in the brain which, because of its connections, can apparently turn on and off conscious experiences: sensations, emotions, wanting, memory, and movement.
Turning Pain and Consciousness off and on
If the electrical nerve pulses that reported to your brain that you scraped your knee had been blocked along the way, you would not have felt the pain. You have probably experienced such blocks. Sometimes when you sit for a long time with your legs crossed, one leg “goes to sleep.” If you then pinch the foot, you hardly feel a thing. There are also drugs that block electrical pulses from running along nerves. To prevent pain when drilling a tooth, the dentist usually injects a drug of this sort onto a nerve in your jaw. This stops pain signals from the tooth from reaching your brain and being felt. Women about to deliver a baby are often injected with this same drug to reduce the pain of childbirth. Drugs that block nerve impulses from reaching the brain are called local anesthetics.
Different drugs, called general anesthetics, not only stop pain, but also make emotions, motivations, and even consciousness completely disappear. They make the “you” inside of your head vanish for a time. These drugs put you into a state of nothingness that many people believe must be just like being dead. But general anesthetic drugs do not cause death. The anesthetized brain continues to control breathing, blood pressure, and the many other essential jobs that keep us alive. General anesthetics are very useful because they let doctors perform surgical operations without the patient feeling pain. Normally operations don’t last long. But the death-like state induced by a general anesthetic can be maintained for weeks or months if the drug is given repeatedly. People do not sense the passage of time when they are under general anesthesia. If you ask, the person will probably say that he was asleep for a few minutes, not a few months [3].
How Are Consciousness and Pain Turned off?
Think of a television set: you can switch the TV sound on and off without affecting the picture. Is this how anesthetics turn off only some functions of the brain and not others? When inhaled or injected into a vein anesthetics reach all parts of the brain, but perhaps they do their job only in some parts. With this question in mind our laboratory conducted experiments to discover where in the brain anesthetics work. It took a lot of effort, but after exploring the whole brain, we found one brain location that was special. Injecting a tiny amount of an anesthetic drug here caused rats and mice to stop responding to normally painful pinching of the foot or tail. Injections elsewhere in the brain did not have this effect [4]. We called this special brain location the mesopontine tegmental anesthesia area, or MPTA for short. We also found that destroying the MPTA caused animals to lose their normal sensitivity to anesthetics [5]. Together, these results make us think that the MPTA might act like a switch. When nerve cells in the MPTA are activated by anesthetic drugs, they send electrical signals along nerve fibers within the brain that temporarily turn off pain, consciousness and some other things, without turning off breathing, blood-flow and additional crucial functions that keep us alive.
Temporary loss of the conscious “me” without loss of other key brain functions also occurs during deep sleep, when people faint and after certain types of head injury (concussion). We all roll around in bed while asleep, but our unconscious sleeping brain knows exactly where the edge of the bed is. Except for babies and some patients, we almost never fall out of bed onto the floor. A particularly dramatic example of continued brain activity during unconsciousness is “sleep-walking.” A person may get out of bed, go to the kitchen to prepare a sandwich and then go back to bed, all while fast asleep. Our research suggests that the MPTA may be related to sleep, fainting and concussion, as well as to anesthesia.
What’s Next?
Students in our laboratory are now trying to identify the specific neurons within the MPTA region that are responsible for the brain’s response to anesthetic drugs, and to figure out why anesthetic drugs excite them. We are also trying to discover which areas of the brain these special nerve cells connect to that allows them to control so many of the things that make us human: pleasure, pain, suffering, love, hate, fear, hunger, and so many others. Who knows, perhaps this line of work will some day show how to bring a patient out of coma caused by brain injury, or to turn a person’s pain off completely without making him or her unconscious. The ultimate hope, however, is that experiments of this sort might shine light on the greatest secret of all: how is the experience of being conscious, of being “me,” generated by the brain in the first place. Today, scientists have no idea how electrical pulses circulating in the brain create sensations, emotions, motivations, and consciousness. This is among the biggest mysteries in all of science. But one thing is clear; these things happen in our brain. Someday, someone will figure it out. Maybe it will be you!
Funding
This work was supported by the Fund for Research on Anesthesia at the Hebrew University of Jerusalem and the Hebrew University’s Seymour and Cecile Alpert Chair in Pain Research (to MD). MB and S-lY are recipients of the Dr. Willem Been Legacy Fellowship.
Glossary
Electrical Pulse: ↑ A signal carried by nerve fibers which transmits information within the brain, and between the body and the brain, using brief pulses of electrical current.
Nerve: ↑ A bundle of nerve fibers made up of many individual nerve fibers from many different nerve cells, that conducts electrical pulses over long distances, for example, all the way from the leg to the brain.
Nerve Fiber: ↑ A long, thin, thread-like extension of an individual nerve cell that conducts electrical pulses between nerve cells within the brain, from the brain to the body and from the body to the brain.
Nerve Cell: ↑ A type of cell, also called a neuron, that makes up much of the brain and connects the brain to the rest of the body. Nerve cells communicate using electrical pulses.
Phantom Limb: ↑ The sensation, which is sometimes painful, felt by a person who has lost a limb, usually an arm or a leg. The sensation feels as if it were coming from the missing limb.
Local Anesthetic: ↑ A type of drug that prevents the formation of electrical pulses by nerve cells and blocks the ability of nerve fibers to conduct electrical pulses that have already formed.
General Anesthetic: ↑ A different type of drug that acts within the brain to eliminate sensation (including pain), most types of movement, memory formation, and consciousness.
Mesopontine Tegmental Anesthesia Area (MPTA for Short): ↑ A small region of nerve cells located in a primitive part of the brain called the brainstem. General anesthetics directed to the MPTA cause loss of pain sensation and loss of consciousness.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Vaso, A., Adahan, H. M., Gjika, A., Zahaj, S., Zhurda, T., Vyshka, G., and Devor, M. 2014. Peripheral nervous system origin of phantom limb pain. Pain. 155:1384–91. doi: 10.1016/j.pain.2014.04.018
[2] ↑ Leknes, S., and Tracey, I. 2008. A common neurobiology for pain and pleasure. Nat Rev Neurosci. 9:314–20. doi: 10.1038/nrn2333
[3] ↑ Kelz, M. B., Garcia, P. S., Mashour, G. A., and Solt, K. 2019. Escape from oblivion: neural mechanisms of emergence from general anesthesia. Anesth. Analg. 128:726–36. doi: 10.1213/ANE.0000000000004006
[4] ↑ Minert, A., Yatziv, S.-L., and Devor, M. 2017. Location of the mesopontine neurons responsible for maintenance of anesthetic loss of consciousness. J. Neurosci. 37:9320–31. doi: 10.1523/JNEUROSCI.0544-17.2017
[5] ↑ Minert, A., and Devor, M. 2016. Brainstem node for loss of consciousness due to GABAA receptor-active anesthetics. Exp. Neurol. 275 (Pt. 1):38–45. doi: 10.1016/j.expneurol.2015.10.001