Abstract
The immune system defends us and combats many microbes, like the viruses that cause the common cold or bacteria that enter wounds. Our defenses can also learn to protect us from more difficult situations—and they can do so with the lessons learned from vaccines. For example, the poliovirus vaccine teaches the immune system to recognize and eliminate the poliovirus, in case it ever enters the body. In recent years, scientists have found that the immune system can also be taught to attack another type of disease: cancer. Cancer is a big mistake in our body. It happens when cells lose control and start to grow without limits. The good news is that we can educate the immune system in cancer patients—this is called immunotherapy. In this article, we will explain how our defenses can learn to attack and eliminate cancer.
Cancer: When the Body Loses Control
Cancer is a serious disease that affects many people. We may know people around us who have long and difficult battles against cancer and eventually may die. However, not all cancers are the same. There are many different forms of cancer and they do not all necessarily cause death. The severity greatly depends on the type of cancer, the treatments used and, especially, how early it is detected.
What is cancer? This word originates from the Greek word “karkinos,” which means “crab”. It is said that, in ancient times, the Greek doctor Hippocrates first compared this disease to a crab, seeing sick parts of the body of his patients that were hard as a rock, which caused pain like a crab’s pinch and could extend to invade other body regions. In biology, cancer is a big mistake: cells start to grow without control within the body. Starting when a baby is conceived, every part of the body grows and develops under strict control. This control shapes our fingers, our bones, our brains, all our organs. In fact, the type of cancer that grows depends on the type of cell that makes a mistake and loses this control. For example, we can have cancer of the brain (neuroblastoma), cancer of the bone (osteosarcoma), or cancer of the skin pigment cells, called melanocytes (melanoma). Often, the cause of the cancer is unknown, or is due to multiple mistakes that accumulate. Sometimes, we know why cancer happens: there are certain things that damage the body and break the mechanisms of control. For example, cigarette smoke can cause lung cancer and too much sun exposure can cause skin cancer.
Immunotherapy: The New Treatment Against Cancer
Many options exist to treat cancer. These options include surgery when the cancer is in a place that surgeons can safely cut out, therapy with radiation (radiotherapy), or therapy with chemicals (chemotherapy). What treatment do we choose for a given patient? This choice depends on several things, such as the type of cancer and the stage of the disease (meaning how advanced the loss of control and the cancer growth is).
In recent years, scientists have discovered more and more proof that cancer can also be attacked by our own defenses: the immune system. Therapy based on our immune system is called immunotherapy. Immunotherapy mainly relies on a very specialized type of white blood cell called the cytotoxic T cell and the way it works is described in the sections below.
Cytotoxic T Cells Can Eliminate Cancer and Help Patients
T cells are the special forces of our immune system: like the police, T cells patrol the body to find harmful invaders (Figure 1A). Each T cell is equipped with a special radar called the T cell receptor (TCR) that allows it to recognize one specific invader. TCRs determine if the body’s cells are healthy by checking their identity (ID), which is given by a molecule called the major histocompatibility complex (MHC). Each cell in the body loads bits of itself on its MHC, and thus presents a general picture of its ID when it interacts with a TCR. These bits of the cell are called antigens, because they can generate an immune response (anti-, against and -gen, generate) when the T cell reacts to them. In addition to the TCR radar, T cells also have weapons to eliminate invaders: the T cells can be cytotoxic (“cytos” is Greek for cell), which means they can kill cells. When they are on patrol, the T cells verify that the body is healthy by checking the ID of the body cells (Figure 1A). If a cell is infected and is sick, it will show its MHC with bits of the infectious microbe, and this will change its ID, making it look strange. When a T cell detects such a change of ID, it gets activated and kills the sick body cell, including the infectious invader that is inside. This way, the spread of the invader to the rest of the body is prevented.
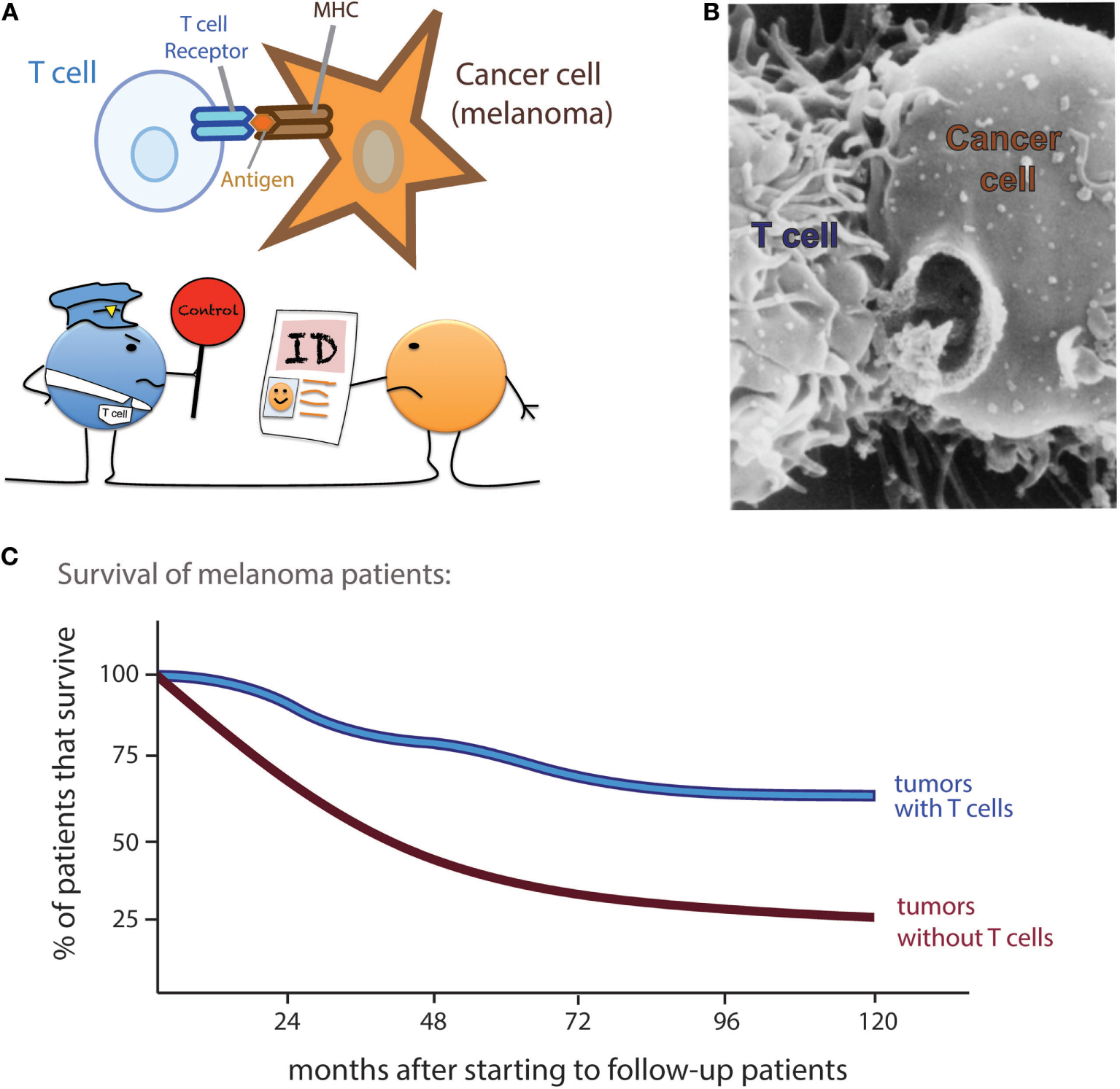
- Figure 1 - T cells can detect and kill cancer cells, helping patients to survive longer.
- A. T cells have specific T cell receptors to detect sick cells. A cell shows its identity (ID) by displaying bits of itself (antigens) on major histocompatibility complex (MHC). A cell that is sick shows an altered ID and T cells become activated. B. A real picture of a T cell making a hole on a cancer cell, taken using an electron microscope (with permission from http://lib.jiangnan.edu.cn/ASM/350-Introduce.htm). C. When doctors followed up patients, it was discovered that patients who have T cells in their tumors survive longer than patients who have tumors without T cells (these data are taken from a study of melanoma patients [1]).
How does a T cell kill a sick cell? Imagine it like punching a hole in a water balloon (Figure 1B). The T cell weapons are substances called perforins, which make the holes, and granzymes, which create general destruction inside the attacked cell.
So, this is how T cells recognize and eliminate invaders. But cancer cells are not microbial invaders: they are sick cells that develop from normal body cells due to mistakes in their growth and development. Usually, our T cells do not see that the cancer cells are bad, because the cancer cells do not invade our body from the outside. Luckily, there are exceptions to this invader rule: when cancer cells behave very suspiciously and they show an unusual, sick ID as compared with healthy cells. Then, T cells can also recognize these sick cancer cells and kill them.
How do we know that T cells can fight cancer? Scientists have noticed that cancer patients who have activated T cells survive longer. By comparing the tumors of many cancer patients, it was found that patients whose tumors contained a lot of T cells survived longer than patients whose tumors did not contain T cells (Figure 1C) [1]. So, it is a big benefit for cancer patients when patrolling T cells see the cancer cells and go inside tumors to kill the sick cancer cells.
Immunotherapy Can Teach T Cells to Recognize Cancer, and T Cells Will Remember, for Many Years!
Why do some cancer patients naturally have good patrolling T cells that can kill the sick cancer cells, while other patients do not? This is a question that is still under intense investigation. The good news is that scientists have found methods to teach the immune system to recognize cancer and to teach T cells to eliminate tumors, even in patients who don’t have good T cells to start with. This type of therapy, based on the education of the immune system to combat disease, is called immunotherapy.
The big advantage of immunotherapy is that it not only teaches the immune system to fight cancer once but also the T cells actually remember, and for many years! Teaching T cells to fight cancer is similar to using vaccines to teach T cells how to fight microbial infections. Vaccines are substances that generate specific immune responses against a given disease; they are usually made of only a part of the microbe that causes the disease, or a modified version of that microbe. For example, the vaccine against poliomyelitis is made by preparing an inactivated (killed) form of the poliovirus itself. When this inactivated poliovirus is injected, it cannot infect us because it is dead, yet, the immune system sees the poliovirus and learns to recognize it. Once vaccinated, if we ever become infected with poliovirus, the immune system remembers and reacts quickly, eliminating the poliovirus before it can reproduce inside of us and cause disease. This capacity of the immune system to learn and remember what should be eliminated is called immunological memory.
Just as a vaccine can teach the immune system to eliminate a virus, we can use immunotherapy to teach the immune system how to better combat cancer. Patients can be injected with immunotherapy treatments that will teach specific T cells to multiply and attack the cancer cell (Figure 2A). Once the cancer is eliminated, the specific T cells will calm down and remain in the patients’ bodies in the form of memory T cells (Figure 2B). These memory T cells will continue to patrol the body. If they ever encounter the same cancer cells again, even at a distant or different location (known as a metastasis), the memory T cells will remember this cancer and quickly reactivate to attack again (Figure 2C).
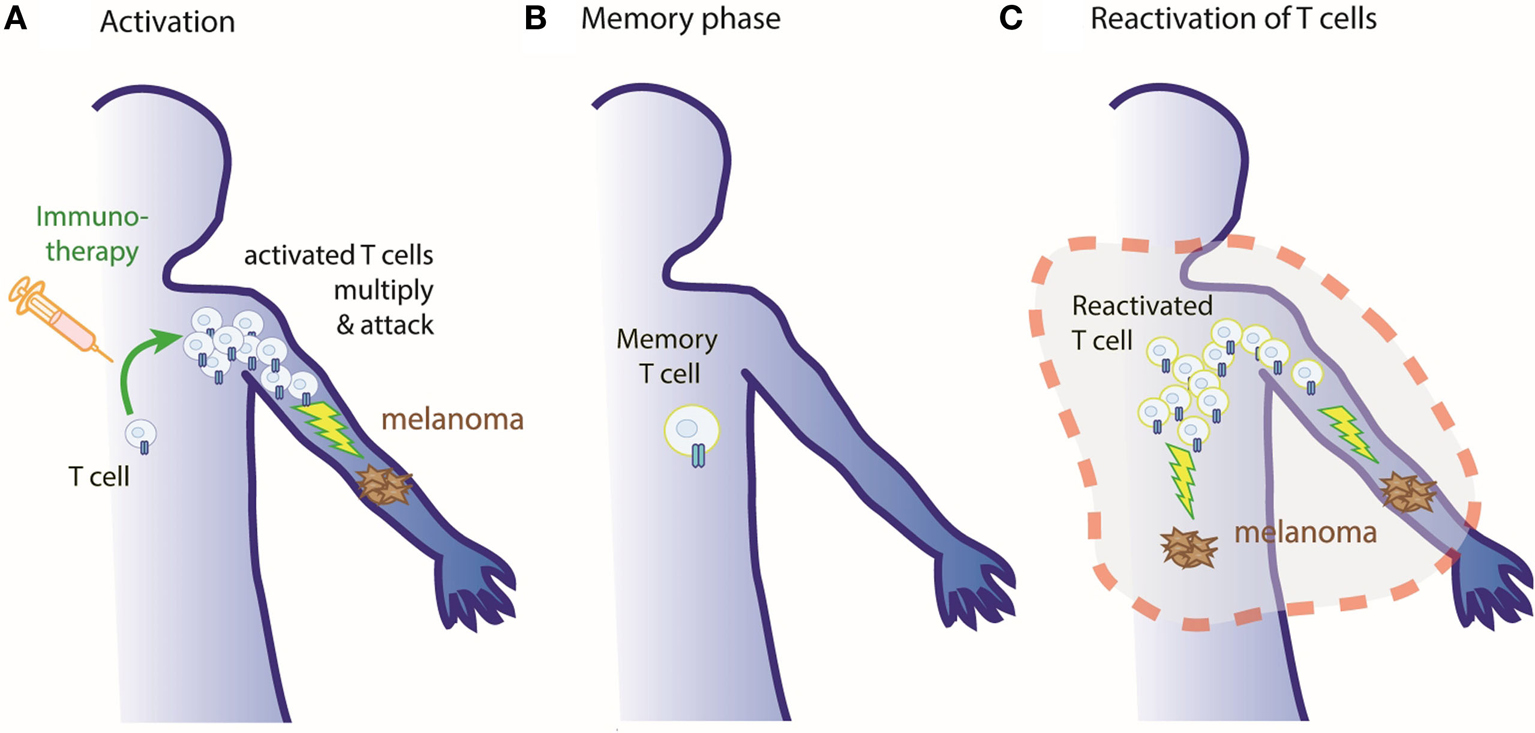
- Figure 2 - Our immune system remembers!
- A. Cancer patients can be treated with immunotherapies to activate anticancer T cells, which recognize and kill the tumors. B. Once the tumor has been destroyed, T cells go back to rest and can remain in the body in a state called memory. C. If the tumor comes back (even in different or distant parts of the body), memory T cells remember how to detect and kill these sick cancer cells and are reactivated to first multiply themselves and then attack the tumor once again.
The fact that the immune system remembers for many years brings the big advantage that the effects of immunotherapy last for a long time. This is in contrast to other treatments such as radio- or chemotherapies, which must be repeated in the patient if the cancer comes back. In fact, the immune system can keep this immunological memory throughout the patient’s lifetime.
There Are Different Types of Immunotherapy, Depending on the Type of Cancer and the Patient
So what is immunotherapy? What is actually injected into the patient?
There are several possible reasons why the immune system cannot see or cannot kill cancer cells. So, there are several possible methods to help the immune system to recognize and attack the cancer cells. Remember that cancer cells can be very different from one another, depending on the person and the cancer type. The general goal of immunotherapy is to educate the immune system to attack the cancer. This can be done with many different types of injections. In fact, there are thousands of different types of immunotherapies being studied for different types of cancer by researchers around the world.
Table 1 gives four different examples of immunotherapies and describes how they work. The last example has been especially successful in recent years, and will be explained in more detail in the following section (also see Figure 3).
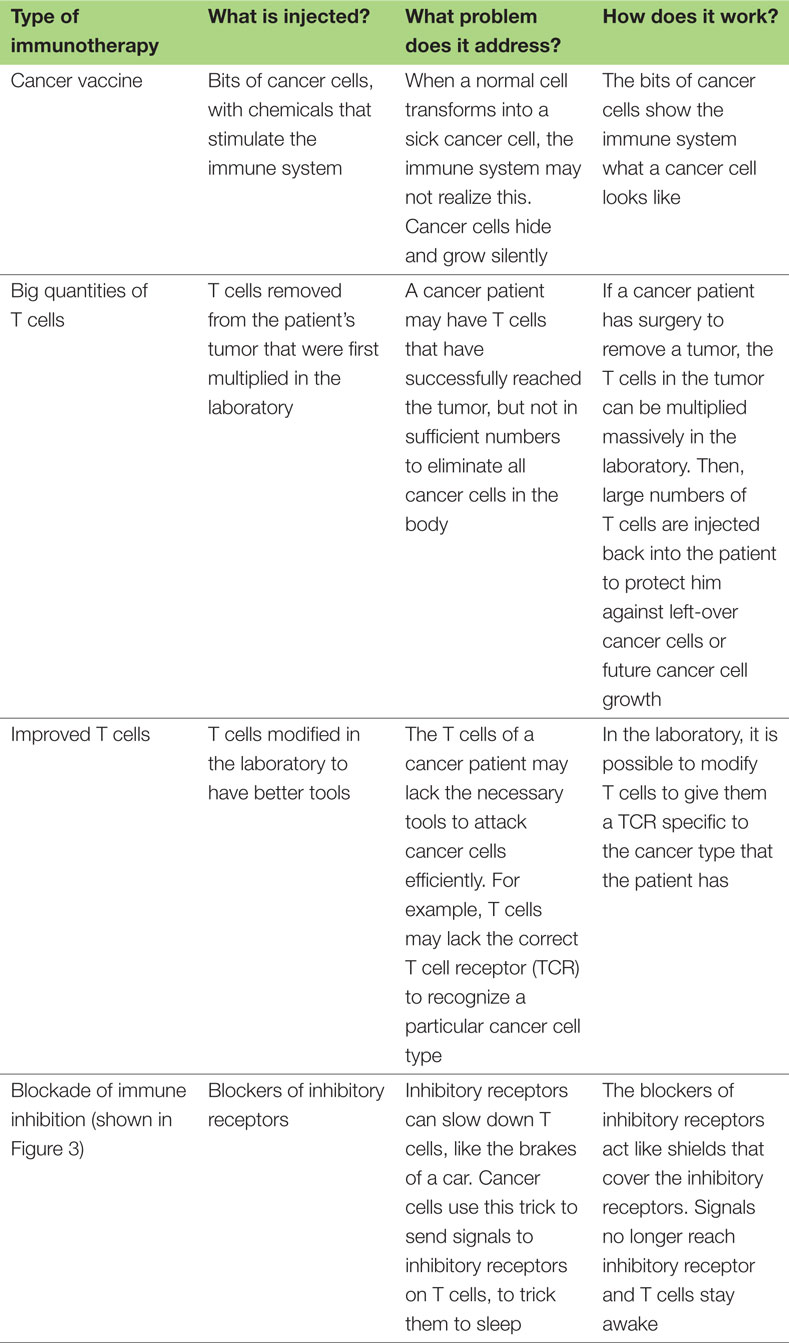
- Table 1 - Examples of immunotherapy: what they are and how they work.
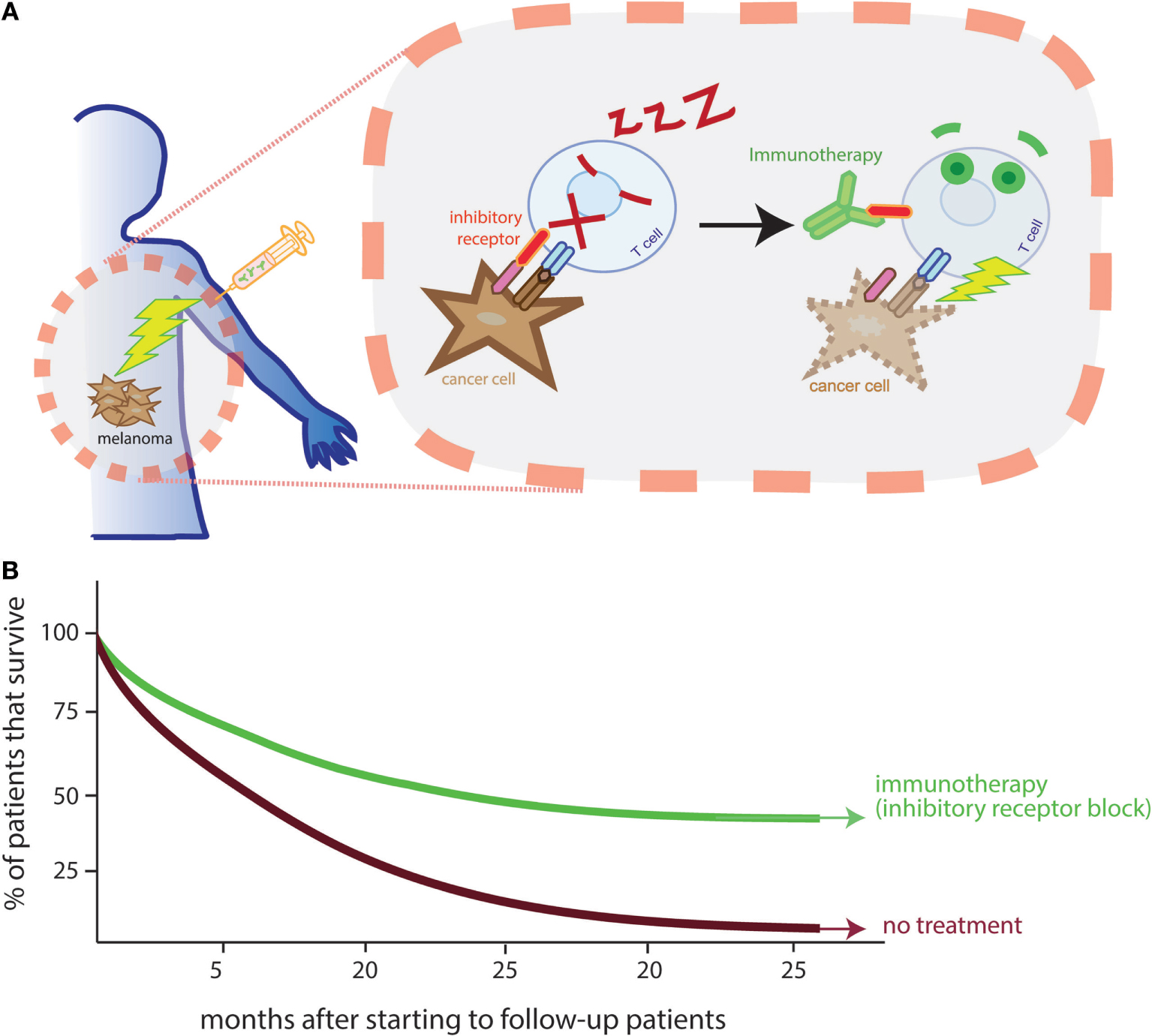
- Figure 3 - Immunotherapy can awaken T cells to kill tumors.
- A. T cells naturally have inhibitory receptors (shown in red, on the T cell surface) that act like brakes to control their speed. Cancer cells can escape by sending signals (in pink, on the cancer cell surface) to these brakes and thus putting T cells to sleep. There are immunotherapies that can block inhibitory receptors (in green, binding to the inhibitory receptor), releasing the brakes, and awaking T cells. B. Patients who receive immunotherapies that block inhibitory receptors survive longer (these data are taken from a study of melanoma patients [2]).
T Cells Can Get Exhausted Fighting Cancer, but Immunotherapy Can Awaken Cytotoxic T Cells to Help Cure Patients
So, if our immune system can kill cancer, why do we get cancer at all? Cancers are very sophisticated—they can escape from the immune system using different tricks. As we saw in Figure 1, T cells patrol the body, checking cells for healthy or strange ID. One way for the cancer cell to escape the T cell attack is by simply hiding its sick bits.
Another escape strategy used by cancer cells is that the cancer cells put the T cells to sleep. This trick is actually stolen from healthy body cells. Normally, when the body fights the invasion of a common cold virus, the T cells become activated and kill all sick cells that have been invaded by the virus. Once all the viruses and sick cells have been eliminated, something has to tell the T cells that they have done their job and that they should go back to rest. Just like cars have brakes to control the speed at which we drive, T cells have special so-called inhibitory receptors to control their activity [3]. In the absence of viruses, the healthy body cells slow down the activated T cells by sending a signal to their inhibitory receptors. The clever cancer cells use this trick and can do the same thing: they can send signals to the inhibitory receptors of the T cells. In fact, T cells can spend long periods of time trying to kill cancer cells—the cancer cells meanwhile send inhibitory signals and put the T cells to sleep (Figure 3A).
So, sometimes a cancer patient can have a lot of T cells that can recognize the cancer cells, but then, the cancer cells use tricks to escape from T cell attack. Cancer cells may even escape after immunotherapy that activates new T cells, by putting all (including new) T cells to sleep! But, another type of immunotherapy can stop this trick! There are now new drugs that can block the inhibitory receptors on T cells (Figure 3A). With this blockade, the cancer cells cannot put the T cells to sleep anymore. T cells stay activated and continue to kill the cancer cells. This new blockade immunotherapy has been very successful—it really gives cancer patients a chance to live longer (Figure 3B) [2]. Blockade immunotherapy has been so important that it was elected as the Breakthrough of the Year in 2013 by one of the top science magazines, called “Science”.
Conclusion
The immune system has the potential to eliminate cancer. The treatments that activate the immune system and teach it to recognize cancer cells are called immunotherapy. The big advantage is that the immune system has the capacity to remember. Once it learns to attack a certain type of cancer, it can continue to do so for many years. There are now several types of immunotherapies that are being used and developed to treat cancer patients. Recent exciting immunotherapy treatments help to block the inhibitory signals from cancer cells that put T cells to sleep. This immunotherapy can be used to reawaken T cells and allow them to re-attack the cancer cells. In some patients, the anticancer effects of immunotherapy are spectacular, but in other patients, we still do not know how to activate the immune system effectively against cancer. Researchers are intensively investigating how to further improve immunotherapy, based on the news that the immune system is a very promising tool for the treatment of cancer patients.
Glossary
Cancer: ↑ A disease that occurs when cells in the body lose control and grow without limits. Cancer cells may form masses that are called tumors.
Immune system: ↑ The group of components in the body that work to defend the organism from invasions and disease. The immune system includes the skin barrier and the mucous membranes, substances called antibodies, and white blood cells, which include T cells.
Immunotherapy: ↑ Treatments based on the education of the immune system to combat disease.
Cytotoxic T cell: ↑ A type of white blood cell that has radars called TCR to specifically recognize sick cells, such as infected or cancer cells, and can eliminate them.
Immunological memory: ↑ The capacity of the immune system to learn how to attack a given microbe or sick cancer cell, and to remember this forever.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Clemente, C. G., Mihm, M. C., Bufalino, R., Zurrida, S., Collini, P., and Cascinelli, N. 1996. Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer 77:1303–10. doi:10.1002/(SICI)1097-0142(19960401)77:7<1303::AID-CNCR12>3.0.CO;2-5
[2] ↑ Hodi, F. S., Chesney, J., Pavlick, A. C., Robert, C., Grossmann, K. F., McDermott, D. F., et al. 2016. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 17(11):1558–68. doi:10.1016/S1470-2045(16)30366-7
[3] ↑ Fuertes Marraco, S. A., Neubert, N. J., Verdeil, G., and Speiser, D. E. 2015. Inhibitory receptors beyond T cell exhaustion. Front. Immunol. 6:310. doi:10.3389/fimmu.2015.00310