Abstract
Tuberculosis (TB) is a contagious disease that can be transmitted from a person who has the bacteria Mycobacterium tuberculosis within their lungs, and who expels the bacteria by coughing, allowing TB to infect other susceptible people. TB can affect people of all ages, from kids to the elderly, and in infected people, it often spreads to other organs, in addition to the lungs and can even spread throughout the body. Today, the most common way to diagnose TB is by staining the bacteria present in sputum (coughed up mucus) samples, using a chemical that will color those bacterial cells. However, in cases where the bacteria are located outside the lungs, this strategy is not effective. Furthermore, in some cases where coughed up mucus can be obtained, it could contain too few bacteria to easily detect them. Also, there are some people in which M. tuberculosis remains “dormant” or hiding, without causing trouble, but upon weakening of the immune (defense) system, the bacteria “wake up” and cause disease. Because of these complications, new strategies for diagnosis of TB rely on the use of samples other than coughed up mucus, in which M. tuberculosis can be detected using simple tests. In this article, I discuss how the immune response varies from person to person and even within the same person, how the immune response to M. tuberculosis changes with age or other circumstances, and how we could take advantage of these changes to improve diagnosis of TB.
Who Can Get Tuberculosis (TB)?
Although anyone, from kids to the elderly, can come into contact with the bacterium Mycobacterium tuberculosis, the vast majority of people (about 90%) who are infected with this bacterium will eliminate it through the work of the immune system. However, some people (about 10%) who come into contact with M. tuberculosis cannot fully control the bacteria. These people can develop a disease called active tuberculosis (ATB), with fever, coughing, and weight loss. In these cases, M. tuberculosis makes its home within the lungs and can be transmitted to other people when the sick people expel the bacteria through coughing. In some people, another scenario occurs in which their immune system keeps the bacteria in a dormant or “sleeping” state. This is called latent TB. In these people, no fever, coughing, or weight loss will be apparent until their immune system stops working properly.
In spite of the ability of M. tuberculosis to infect pretty much anyone, there are only a few countries that contain the majority of people who have ATB. These countries are generally affected by either overpopulation and/or hunger, or there is a high occurrence of other diseases, such as HIV/AIDS or diabetes mellitus (DM). Overpopulation, hunger, and disease are common in many developing countries, and these conditions make it difficult to stop the disease from spreading. This means that the risk of developing ATB is higher in people who suffer from hunger, poverty, bad diet, or lack of exercise.
How is Active TB Usually Detected?
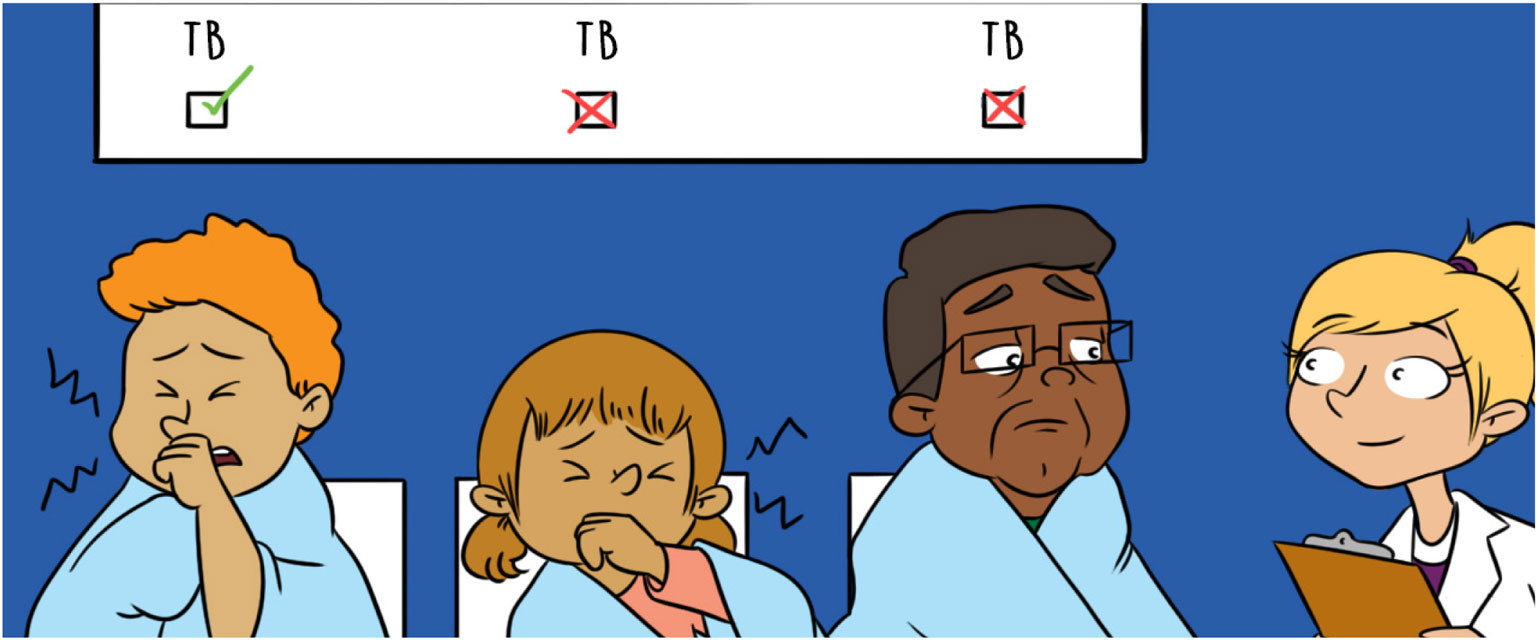
When a person is infected with M. tuberculosis and develop ATB, bacteria often multiply without a great restriction in the body, and often can reach high numbers within the lungs. This results in a good number of bacteria being coughed up as sputum, so that when the secreted mucus is stained in the laboratory, it is relatively easy to find colored M. tuberculosis there (Figure 1). However, some people (for example, kids or the elderly) may not be able to produce the secreted mucus in an amount good enough to conduct the staining, or the number of bacteria being present there could be too low to find them. In some other cases, M. tuberculosis may even be present out of the lungs, so the process for obtaining a sample to stain it becomes more complicated and potentially results in discomfort for a patient. Other bacteria that do not produce ATB can also be detected with the staining used to find M. tuberculosis, therefore the risk for wrong diagnosis exists. These drawbacks call for methods that accurately diagnose ATB to allow patients the chance to be cured.
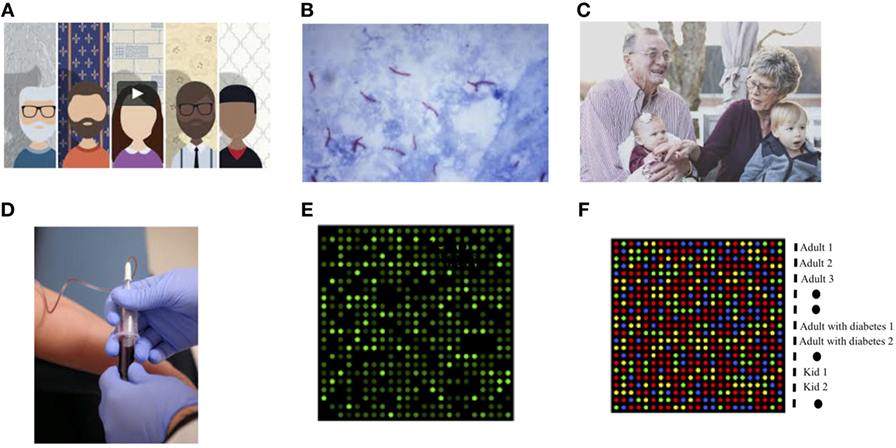
- Figure 1 - Improved diagnosis of tuberculosis for everyone.
- In the near future, it may be possible to detect Mycobacterium tuberculosis no matter where the bacteria responsible for producing it is hidden in the body. As we reach this goal, we will be able to: (A) Better understand why different people respond differently to M tuberculosis, with each one of us producing a unique response to infection. (B) In some cases, when M. tuberculosis is present in large amounts in the lungs, the bacteria can be detected in the sputum (coughed up mucus) using dyes (staining/coloring them). The bacteria in this image are the purple rod-like structures. (C) Not all people are able to produce sputum, and the bacteria are not always present in the lungs. Moreover, as we grow up and depending on other conditions (for example, pollution or food intake), our capacity to produce an antibodies varies. (D) To improve our chances of finding M. tuberculosis, we hope to use other body fluids in addition to sputum (blood, urine, saliva, etc.). If we can detect antibodies to M. tuberculosis in these fluids, the antibodies might indicate that the person is infected with this organism. (E) Antibodies present in body fluids can be used to detect specific structures on M. tuberculosis, and these antibodies can be used to produce a visual signal that can be easily detected. In the example shown, every bright, green dot represents one single structure from M. tuberculosis that is recognized by one of the many human antibodies produced during TB. This image represents a unique antibody fingerprint produced by a single person. (F) Different antibodies will be uniquely present in different people (kids, elderly, diabetic people, etc.), who have TB, and these people would therefore produce their own unique fingerprint. In this example, you can see colored spot representing a combination (pattern) of antibodies from different adults, kids, and patients who also have diabetes (each row represents the pattern of the person listed on the right). As you can see, every person produces a different pattern, indicating that the antibody response varied according to age, gender, and other conditions. The lines with black dots indicate “controls” or samples that would always produce a signal to indicate that the test is working.
How Does the Body React to M. tuberculosis?
The body’s first line of defense against M. tuberculosis is something called innate immunity, which will fight the attempt of M. tuberculosis to establish and maintain an infection. The innate immune response starts with cells and proteins of the immune system that recognize structures present on the bacterial surface. This recognition results in the production, by white blood cells (leukocytes), of a number of compounds that are toxic to bacteria. Moreover, white blood cells also produce additional substances that attract other defense cells, so that the immune cells join forces in an attempt to avoid spread of the invading bacteria to other places in the body.
In most people, innate immunity will lead to the elimination of M. tuberculosis. Conversely, in susceptible people, another kind of immunity called the adaptive immune response will take place, in an effort to contain the infection and optimally, eradicate it at this stage.
In contrast to the innate immune response, the adaptive immune response is based on recognition of unique structures on an invading bacteria, which are not shared by other bacteria in the body. The adaptive immune response stores cells called B lymphocytes that produce substances called antibodies. If the same M. tuberculosis bacteria are encountered again, anywhere in the body, the B lymphocytes will rapidly produce the antibodies needed to fight the battle against those bacteria.
Can We Detect TB by Looking for Antibodies?
As we have already stated, antibodies are substances produced by B lymphocytes. Antibodies are large, Y-shaped proteins that are used by the immune system to bind to specific structures on bacteria like M. tuberculosis, or other infectious organisms, and effectively neutralize their dangerous properties. Antibodies can be found in different body fluids (saliva, blood, tears, and urine) so that in cases where mucus secretion cannot be obtained from a patient, it is still possible to look for an infection. No matter where the M. tuberculosis infection occurs (lungs, liver, stomach, bones, etc.), the immune response produces antibodies that circulate throughout the entire body. This makes antibodies a more effective way to detect M. tuberculosis—especially when it is present in organs other than the lungs. A limitation to the use of technologies based on these compounds is that antibodies can be found even in cases where the harmful bacteria have already been eliminated from our body thanks to our defense system.
We need to be aware that every one of us will react slightly differently to the presence of M. tuberculosis in our bodies, because of inherent differences in our genes. These differences can result in variations in antibody responses [1]. Some people may produce more antibodies than others. Also, as people grow up and age, additional differences in the amount and also the kinds of antibodies produced may occur, due to natural changes in the immune system. Last, malnutrition or diseases like DM may also affect a person’s capacity to produce antibodies to M. tuberculosis.
Because of all these differences, scientists are working to produce different methods to diagnose ATB for different people, for example, to detect antibodies produced by children, patients with diabetes, or the elderly (Figure 1). It could be that we need to look for antibodies that are useful at early, medium, and late stages of TB disease.
In my research group, we are trying to use the presence of antibodies to detect M. tuberculosis in patients who have DM. DM is a disease where blood sugar is higher than in normal people, and that among other characteristics, reduces the capacity of the immune system of these patients to fight infections, including ATB. At this point, we do not know whether people with DM will produce antibodies against M. tuberculosis, so we are studying this question and hope to discover an effective method to detect M. tuberculosis in patients with DM before ATB has developed in them.
Glossary
Immune System: ↑ The network of cells, tissues, and organs that work together to protect the body from infectious agents.
HIV/AIDS: ↑ Infection and disease produced by human immunodeficiency virus (HIV) that produces acquired immune deficiency syndrome (AIDS), a severe condition that reduces capacity to fight infections.
Diabetes Mellitus: ↑ A chronic condition where abnormally high levels of sugar (glucose) are present in blood, which, among other effects, reduces the capacity of immune cells to fight infections.
Sputum: ↑ A mixture of saliva and mucus coughed up from the airways.
Staining: ↑ Use of dyes that binds to components present in cells, which facilitate their visualization under a microscope.
Innate Immunity: ↑ The first line of defense against invading pathogens, also known as non-specific immune system or in-born immunity system.
Adaptive Immune Response: ↑ Also known as the acquired immune system, composed of highly specialized, systemic cells and processes that eliminate pathogens or prevent their growth.
Antibodies: ↑ Large, Y-shaped proteins produced mainly by B lymphocytes that are used by the immune system to neutralize pathogens, and that recognize specific structures on an infecting organism.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgements
I am indebted to my son, Xavier A. Flores-Barba, for being my inspiration for this work. The National Council of Science and Technology (GACD-FONCICYT-CONACYT, project # 265796) in Mexico provides financial support for starting my quest for new methods to diagnose tuberculosis, focused in early detection in people living with diabetes mellitus.
Reference
[1] ↑ Kunnath-Velayudhan, S., Salamon, H., Wang, H. Y., Davidow, A. L., Molina, D. M., Huynh, V. T., et al. 2010. Dynamic antibody responses to the Mycobacterium tuberculosis proteome. Proc. Natl. Acad. Sci. U.S.A. 107:14703–8. doi:10.1073/pnas.1009080107