Abstract
A significant proportion of our aging society suffers from Alzheimer’s disease (AD). AD is a disorder that changes the brain tissue and slowly destroys several important parts of the brain responsible for memory, thinking, and communication skills. Over time, patients’ forgetfulness increases, and they need more care to carry out even the simplest tasks—such as eating, drinking, or self-hygiene. This can create extremely challenging living conditions for their families. Many children witness how their beloved grandparents or other elderly relatives change, forget things, and eventually do not recognize them or confuse them with their parents. Watching family members progress through the stages of Alzheimer’s disease can be a challenging, painful, and even frightening experience for young people. The aim of this article is to explain Alzheimer’s disease, its symptoms, and its consequences to help young people understand and cope with this disease if it happens in their families.
What Is Alzheimer’s Disease?
How do you remember the way to get home? How do you know what the word for chair is? How do you know what day it is? Your brain helps you complete all these tasks. It is what allows you to think thoughts, feel emotions, and learn new things. The brain contains billions of specialized cells called neurons that are essential to everything you do. Every time you think a thought or pick up a glass of water, your neurons are communicating with each other.
When someone has a neurodegenerative disease, neurons are damaged and can die. This causes miscommunication between neurons, which affects how the brain works. Alzheimer’s disease (AD) is a type of neurodegenerative disease [1]. AD is a permanent disease that gradually gets worse over time. One of the first signs of AD is difficulty remembering recent conversations, activities, or events. People may struggle to complete familiar tasks, like turning on the TV, getting dressed, or making a meal. They may get lost easily, forget where they live, or have trouble understanding new information. They may also have changes in mood and behavior, such as becoming anxious or suspicious [2].
AD typically affects people ages 65 or older. Unlike the flu or a cold, AD is not contagious. It is caused by changes in the brain that are still not completely understood by scientists. Around five million people in the USA have AD [3].
There is currently no cure for AD, although there are treatments that can slow down the effects of the disease [1]. Medicines can treat and manage the symptoms of AD, helping patients live their daily lives. Cholinesterase inhibitors are one type of medicine used to treat AD [4]. People with AD tend to have lower amounts of a brain chemical called acetylcholine. Acetylcholine is a chemical that neurons use to communicate with each other. Cholinesterase inhibitors are used to increase the amount of acetylcholine in the brain, and they can help improve brain function [4].
How Does Alzheimer’s Disease Affect the Brain?
In the brain of people with AD, there is a buildup of a toxic substance called beta-amyloid protein, which forms clumps around neurons [1]. These clumps damage nearby neurons and stop them from communicating with each other. People with AD also have a buildup of another toxic substance called tau protein. Unlike beta-amyloid protein, which accumulates around neurons, tau protein accumulates inside the neuron cell body. Clumps of tau protein are called neurofibrillary tangles, and they can cause cell death and prevent neurons from communicating with each other [3].
Certain areas of the brain are more severely affected by AD than others. The hippocampus and temporal lobe are highly affected areas, and these are the brain regions important in memory. The hippocampus is particularly important for storing long-term memories and converting short-term memories into long-term memories, so that you can remember things that happened to you a long time ago [5]. The hippocampus also helps process events, locations, and times [5]. In AD, neurons in the hippocampus are damaged and eventually die [1, 6]. This can prevent the hippocampus from working properly, leading to memory loss [2]. A person with AD might not be able to recognize family members or might call a family member the wrong name. The person also might not be able to remember where they are or how they got there.
AD can also affect a part of the brain called the amygdala, which is involved in emotions and emotional reactions [6, 5]. Damage to the amygdala in AD is associated with personality changes, mood changes, anxiety, and irritability [7]. A brain area called the frontal lobe can also be damaged in AD, which can lead to difficulty with planning, multitasking, or decision making [7, 8]. Some people may also have trouble with tasks that must be done in a certain order, like cooking [7]. Some AD symptoms are more common than others, but AD can affect people in different ways. Two people with AD might have completely different symptoms.
What Causes Alzheimer’s Disease?
There is not one thing that causes AD—there are many things that affect whether or not a person gets it [1]. Things that increase the chances that a person will develop a disease like AD are called risk factors (Figure 1). The most significant risk factor for AD is age: the majority of AD cases are in people who are 65 years old or older, and the likelihood of developing AD almost doubles every 5 years past the age of 65 [3]. That means that someone who is 70 years old is almost twice as likely to get AD as someone who is 65 years old, and someone who is 75 is almost four times as likely to develop AD than someone who is 65 years old.
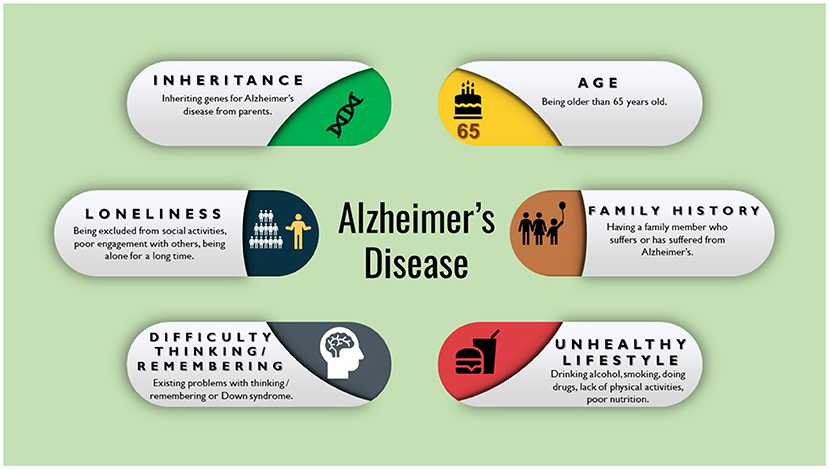
- Figure 1 - Things that can increase a person’s chances of getting a disease like AD are called risk factors.
- The more risk factors a person has, the more likely the person is to get AD. It is important to note that having these risk factors does not necessarily mean a person will develop AD. Rather, risk factors increase the chances of developing the disease.
Genetic mutations—certain changes in a person’s DNA—are another risk factor for AD [1]. Many mutations have been found to be associated with developing AD, but the genetics of AD are complex and are not yet fully understood. Because mutations can be inherited, this also means that a person who has a family member with AD might be more likely to develop AD in the future. But just because a person has AD does not guarantee that their relatives will develop the disease. Other factors such as diet and medical conditions are also important risk factors for developing AD [1].
What if You Know Someone With Alzheimer’s Disease?
If someone you love has Alzheimer’s disease, it may be difficult sometimes. The person may not remember events, might call you by the wrong name, or might show personality changes. Your relationship with this person might change as well. It can help to remind yourself that your loved one with AD is still the same person they have always been, even though they may have trouble remembering things or thinking clearly. The person still has feelings, can still enjoy life, and can still experience pain if they are neglected or mistreated. It is important to treat people with AD like any other human being—they deserve to be treated with respect, kindness, and compassion. Even if you feel uncomfortable, weird, sad, nervous, embarrassed, or confused around this person, you can still treat them well. You might feel all—or none—of these things, and that is totally normal.
How Can You Support Someone With AD?
If someone you love has AD, it is important to know that they still care about you. The disease is changing their brain in ways that they cannot control, and that also changes the way that they act. AD is not anyone’s fault. There are several ways that you can support a loved with AD (Figure 2):
- Love is healing and takes away the pain. Love has a special power that can make things better. If someone in your family has AD, they may have trouble remembering people’s faces, names, or where they are. But you should know that, deep down, the person still loves you just like they always have. When you show the person love and care, it brings them lots of joy and happiness.
- Educate yourself about AD. This knowledge will help you understand what to expect and how to best support your loved one. You can read books or watch documentaries about AD. You can also talk to your family and other people you trust about AD and how it makes you feel.
- Be mindful of how you communicate with a loved one with AD. Talking with a person with AD can be challenging. However, it is very important to be patient, use simple language, repeat what you said when needed, and avoid arguments or confrontations.
- Talk about pleasant past experiences with your loved one with AD. It can help to reminisce about positive things, for example by looking at old photos. You can ask your loved one about their childhood, siblings, school, or pets. It can be uplifting for the person with AD to connect with their past. You can also encourage them to talk about subjects they are interested in.
- Spend time with your loved one with AD. Spending time together shows that you care about them and that they are important to you. You can do something outside, like go on a walk or plant flowers! You can also watch a movie, read a book together or read aloud to them, play a game, or complete a puzzle.
- Include your loved one in simple family activities such as listening to music or looking at photo albums. People with AD still enjoy these types of activities.
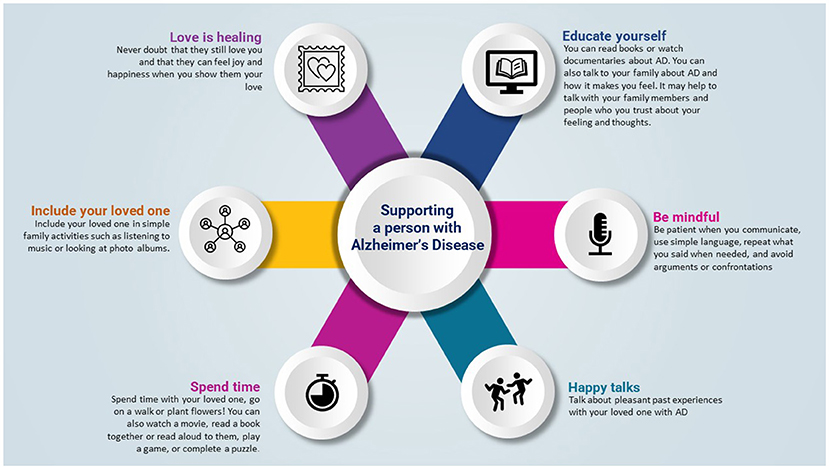
- Figure 2 - There are many ways you can provide support to a loved one with AD.
If you are spending time with someone with AD, try to be patient with them. On some days they might remember more, and other days their symptoms might be worse. The same is true for any of us: we all have good days and bad days. The most important thing any of us can do if we have a family member with AD is to remember to support and take care of one another.
Glossary
Neuron: ↑ A neuron is a special brain cell that acts like a tiny messenger in your brain. It sends messages to other parts of your body, helping you think, move, and feel things.
Neurodegenerative Disease: ↑ A disease that causes brain cells to die and damages the brain.
Cholinesterase Inhibitor: ↑ A medicine that helps to keep the neuron-communication molecule acetylcholine around a bit longer, to keep messages in the brain flowing smoothly.
Acetylcholine: ↑ A messenger molecule in the brain, sent between neurons as a form of communication.
Beta-Amyloid Protein: ↑ A protein that forms toxic clumps around brain neurons.
Tau Protein: ↑ A protein that accumulates inside of neurons, forming toxic clumps called neurofibrillary tangles.
Neurofibrillary Tangles: ↑ Clumps of twisted protein fibers that build up inside nerve cells in the brain and disrupt normal brain function.
Genetic Mutation: ↑ A change in the DNA sequence of a gene that can be good, do nothing, or be harmful.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Breijyeh, Z., and Karaman, R. 2020. Comprehensive review on Alzheimer’s disease: causes and treatment. Molecules 25:5789. doi: 10.3390/molecules25245789
[2] ↑ López, O. L., and DeKosky, S. T. 2008. Clinical symptoms in Alzheimer’s disease. Handb. Clin. Neurol. 89:207–16. doi: 10.1016/S0072-9752(07)01219-5
[3] ↑ Korolev, I. O. 2014. Alzheimer’s disease: a clinical and basic science review. Med. Stud. Res. J. 4:24–33.
[4] ↑ Knafo, S. 2012. “Chapter 15, Amygdala in Alzheimer’s Disease,” in The Amygdala - A Discrete Multitasking Manager (London: IntechOpen Limited).
[5] ↑ Martin, J. H. 2021. Neuroanatomy: Text and Atlas. 5th Edn. New York, NY: McGraw Hill.
[6] ↑ Planche, V., Manjon, J. V., Mansencal, B., Lanuza, E., Tourdias, T., Catheline, G., et al. 2022. Structural progression of Alzheimer’s disease over decades: the MRI staging scheme. Brain Commun. 4. doi: 10.1093/braincomms/fcac109
[7] ↑ Jones, D. T., and Graff-Radford, J. 2021. Executive dysfunction and the prefrontal cortex. Behav. Neurol. Psychiatry 27:1586–601. doi: 10.1212/CON.0000000000001009
[8] ↑ Swanberg, M. M., Tractenberg, R. E., Mohs, R., Thal, L. J., and Cummings, J. L. 2004. Executive dysfunction in Alzheimer disease. Arch. Neurol. 61:556–60. doi: 10.1001/archneur.61.4.556
