Abstract
Palliative care is a type of healthcare focused on improving the quality of life for people with serious illnesses and their families. It helps manage pain, reduce symptoms, and provide support for emotional, social, and spiritual needs. Palliative care is not just for the final stages of life—it can help at any point during an illness. A team of professionals, including doctors, nurses, psychologists, and social workers, works together to give personalized care and support. They also help the patient’s family cope with challenges during this difficult time. By focusing on comfort, dignity, and wellbeing, palliative care ensures that no one faces their illness alone. It also reminds us that being kind and helping others is an important part of healthcare. However, there are challenges, like not having enough resources or how hard it can be for professionals to handle the emotional side of their work.
Compassionate Care During Serious Illnesses
Imagine you had a career fair at your school, where parents were invited to talk about what they do and answer questions. You have always been curious about what Linda, your best friend Peter’s mother, does. Peter mentioned that she is a palliative care nurse and explained that she helps people during the final stages of their lives. Have you ever heard of palliative care? What questions would you ask if you knew someone who worked with people during the final stages of life?
Now imagine having the chance to talk to Linda. “What is palliative care?” you ask, curious. “The meaning of ‘palliative’ is to protect”, Linda responds (Figure 1). “The word comes from the Latin ‘pallium’, which was the cloak knights wore to protect themselves from storms during their journeys. Protecting someone is a form of care, and palliative care aims to relieve pain and suffering, whether physical, psychological, social, or spiritual”. She pauses to see if you are following and continues: “When you hear that someone you know is eligible for palliative care, there is nothing to fear [1]. Many people think palliative care is only for the final moments of life, but that is not quite true. It is for any stage of a serious illness, to help improve quality of life”.

- Figure 1 - The “heart” of palliative care.
- This word collage illustrates some of the important qualities and aspects of palliative care.
Help With All Aspects of Life
Still curious about palliative care, you ask Linda “What exactly does receiving palliative care mean?” Linda smiles and explains, “Receiving palliative care does not mean there is nothing more that can be done for the patient or their family. It means there is a serious chronic illness that threatens life, and a team of specialized professionals will care for the sick person and those around them. In other words, there is still much to do for the patient”. Linda continues, “Now, think about how difficult it must be to receive such a diagnosis. Besides the physical symptoms of the illness, people start to deal with fears about death, concerns about leaving family unsupported, past conflicts, and even practical problems like needing to take time off work and decreased income”. She continues, “These issues are complex and cannot be handled by a single professional. That is why palliative care teams are made up of several specialists, in what is called an interdisciplinary approach, where doctors, nurses, psychologists, social workers, and other specialists work together. Each professional brings their expertise to care for the patient from every angle, addressing the full spectrum of needs”.
Details of the Palliative Care Team
Even more curious, you ask, “So, how does the palliative care team work exactly?” Linda explains, “The palliative care team understands that a serious illness affects patients and those who love them. Our role is to care for everyone involved, and that is why our team is so diverse (Figure 2)”. She pauses to ensure you are following, then continues, “Each of us has a specific role to meet the diverse needs of patients and their families. For example, palliative care doctors focus on the patient’s physical comfort—relieving pain and reducing discomfort caused by the illness or treatment. Nurses help monitor the patient’s health and administer necessary treatments. Physiotherapists work to improve the patient’s mobility and strength, helping them feel more comfortable and independent. Psychologists”, Linda continues, “offer emotional support to deal with the stress and anxiety that come with the illness. Occupational therapists help patients maintain their independence in daily activities, while chaplains provide spiritual support for those who need it. Social workers assist with practical and legal issues”. You are impressed with the number of professionals involved. “Wow, it is a big team working together to help the patient”, you say. “Yes”, Linda responds. “Our goal is to ensure that the patient and their loved ones receive all the necessary support to face the situation in the best possible way. We work together to reduce suffering in all its forms, improving the quality of life for everyone involved in the journey and ensuring that no one feels alone [2]”.
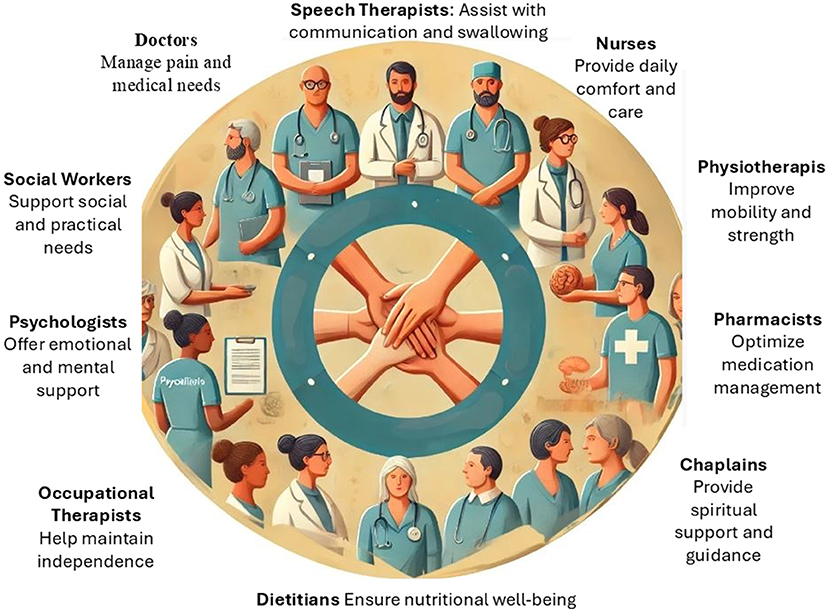
- Figure 2 - The many professionals in the interdisciplinary palliative care team each have a critical role in supporting the patient and the patient’s family.
- From managing physical symptoms to providing emotional, social, and spiritual support, this team approach ensures broad and compassionate care at every stage of a serious illness.
Evolution of Palliative Care
Next, you ask Linda about the origins of palliative care. She smiles, eager to share the story. “The concept of palliative care has its roots in the development of hospices”, Linda begins, explaining that hospices are special places where people with serious illnesses can go to receive care, comfort, and support when they are nearing the end of their lives. “Hospices are not scary”, Linda says gently. “Instead, they are places full of warmth and kindness, where families can spend meaningful time together. The focus is on making sure every moment is as peaceful and comfortable as possible”. She pauses for a moment before continuing, “But did you know hospices are also part of something bigger called palliative care? That means helping people feel better physically, emotionally, and even spiritually, no matter where they are—at home, in the hospital, or here in a hospice. It is not just about curing; it is about caring”. “In the 1960s, a British nurse named Dame Cicely Saunders was moved by the lack of compassionate care for people at the end of life. She believed everyone deserves to pass their final days with dignity and comfort, so she opened the first modern hospice, St. Christopher’s Hospice, in London”. Linda explains that Saunders’ vision was revolutionary because it introduced the idea of holistic care, where the focus was not solely on treating symptoms but on caring for the whole person. “She saw how important it was to address emotional, social, and spiritual needs, not just physical pain”, Linda adds. “This approach laid the foundation for what we now know as palliative care”.
Who is Palliative Care For?
Still curious, you ask Linda, “How popular is palliative care and who uses it?” Linda explains, “Palliative care is becoming increasingly well-known worldwide. More and more hospitals and clinics now offer this type of care as part of standard treatment because people recognize how much it can improve quality of life from the moment of diagnosis of a serious illness”. You reflect on how important it is for more people to know about this type of care, so they can receive the support they need when facing a severe illness. Linda continues, “As for the patients who need palliative care, we work with people of all ages facing serious health conditions. This includes individuals with cancer, chronic heart and lung diseases, neurological conditions like Parkinson’s and Alzheimer’s, and even certain severe childhood illnesses. Each patient’s needs are unique, and so is the care they receive”.
“Timelines also differ depending on the patient’s condition and personal journey. By starting to treat people with serious illnesses before they reach the end of life, we can manage their symptoms and improve their quality of life from an early stage”. Intrigued, you ask Linda, “Do only patients with no hope of a cure receive palliative care, or can someone with a slim chance of being cured also enter palliative care?” Linda clarifies, “Palliative care is not limited to those without hope of a cure. Even patients with a small chance of recovery can receive palliative care to manage symptoms and improve their quality of life. It is about providing support whenever there is a serious illness, regardless of the outlook”.
Next, you ask, “Do we currently have enough resources in palliative care? I imagine more patients are entering palliative care these days because people live longer”. Linda sighs, “That is a big challenge. You are right—aging populations and advances in disease management mean more people need palliative care than 30 years ago. Unfortunately, resources have not kept up with this demand in many places. There is always a need for more trained professionals, facilities, and funding to ensure that everyone who needs palliative care can access it”.
General Principles of Palliative Care
To learn even more, you ask Linda about the general principles of palliative care. Linda explains, “Several fundamental principles guide our work. First, we aim to relieve pain and other distressing symptoms, such as extreme weakness, loss of appetite, difficulty breathing, and other severe emergencies that may arise [3]”. She continues, “We firmly believe life and death are natural processes. We are not here to hasten or delay death but to help the patient live with the best possible quality of life for the time they have”.
“What about family support?” you ask. “We offer a robust support system to help the family cope with the patient’s illness”, says Linda. “We understand that the illness affects the whole family, not just the patient. We provide emotional, practical, and legal support to help families navigate this difficult period”. She continues, “We also help patients live as actively as possible until the end. We want them to maintain their dignity and enjoy life to the fullest within their possibilities”.
“Does the palliative care team help the relatives after a patient has passed away?” you ask. Linda nods, “Absolutely. Supporting the family is a central part of palliative care. Our team offers grief counseling and emotional support to help relatives cope with their loss. We understand that the family’s journey does not end when the patient passes, and we are here to help them find comfort during such a challenging time”.
Effectiveness and Challenges
“But how successful is palliative care?” you ask. Linda says, “It is very effective! Palliative care helps manage symptoms like pain, anxiety, and depression, providing both physical and emotional relief. Studies show that palliative care improves wellbeing and can extend a patient’s life by reducing unnecessary hospitalizations and focusing on comfort”.
“Are there any problems the health team faces during this process?” you ask. Linda thinks for a moment and replies, “Yes, there are. Working with patients in the advanced stages of life can be emotionally exhausting for healthcare professionals. Many doctors and nurses experience emotional burnout because forming close connections with patients and their families can be challenging when they are dealing with the reality of death. There are also practical challenges, such as managing complex symptoms and coordinating care among various specialists. And sometimes, handling patients’ and families’ expectations is complicated, especially when cultural or personal beliefs influence care decisions”.
You reflect on everything Linda has shared and feel a new admiration for the work she and her team do. “This shows how compassionate and kind palliative care is”, you comment. Linda smiles and agrees. “Yes, our goal is to care for people completely, providing comfort, dignity, and support, no matter how difficult the journey. I hope this inspires you to see the importance of caring for each other in all moments of life”.
After your discussion with Linda, you realize that palliative care represents a deep commitment to human dignity, providing relief, comfort, and holistic support to patients and their families during critical moments of a severe illness. More than a set of medical treatments, palliative care includes emotional, social, and spiritual aspects, reaffirming life while naturalizing the dying process. With an interdisciplinary approach and a focus on overall wellbeing, palliative care ensures that no one faces suffering alone, helping people to live quality lives until the very last moment.
Glossary
Palliative Care: ↑ Healthcare focused on comfort and support for individuals with serious illnesses, addressing physical, emotional, social, and spiritual needs.
Quality of Life: ↑ The overall wellbeing and comfort of a person, encompassing physical, emotional, social, and spiritual aspects.
Interdisciplinary: ↑ Describes a group (in this case, of healthcare professionals) from various specialties working together to provide broad care to patients and their families.
Hospices: ↑ Facilities providing care and support for individuals in the final stages of life, emphasizing dignity, comfort, and quality of life.
Holistic Care: ↑ Care that goes beyond simply treating symptoms, to consider the physical, emotional, social, and spiritual wellbeing of the patient.
Grief Counseling: ↑ Emotional support to help individuals cope with loss, process grief, and find resilience after the death of a loved one.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Schlick, C. J. R., and Bentrem, D. J. 2019. Timing of palliative care: when to call for a palliative care consult. J. Surg. Oncol. 120:30–4. doi: 10.1002/jso.25499
[2] ↑ Sekse, R. J. T., Hunskår, I., and Ellingsen, S. 2018. The nurse’s role in palliative care: a qualitative meta-synthesis. J. Clini. Nurs. 27:e21–e38. doi: 10.1111/jocn.13912
[3] ↑ Ryan, S., Wong, J., Chow, R., and Zimmermann, C. 2020. Evolving definitions of palliative care: upstream migration or confusion? Curr. Treat. Options Oncol. 21:20. doi: 10.1007/s11864-020-0716-4
