Abstract
Receiving an organ transplant provides people with an opportunity to be healthy. When young people receive transplants, they face unique challenges beyond the typical medical challenges all transplant patients experience. The overall goal of transplantation is health and life satisfaction. So, our research aimed to describe the main concerns among 14–25-year-old young people who have received transplants. Based on surveys, interviews, and a workshop attended by 44 young people, we identified nine major types of concerns. In this article, we will describe some of these concerns and what can be done to improve the health and life satisfaction of young transplant recipients.
Introduction
Spending time in a hospital due to illness and disease is challenging, especially for young people. Undergoing an organ transplant, which means replacing a broken organ with a new one, is an experience that affects everyday life, including spending time with friends, going to school, and maintaining an active lifestyle. The four most common organs transplanted are the kidneys, liver, heart, and lungs. Often, transplantation cannot happen immediately—many people have to wait months to years until an organ is available (Figure 1).
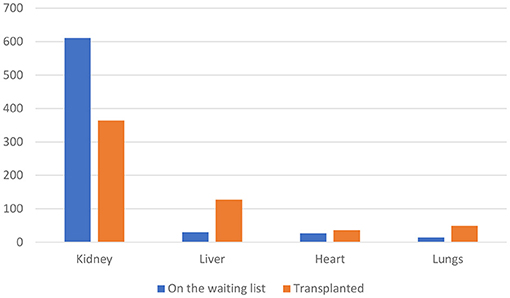
- Figure 1 - The kidneys, liver, heart, and lungs are the most common organs transplanted.
- This graph shows the number of people transplanted in Sweden as of October 2024, and the number still waiting for an organ.
After transplantation, essential medicines must be taken, and the young person must go for many check-ups to ensure that everything is fine. When scientists study life after transplantation, they mainly focus on survival and the negative effects of the medications that prevent the body from attacking the organ, which is called graft rejection. Such side effects can include kidney problems, heart disease, diabetes, and cancer. Taking the medications as prescribed to prevent graft rejection is a particular challenge for young people [1]. While most teens get jobs or go on to college when they grow up, those who have been transplanted are vulnerable by means of being sensitive to infections or dealing with side-effects of their treatment [2]. Problems that might reduce quality of life among kidney-transplanted young people are concentration difficulties and hyperactivity [3]. However, when they reach adulthood, people who got transplants as kids report the same quality of life as other people [4]. Because quality of life is the main goal, it is important to ask young people with transplants about their main concerns. The aim of this article is to describe the main concerns among people transplanted when they were 14–25 years old. We also hope to raise awareness of transplantation among young people and reduce the sense of loneliness that young people with organ transplants may feel.
How We Studied Young People’s Concerns
In this Swedish study, we approached four target groups: teenagers either 14–17 years old or 18–25 years old who were either transplanted or on the waiting list for transplantation, young adults older than 25 who were transplanted when they were younger, and parents with transplanted children younger than 25 years old. A total of 44 young people aged 14–25 participated in the project, which involved questionnaires, interviews, and workshops. Fifty percent of the participants were women, 41% were men, and 9% chose not to state their gender. The study was organized by the Swedish organization More Organ Donation (MOD).
Key Areas of Concern
The key areas of concern for our study participants are illustrated in Figure 2.
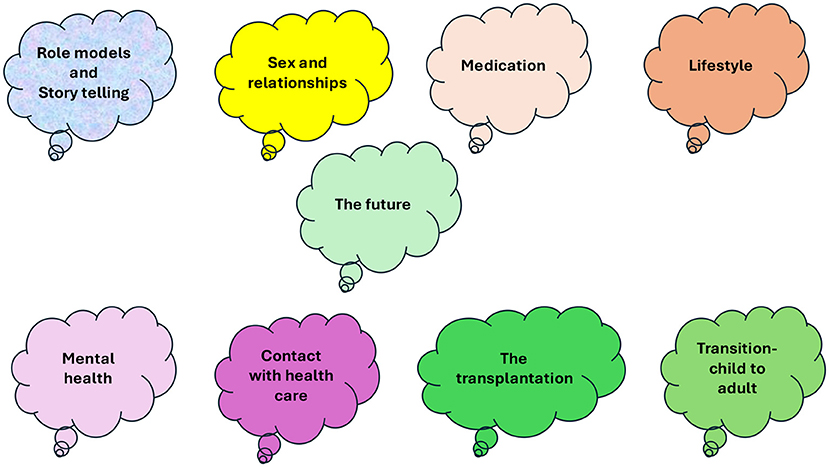
- Figure 2 - Key concerns among young people who are on the waiting list for transplantation or who were transplanted when they were younger than 25 years old.
Transition
One of the biggest challenges for young people who have received transplants seems to be the transition from the pediatric clinic to the adult clinic for follow-up. Evidence from young people and their families tells us that this is a time when young people are gaining their independence, and they might feel powerless on the one hand and overwhelmed on the other [5]. One participant aged between 14 and 17 years described it as follows:
“It would be very helpful if you could meet the new staff in the adult facilities before you are transferred.”
Some participants said that they felt lonely and abandoned when they moved to the adult clinic, and that more preparation and support would have been helpful. They felt that they were much better cared for when they were children. Thus, there is a need to “bridge the gap” between the pediatric clinic and adult care follow-up [6].
Information Needs
Children or teenagers who receive organ transplants need information about various things to make their everyday lives work (Figure 3).
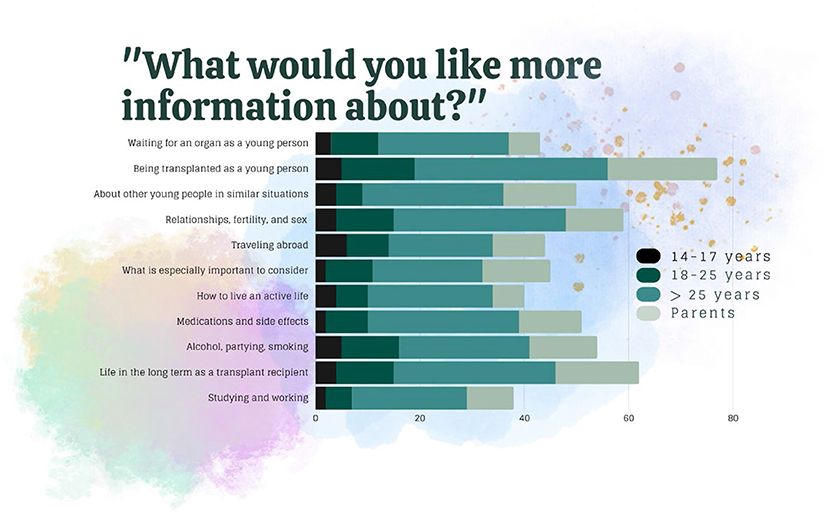
- Figure 3 - Key areas for which young people want information after transplantation.
Some found it difficult to ask healthcare professionals about their concerns and worried about the transition to adult care. Sometimes they noticed a negative approach toward adolescents. The need for information varied based on personal preferences and sometimes young people felt more in control of their situations than their parents did. In talking about school, one adolescent said,
“It would be great to have information about how to keep up with school when you are absent frequently and sometimes for a long period of time.”
Other areas of concern were sex and emotions. Some transplanted young people found it difficult to talk to people who did not have the experience of being transplanted. Some participants described difficulties concentrating and said they felt mentally worse after the transplantation than before. Some felt that nobody asked about their emotions, and some were embarrassed during certain interactions with healthcare professionals, as in the following example:
“They told me I got my urinary tract infection because I had had sex. It made me feel really guilty.”
Some female participants experienced that healthcare professionals focused more on preventing pregnancy than on conversations about sex and relationships relevant to transplanted teenagers or young adults.
Lifestyle and Future
Young people basically want to lead normal lives, meaning they want to be able to do the things everyone else does. Participants in our study mentioned several key concerns regarding lifestyle and their future. Lifestyle issues included sunbathing, leisure activities, traveling, swimming in the sea, physical exercise and training, dietary recommendations, drinking alcohol, partying with friends, and smoking. Aspects of the future included what and where to study, starting a family, career choice, getting a driving license, and contacts with school about their studies. Dreams of future careers were sometimes shattered, as illustrated by the following:
“My dream has always been to become an au pair. But my physician told me that as a transplanted person, I cannot go outside Scandinavia.”
Another participant said,
“I cannot work as a carpenter, pre-school teacher, at construction sites, or as a lorry driver.”
Suggestions for Improvement
According to our young study participants, there is room for improvement in post-transplant care for young people. They suggested making films about life as a young, transplanted person and creating places where they could meet other young transplant recipients. Participants also wished for mentors of their own age. Interviews with experts on sex and relationships were requested, as well as more information about medications and their side effects. Some participants wanted to talk to teenagers who had stopped taking their medications for a while, to learn about the consequences.
When processing their plans for their future, participants wished to interview adults with fun or exciting jobs and those with regular jobs, in addition to someone who had studied abroad. In terms of their mental well-being, participants wanted a list of people they could contact when feeling lonely or sad. They also wanted to listen to “success stories” from other transplanted people talking about emotional strategies. Role models were essential, as well as keeping up leisure activities such as training.
Improving Life After Transplantation
Because the transition from the pediatric to the adult clinic is challenging, efforts have been made to improve this passage in young adults’ care pathways. For example, a transition coordinator could organize the transfer to the adults’ clinic [7]. Since there is a relationship between mental distress and difficulties taking medicine as prescribed [8], paying attention to how the young person feels is essential. Listening to the concerns of young people regarding the transition is important [9]. However, readiness for transition can be measured using the Transition Readiness Assessment Questionnaire [10]. It is also possible to learn about young patients’ perspectives using what are called patient-reported outcome measures (PROMs), which are questionnaires focusing on the young person’s wellbeing. PROMs can play an important role in involving the teenagers, capturing their experiences, and improving their care [11].
Overall, new, creative ways of organizing care for teens with organ transplants are needed. For example, when nurses regularly follow up with young people who have received transplants, the focus is more on the young peoples’ everyday life [12, 13]. When nurses focus on building relationships with young adults rather than focusing just on medical tasks, they can establish trust, help young adults to be more capable improve their satisfaction with care, increase the chances that they will follow medical instructions, and optimize their quality of life [13].
In conclusion, young people seeking quality of life after transplantation clearly have many concerns. They need role models and peers to identify with, as well as expert opinions to help them understand what to expect after transplantation and what is possible in terms of lifestyle and the future. As healthcare professionals, we can learn from these young people—their perspectives of what is important should guide what we do in the clinic. After transplantation, follow-up routines based on young peoples’ needs could be the best way to support a high-quality life full of joy and satisfaction.
Glossary
Organ Transplant: ↑ When a non-functioning organ is replaced by an organ that works.
Graft Rejection: ↑ When the immune system tries to attack the new organ.
Transition Coordinator: ↑ A person that helps young people when they are transferred to adult care.
Patient-Reported Outcome Measures: ↑ Explains how patients experience their health as expressed by themselves.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Campagna, B. R., Weatherley, K., Shemesh, E., and Annunziato, R. A. 2020. Adherence to medication during transition to adult services. Paediatr. Drugs. 22:501–9. doi: 10.1007/s40272-020-00414-2
[2] ↑ Pankhurst, T., Evison, F., Mytton, J., Williamson, S., Kerecuk, L., Lipkin, G., et al. 2020. Young adults have worse kidney transplant outcomes than other age groups. Nephrol Dial Transplant. 35:1043–51. doi: 10.1093/ndt/gfaa059
[3] ↑ Durish, C. L., Lin, J., Pol, S., Damer, A., Anthony, S., Wray, J., et al. 2022. Quality of life and psychosocial outcomes of adults who were pediatric solid organ transplant recipients. A systematic review. Ped. Transpl. 27:14448. doi: 10.1111/petr.14448
[4] ↑ Bulut-Demir, M. H., Taner, S., Demir, H. B., Tasdemir, A. I., Keskinoglu, A., Kaplan-Bulut, I., et al. 2023. Quality of life and psychological well-being in children and adolescents after renal transplantation. Transpl. Proc. 55:1160–5. doi: 10.1016/j.transproceed.2023.04.022
[5] ↑ Dallimore, D. J., Neukirchinger, B., and Noyes, J. 2018. Why is transition between child and adult services a dangerous time for young people with chronic kidney disease? A mixed-method systematic review. PLoS ONE. 13:e0201098. doi: 10.1371/journal.pone.0201098
[6] ↑ Harden, P. N., Walsh, G., Bandler, N., Bradley, S., Lonsdale, D., Taylor, J., et al. 2012. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. 344:e3718. doi: 10.1136/bmj.e3718
[7] ↑ Annunziato, R. A., Parbhakar, M., Kapoor, K., Matloff, R., Casey, N., Benchimol, C., et al. 2015. Can transition to adult care for transplant recipients be improved by intensified services while patients are still in pediatrics? Prog. Transplant. 25:236–42. doi: 10.7182/pit2015599
[8] ↑ Annunziato, R. A., Arrato, N., Rubes, M., and Arnon, R. 2015. The importance of mental health monitoring during transfer to adult care settings as examined among paediatric transplant recipients. J. Paediatr. Child Health. 51:220–2. doi: 10.1111/jpc.12765
[9] ↑ Wright, J., Elwell, L., McDonagh, J. E., Kelly, D. A., and Wray, J. 2016. “Are these adult doctors gonna know me?” Experiences of transition for young people with a liver transplant. Pediatr. Transplant. 20:912–20. doi: 10.1111/petr.12777
[10] ↑ Parfeniuk, S., Petrovic, K., MacIsaac, P. L., Cook, K. A., and Rempel, G. R. 2020. Transition readiness measures for adolescents and young adults with chronic health conditions: a systematic review. J. Transit. Med. 2:1. doi: 10.1515/jtm-2020-0020
[11] ↑ Anthony, S. J., Stinson, H., Lazor, T., Young, K., Hundert, A., Santana, M. J., et al. 2019. Patient-reported outcome measures within pediatric solid organ transplantation: a systematic review. Pediatr. Transplant. 23:6. doi: 10.1111/petr.13518
[12] ↑ Betz, C. L., Smith, K. A., Van Speybroeck, A., Hernandez, F. V., and Jacobs, R. A. 2016. Movin’ on up: an innovative nurse-led interdisciplinary health care transition program. J Pediatr. Health Care. 30:323–38. doi: 10.1016/j.pedhc.2015.08.005
[13] ↑ Gabay Gillie, G., Tarabeih M. 2020. “A bridge over troubled water”: nurses’ leadership in establishing young adults’ trust upon the transition to adult renal-care - a dual-perspective qualitative study. J. Pediatr Nurs. 53:e41–e48. doi: 10.1016/j.pedn.2020.02.004
