Abstract
Serious bleeding, known as major hemorrhage, is the most common cause of death in people with serious injuries. People with major hemorrhage often have a lower amount of an important protein called fibrinogen in their blood, which makes it more difficult to stop the bleeding. In a big randomized controlled trial called CRYOSTAT 2, we looked at whether giving people extra fibrinogen soon after their injury helped stop bleeding and increased the number of people who survived. We were surprised to find that fibrinogen did not help as much as we expected, and that it may even make some people more likely to die. In this article, we talk about the CRYOSTAT-2 experiment and how it shows we cannot treat all bleeding patients in the same way.
What Does the Blood Do?
Blood carries the food and oxygen that the body needs to work normally. Blood moves through our bodies in tubes called blood vessels, taking food and oxygen to where they are needed. If the blood vessels are damaged, the blood inside leaks out and this is called bleeding.
Most bleeding is minor and is stopped by components of the blood itself. Small cells in the blood called platelets stick to damaged parts of the blood vessel and to each other, making a plug called a blood clot that blocks the hole to stop the leak. This plug can easily be washed away or broken apart, so the platelets send messages to other cells and proteins in the blood to make the clot stronger.
Fibrinogen is one of the main proteins that helps make blood clots stronger, and this protein travels in the blood all the time. When there is bleeding, the body turns fibrinogen into stringy fibers called fibrin, which are knitted around the platelets to hold them in place. At the same time, the body starts to break down some of the fibrinogen fibers, so the clot does not get too big. This happens to keep the balance—so the clot that forms is big enough to plug the hole, but not too big that it blocks blood vessels (Figure 1).
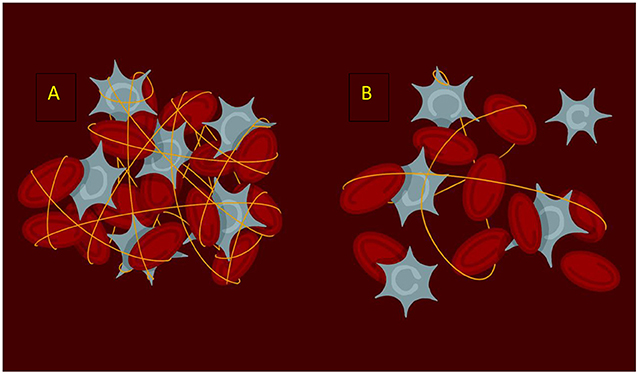
- Figure 1 - (A) A normal blood clot in which the platelets (gray) are knitted together by fibrin (yellow strands) to make a strong clot that stays in place.
- (B) A blood clot in someone with TIC. There is less fibrin to knit the platelets together, leaving a fragile clot that is easily washed away.
Serious Injuries Can Cause The Blood To Stop Clotting
More serious injuries, sometimes called major trauma [1], are divided into two groups: blunt and penetrating. Blunt injuries, such as a fall, being hit with an object, or being hit by a car, usually cause bleeding inside the body. Penetrating injuries, like being stabbed or cut, are when something breaks the skin and we see blood come out. If the bleeding from blunt or penetrating injuries causes so much blood to leak out that the body cannot get enough food or oxygen to work properly, it is called major hemorrhage. Around four in 10 people with major hemorrhage develop a condition called trauma-induced coagulopathy (TIC) [2]. People with TIC have problems with a lot of their blood clotting proteins because of their injuries. The systems that cause blood clots to break down are more active in these injured people than the systems that help blood to clot. People with TIC bleed more and are more likely to die than people without it. Research has found that the amount of fibrinogen in the blood of people with TIC is much lower than normal [3].
Does Giving People Fibrinogen Stop Their Bleeding?
Some studies have shown giving fibrinogen to people who are bleeding can help their blood to clot and improve their survival. An experiment called the CRYOSTAT 2 Trial was developed to see if giving people extra fibrinogen very soon after their injuries, when they arrived in the Emergency Department, would help stop their bleeding and increase the number of people who survived. Testing for fibrinogen with the most common test takes around an hour, which is too slow in an emergency, so in this study the treatment was given without knowing whether people had low fibrinogen levels or not.
Doing research like this is very difficult, as the people we study are very sick and must meet strict rules to be included in the experiment. In this study, people with a major hemorrhage who needed blood transfusions and got to the hospital within 3 h of injury could be included. As these patients were very sick, we could not ask them if they wanted to take part, so researchers had special permission to include them without consent. This is allowed in emergency research, when researchers cannot carry out the research another way, as long as the researchers ask for permission later on. In our study, only 50 people out of 1,604 did not want to take part when they were asked!
If someone met the rules to be included, the researchers opened an envelope that told them whether they should give the normal treatment for bleeding (called standard care) or the new treatment (early fibrinogen). A computer had randomly decided which treatment went in which envelope before the trial started, and there was no way for anyone to know what was inside. This is called a randomized controlled trial. Once the treatment had been decided by opening the envelope, the researchers and medical team knew whether the patient had received the new treatment or not. The patients were not aware of the study when they received treatment (because they were so sick) but could ask about the study later.
Based on other studies, if the treatment worked, we thought the number of deaths would be 7% lower in the group that was given extra fibrinogen compared to the standard care group [4]. We used this estimate, along with some statistics and an estimate of the number of people who might decide they did not want to take part, to decide how many people we should include in the study. We ultimately included 1,604 patients who were treated in hospitals across the UK and America (Table 1).
| Early fibrinogen | Standard care | |
|---|---|---|
| Number of people | 799 | 805 |
| Age (median) | 38 | 40 |
| Male (%) | 79 | 80 |
| Blunt injury (%) | 63 | 65 |
| Penetrating injury (%) | 37 | 35 |
| Time from injury to arrival in hospital (minutes) | 75 | 77 |
- Table 1 - Make-up of the study, including the early fibrinogen group and the standard care group.
What Did The Experiment Find?
Overall, there was very little difference in what happened to the patients in either group, with around one quarter of the patients dying of their injuries in both groups. When the type of injury was compared, there were some important differences: people who had blunt injuries seemed to benefit from early fibrinogen, but people with penetrating ones were more likely to die if they received fibrinogen (Figure 2). The time the fibrinogen was given may also be important. Patients who got fibrinogen earlier seemed to do worse than those who got it later, but the difference was not big enough to be statistically significant. This might mean there was not a true difference, or it might mean there were not enough people in each time group to show a difference that really exists—but we cannot know for sure without more research.
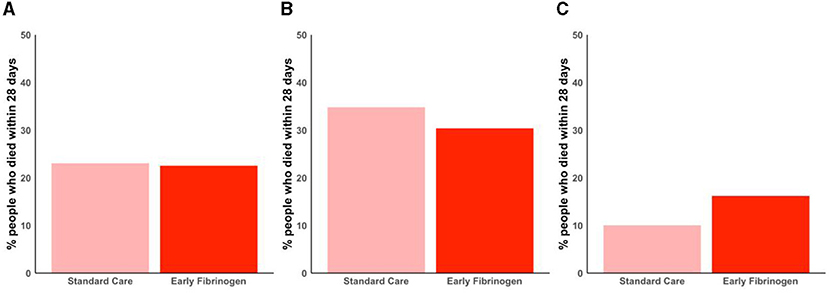
- Figure 2 - The percentage of people who died within 28 days of their injuries, in groups who were given the normal treatment for bleeding (standard care) compared to those who had early fibrinogen added to their treatments.
- Graphs show result for (A) everyone in the study, (B) people with blunt injuries, and (C) people with penetrating injuries. Early treatment may help people with blunt injuries but people with penetrating injuries were worse off.
Why Might Fibrinogen Treatment Not Work?
We did not measure how much fibrinogen people had before they received the treatment. It may be that the patients who did not benefit from early fibrinogen had normal fibrinogen levels and the treatment either made no difference or caused harm such as organ failure, and in patients with low fibrinogen levels, the fibrinogen was not given at the right time or in the right amount.
What We Learnt About Helping People’s Blood To Clot
In summary, this study found that giving extra fibrinogen to everyone with major hemorrhage does not help stop them from dying and, in some cases, it may cause harm. Further research is needed to understand who should get fibrinogen treatment and when, so doctors can make sure the treatment is given to people who need it and not those who could be harmed by it.
Glossary
Platelets: ↑ Fragments of large cells found in the blood which have an important job in making blood clots.
Fibrinogen: ↑ A naturally occurring substance dissolved in the blood. When somebody bleeds, fibrinogen is converted into fibrin.
Fibrin: ↑ A string like substance which strengthens blood clots.
Major Trauma: ↑ Serious and often multiple injuries which are likely to cause death or disability.
Major Hemorrhage: ↑ Serious bleeding in which a person may lose half their blood in less than 3 h.
Trauma-Induced Coagulopathy (TIC): ↑ A blood clotting problem that happens in seriously injured people that makes it difficult to stop them from bleeding.
Randomized Controlled Trial (RCT): ↑ The fairest kind of experiment, in which two conditions are compared. With the people receiving a new treatment chosen at random.
Conflict of Interest
RD reported receiving grants from Barts Charity and UK National Institute for Health and Care Research: Health Technology Assessment during the conduct of the study and personal fees from Octapharma, personal fees and nonfinancial support from Werfen, and grants from HemoSonics outside the submitted work.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Original Source Article
↑Davenport, R., Curry, N., Fox, E. E., Thomas, H., Lucas, J., Evans, A., et al. 2023. Early and empirical high-dose cryoprecipitate for hemorrhage after traumatic injury: the CRYOSTAT-2 randomized clinical trial. JAMA 330:1882–91. doi: 10.1001/jama.2023.21019
References
[1] ↑ NICE guideline [NG24] 2015. Available online at: https://www.nice.org.uk/guidance/ng24/chapter/recommendations#:~:text=Major%20haemorrhage,-This%20can%20be&text=A%20loss%20of%2050%25%20of,beats%20per%20minute%20in%20adults
[2] ↑ Moore, E. E., Moore, H. B., Kornblith, L. Z. Neal, M. D., Hoffman, M., Mutch, N. J., et al. 2021. Trauma-induced coagulopathy. Nat. Rev. Dis. Primers 7:30. doi: 10.1038/s41572-021-00264-3
[3] ↑ Rourke, C., Curry, N., Khan, S., Taylor, R., Raza, I., Davenport, R., et al. 2012. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J. Thromb. Haemost. 10:1342–51. doi: 10.1111/j.1538-7836.2012.04752.x
[4] ↑ Curry, N., Rourke, C., Davenport, R., Beer, S., Pankhurst, L., Deary, A., et al. 2015. Early cryoprecipitate for major haemorrhage in trauma: a randomised controlled feasibility trial. Br. J. Anaesth. 115:76–83. doi: 10.1093/bja/aev134