Abstract
Alzheimer’s and Parkinson’s are the two most common diseases that affect people’s brains and nerves worldwide. You might have a family member, friend, or neighbor who received one of these diagnoses and may have seen how the disease has made their life more challenging. The diseases are different from each other. Alzheimer’s primarily causes loss of memory and thinking skills, while Parkinson’s decreases control over body movements. However, they share two unexpected similarities. First, they begin with the death of brain cells in tiny, specialized brain regions that produce chemicals that help coordinate thoughts and behaviors. Second, in both brain regions, the damage to these cells begins many years before people show any disease symptoms—even 20 years earlier or more! For scientists working to detect and prevent brain diseases and communities trying to keep themselves healthy, it is critical to understand how these brain regions change in disease.
Neurodegenerative Diseases Start in Two Special Brain Regions
Alzheimer’s and Parkinson’s are two common diseases that cause brain cells, called neurons, to die. You may know an adult, like a family member, friend, or neighbor, who is living with one of these diseases and has trouble because of their symptoms. Alzheimer’s is a disease that causes serious memory loss, while Parkinson’s makes it harder to control movements. Although Alzheimer’s and Parkinson’s eventually affect many brain systems, they begin with changes in the health of two important brain regions: the locus coeruleus and substantia nigra. Changes can occur in these two brain regions even up to 20 years before disease symptoms appear. The regions are similar in size, and they undergo similar changes during disease.
The locus coeruleus is found in the bottom part of the brain (called the brain stem), and it consists of roughly 60,000 neurons. The substantia nigra consists of 400,000 neurons and is found in the middle of the brain, in an area called the basal ganglia. This may sound like a lot of neurons, but these regions are tiny compared to other brain regions—<0.00001% of the neurons in the brain are found in these regions. The locus coeruleus and substantia nigra exist in both the left and right hemispheres (halves) of the brain.
A Colorful Brain Chemical Found Only in the Locus Coeruleus and Substantia Nigra
The similarities between these two regions continue with their unique names. In Latin, “locus coeruleus” means “blue spot” and “substantia nigra” means “black stuff”. These brain regions have colorful names because they both contain a dark-colored chemical called neuromelanin. Neuromelanin is very similar to the pigment that gives skin and hair its color. One region looks black and the other blue simply due to differences in neuromelanin concentration. Neuromelanin is only present in the locus coeruleus and substantia nigra. The rest of the brain looks gray or white. Researchers can find the locus coeruleus and substantia nigra in living people using special kinds of brain imaging called magnetic resonance imaging (MRI) [1] (Figures 1A–C).
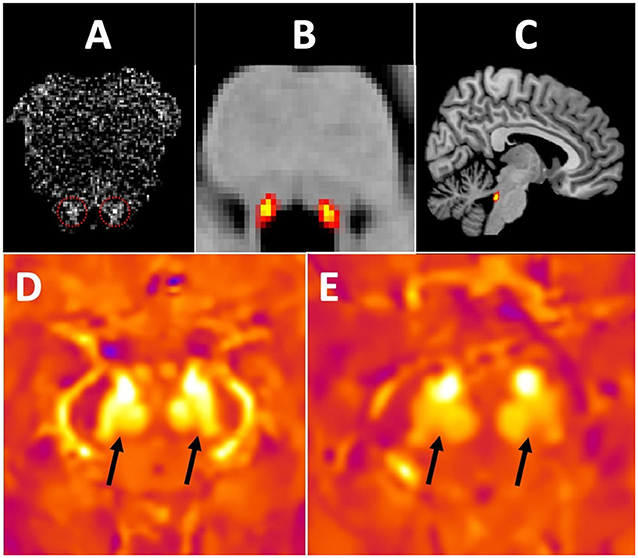
- Figure 1 - (A) This horizontal slice through the brain stem detects neuromelanin in the locus coeruleus (LC; arrows).
- (B) We made a map showing where the LC usually is (yellow and red), based on MRI scans of about 100 people. (C) This is the same map of the LC from looking at the brain from the side. (D) This horizontal image of the brain stem of a Parkinson’s disease patient measures iron in the brain. When cells die in the substantia nigra (SN), toxic iron is released and produces a brighter yellow signal (E). In a healthy person, these areas are dimmer, meaning neurons are still alive and have not released their iron.
Neuromelanin is not just colorful, and it does more than allow researchers to find the locus coeruleus and substantia nigra in MRI pictures: it changes the risk of disease. Neuromelanin plays both a protective and damaging role in brain health. Neuromelanin may be protective in younger people because, like a sponge, it can soak up toxins (dangerous substances) that can damage the brain. However, if the neuromelanin in these brain regions soaks up more toxins than it can hold, or if it gets damaged, it can release toxins like iron back into the brain [2] (Figures 1D, E). When, how, and why neuromelanin becomes more harmful than helpful are questions that still need answers. These answers could tell us how the choices we make when we are young influence our brain health in middle age and later life.
The Locus Coeruleus and Substantia Nigra Play Special Roles in Human Brain Health
The locus coeruleus is found in all vertebrates, meaning all animals with backbones—from fish to humans. The substantia nigra is not found in all vertebrates, but it is present in most. The roles that these brain regions play in brain health, however, is special to humans. For example, other animals do not have neuromelanin. Also, humans are the only animals (or one of a very small group) that naturally develop neurodegenerative diseases. This tells us that something about how the locus coeruleus and substantia nigra work in humans is different from other animals. Researchers are trying to discover why these brain regions are susceptible to damage and how the ways humans use their brains might increase or decrease the risk of neurodegeneration [3].
One special role the locus coeruleus and substantia nigra play is producing chemicals, called neuromodulators, that help control mood, movement, and alertness. These chemicals are important for how we feel, move, and pay attention (Figure 2A). Neuromodulators alter neuron activity levels and change the flow of information in the brain, to help us perform various tasks. Neuromodulators help in all the complex behaviors people do, such as giving directions, responding to a medical emergency, or playing a chess game. In Alzheimer’s and Parkinson’s diseases, there are locus coeruleus and substantia nigra changes in the production and release of neuromodulators very early in the diseases. The changes to the neuromodulators often cause people to have trouble doing or thinking what they want, walking safely, or paying attention, because these behaviors are normally supported by healthy neuromodulators.
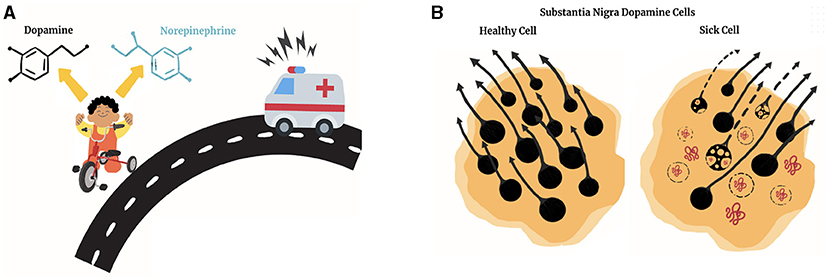
- Figure 2 - (A) Brain chemicals from the substantia nigra (SN) and locus coeruleus (LC) work together during tasks like riding a bike.
- Dopamine provides feedback that helps you pedal correctly or correct yourself after a mistake. Norepinephrine helps you pay attention to what is important, like a siren. (B) Healthy SN cells are rich in neuromelanin and produce neuromodulators efficiently. In Alzheimer’s and Parkinson’s, cells accumulate toxins that cause cell death and impair function. These cells lose neuromelanin and produce less dopamine and norepinephrine, leading to symptoms like difficulty moving, concentrating, sleeping, etc., (figure designed by Annalee J. Pratt).
What Happens When the Locus Coeruleus Gets Sick?
The locus coeruleus is the brain’s primary producer of a substance called norepinephrine. Norepinephrine increases alertness, engagement, anxiety, and physical performance. It helps us deal with immediate challenges or dangers. Norepinephrine influences behavior by traveling from the locus coeruleus to other brain regions and affecting information processing there. Having the right level of norepinephrine in the brain at the right time (not too much or too little for what you are trying to do) is important to your health [4].
The behaviors and mental actions associated with norepinephrine, like alertness and anxiety, are part of the Alzheimer’s disease process. However, what happens in Alzheimer’s is more than a lack of norepinephrine. The early phase of the disease may be characterized by increased norepinephrine release, causing anxiety and agitation and affecting sleep cycles. In the later phases of the disease, cell death in the locus coeruleus significantly reduces norepinephrine release, leading to inattention and tiredness. By the time an Alzheimer’s diagnosis is made, many locus coeruleus neurons are typically already dead. One of our major research goals is identifying these sneaky changes occurring in the locus coeruleus before cells die in other places in the brain.
What Happens When the Substantia Nigra Gets Sick?
In contrast to the locus coeruleus’s role as the primary producer of norepinephrine, the substantia nigra is one of several brain regions that produce its neuromodulator, dopamine. You may have heard of dopamine because it plays an important role in rewarding activities like playing video games, eating delicious foods, or spending time with friends. However, dopamine is also produced when an adverse event occurs (like making a mistake on a test), or when the body moves, or when you are learning something new.
In Parkinson’s disease, the locus coeruleus norepinephrine cells begin to die, just like in Alzheimer’s disease, years before the substantia nigra cells. Then the dopamine-producing cells in the substantia nigra begin to die. Researchers know that loss of dopamine due to cell death in the substantia nigra causes Parkinson’s symptoms. Surprisingly, it takes the loss of 80% of the dopamine-producing cells in the substantia nigra before the usual movement difficulties associated with Parkinson’s appear (Figure 2B). This means the Parkinson’s disease process begins many years before symptoms begin, just like the Alzheimer’s disease process.
If that sounds scary, it is! But importantly, research has uncovered a lot of information about the “gunk” that may cause cell death in the locus coeruleus and substantia nigra. Scientists use this information and keep discovering more, so we can take action before the brain is seriously damaged. We may also be able to use this kind of information to keep ourselves healthier.
Keeping the Locus Coeruleus and Substantia Nigra Safe From Brain Gunk
The primary suspect for starting the cell death in the locus coeruleus and substantia nigra is brain gunk. In Alzheimer’s, gunk made from the protein beta-amyloid accumulates in the brain. A certain amount of amyloid gunk triggers a second type of gunk, called hyperphosphorylated tau, which leads to cell death starting in the locus coeruleus. In Parkinson’s, the gunk is made from the protein alpha-synuclein, which, in clumping together, causes cell death. Scientists are still unsure about what makes these regions susceptible to damage from these different types of brain gunk.
When locus coeruleus or substantia nigra neurons detect that gunk is building up, they may get stressed. Stressed neurons can have lots of problems. They might release neuromelanin, dumping the toxins it holds to create even more problems. Recently, important experiments have tried to measure gunk with brain scans or blood tests, or to stop these types of gunk before they lead to cell death [5]. Safeguarding these brain regions is not only the work of professional researchers but also something you can start thinking about to help keep yourself healthy. While everyone has a different physical makeup, health history, and environment, there are powerful and straightforward actions you can take to help keep your locus coeruleus and substantia nigra healthy (Figure 3).
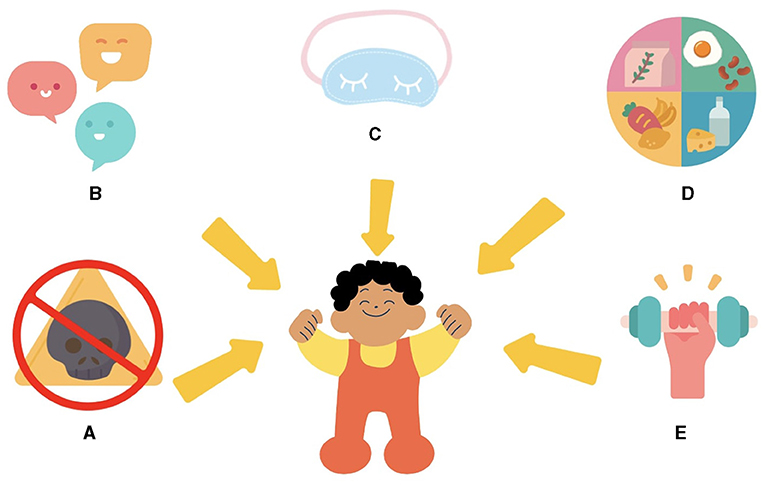
- Figure 3 - The actions and behaviors shown in this figure can specifically protect the health of the locus coeruleus and substantia nigra, by limiting the build-up of brain gunk and neurodegeneration.
- These behaviors also reduce a person’s overall risk for other conditions, like diabetes or heart disease, and support a healthy brain, brain-body communication, and overall well-being. (A) Toxins and pesticides can cause degeneration. (B) Social engagement supports brain health. (C) Sleep clears the “gunk” that accumulates in your brain. (D) Good nutrition and a healthy diet safeguard the brain. (E) Exercise reduces disease likelihood and symptoms (figure designed by Annalee J. Pratt).
In conclusion, Alzheimer’s and Parkinson’s diseases can be bewildering. However, probing their earliest beginnings can help us understand why they occur and how we might protect ourselves. The locus coeruleus and substantia nigra, these tiny, colorful, influential, and protectable brain regions, play a significant role in the story of neurodegeneration.
Glossary
Neuromelanin: ↑ A pigment like the kind that gives color to hair or skin, but in your brain.
Magnetic Resonance Imaging: ↑ A way of imaging the inside of the body for research and diagnosis. MRI uses magnets and radio waves to take images non-invasively, so it is safe for long-term exposure.
Neurodegeneration: ↑ The slow, continuous death of brain cells (neurons) over time. Different diseases like Alzheimer’s and Parkinson’s cause death in different brain areas, which causes different symptoms.
Neuromodulators: ↑ Chemicals such as dopamine and norepinephrine that change the way the brain responds to events and information, influencing our feelings, thoughts, and actions.
Beta-Amyloid: ↑ Gunk that clumps up in the brains of people with Alzheimer’s disease. These clumps cause cell death (neurodegeneration).
Hyperphosphorylated Tau: ↑ A protein (tau) that has been abnormally modified (hyperphosphorylated, meaning too many phosphate groups have been added) such that it clumps up. This happens in several different neurodegenerative diseases and causes cell death (neurodegeneration).
Alpha-Synuclein: ↑ Gunk that clumps up in the brains of individuals with Parkinson’s disease and other related diseases, causing cell death (neurodegeneration).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by the National Institutes of Health through the F32 AG058479 to ER and R01 AG066430 to the lab.
References
[1] ↑ Bae, Y. J., Kim, J. M., Sohn, C. H., Choi, J. H., Choi, B. S., Song, Y. S., et al. 2021. Imaging the substantia nigra in Parkinson disease and other parkinsonian syndromes. Radiology 300:260–78. doi: 10.1148/radiol.2021203341
[2] ↑ Iannitelli, A. F., and Weinshenker, D. 2023. Riddles in the dark: decoding the relationship between neuromelanin and neurodegeneration in locus coeruleus neurons. Neurosci. Biobehav. Rev. 152:105287. doi: 10.1016/j.neubiorev.2023.105287
[3] ↑ Matchett, B. J., Grinberg, L. T., Theofilas, P., and Murray, M. E. 2021. The mechanistic link between selective vulnerability of the locus coeruleus and neurodegeneration in Alzheimer’s disease. Acta Neuropathol. 141:631–50. doi: 10.1007/s00401-020-02248-1
[4] ↑ Sara, S. J., and Bouret, S. 2012. Orienting and reorienting: the locus coeruleus mediates cognition through arousal. Neuron 76:130–41. doi: 10.1016/j.neuron.2012.09.011
[5] ↑ Siderowf, A., Concha-Marambio, L., Lafontant, D. E., Farris, C. M., Ma, Y., Urenia, P. A., et al. 2023. Assessment of heterogeneity among participants in the Parkinson’s Progression Markers Initiative cohort using α-synuclein seed amplification: a cross-sectional study. Lancet Neurol. 22:407–17. doi: 10.1016/S1474-4422(23)00109-6
