Abstract
How often you poop can reflect your digestive health. Irritable bowel syndrome (IBS) is a very common digestive illness that affects close to one in five people. Symptoms include pain in the abdomen and changes in how often someone poops. Certain behaviors can increase a person’s risk of having IBS, including the foods they eat, the amount of exercise they get, how much sleep they have per night, and how often they go outside. All these behaviors can influence the brain, which tells the digestive tract the rate at which it should work—which then determines how often people poop. In this article, we will introduce IBS and the main behaviors that are known to affect this disorder.
Bowel Movements Reflect Gut Health
Passing a bowel movement, also known as defecation or pooping, is part of daily life for most people. If you pass a bowel movement approximately once a day, you are generally considered to have a healthy digestive system. Unfortunately, many people do not have consistent bowel movements, and this can lead to emotional and physical side effects. One common reason for irregular bowel movements is irritable bowel syndrome (IBS). 15–20% of people in the United States have this long-term illness, and symptoms include pain in the lower abdomen, defecating too often, having trouble going at all, or both [1]. People with IBS also usually see changes in their poop—either it is too soft and watery, like diarrhea, or too hard and rocklike, usually caused by constipation. In IBS, there is nothing physically wrong with the digestive tract, but digestion still does not function like it should. This means IBS generally results from problems with gut function.
What We Know About IBS
While IBS is a very common illness, very little is known about what causes it. Some scientists suggest that the bacteria that live in the intestines, called the gut microbiome, have something to do with it. Others believe IBS may happen because the digestive tract moves food through either too quickly or too slowly. Another potential explanation may be an issue with how the brain sends messages to the nerves of the digestive organs. It may even be that all the nerves inside the intestines are just extra sensitive, which causes the pain and associated bowel movement changes seen in IBS [2]. Scientists also have not figured out a great way to treat IBS. They may suggest changes in the foods people eat, or recommend that people take prescription medicines, vitamins, or probiotics (food or medicines containing gut microbes) [2]. Sometimes these treatments work, and sometimes they do not. That is the challenge with IBS—every person is different in both the symptoms they show and the treatments that work for them.
IBS and Behavior
All these differences in people with IBS have really stumped scientists, but new research suggests that IBS is likely caused by the environments people live in, as well as their behaviors (Figure 1) [3]. This could be as simple as what they do during the workday to what they eat for dinner. Scientists are learning not to underestimate the role of everyday behaviors in overall health, and that includes the health of the digestive tract. When it comes to IBS, there are several behavioral risk factors that may increase a person’s chance of having this condition.
- Figure 1 - Behaviors that may influence how often someone has bowel movements, as well as their chances of having IBS, include sleep habits, exercise frequency, the types of foods they eat, and how much time they spend outside (created with BioRender.com).
What You Eat
What goes in must come out, right? And what you eat is quite important, especially when it comes to the health of your intestines. It is not surprising that certain foods that can upset digestion are also associated with IBS (Figure 2). These foods include dairy products, like milk and cheese, gluten products, such as bread or pasta, and onions, garlic, and beans. Not everyone is bothered by eating these foods, but several studies have found that people with IBS also are sensitive to eating large amounts of these items [1]. Some people have other illnesses that make them unable to have milk or gluten products, but when it comes to IBS, there is a different explanation for why eating too much of certain foods creates digestive issues. These foods can contain specific kinds of carbohydrates called FODMAPs, which cannot be fully digested by the gut. Since digestion does not break FODMAPs down, the microbes in the intestines then eat these carbohydrates, creating gas. All that gas builds up inside the abdomen, which causes a lot of pain and can also cause a person to defecate more [1].
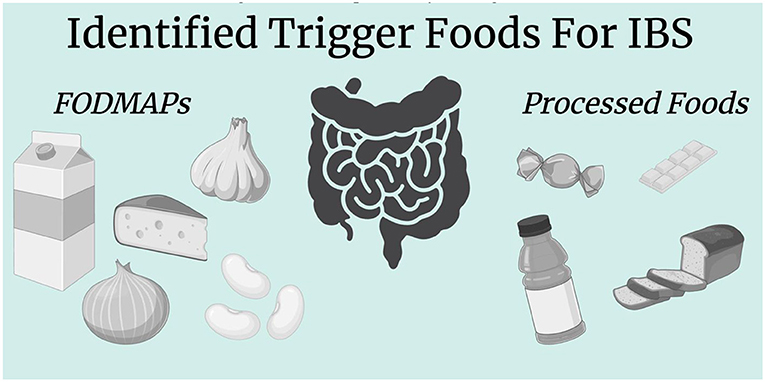
- Figure 2 - Several types of foods may potentially trigger IBS, including certain carbohydrates called FODMAPs, which cannot be digested, and processed (junk) foods, which frequently contain added chemicals and dyes (created with BioRender.com).
Junk foods, like soda, candies, packaged noodles, or chips, can also cause issues with bowel movements. As good as they may taste, they can be bad for digestion! Processed foods can impact how often you defecate and may also cause IBS [3] because they contain added chemicals and food dyes. These chemicals can kill the good bacteria in the gut microbiome, which then worsens overall digestive health, potentially leading to IBS.
How Much You Move
We all know exercise is important to keep us healthy, but did you know it is also important to keep your digestion in working order? Physical activity is another everyday behavior that has an impact on bowel movements. When studying IBS patients, doctors have found that those who move the least have the highest rates of IBS [2, 4]. That means that low levels of exercise (generally under 1 h per week) over long time periods may contribute to IBS. Because of these findings, IBS patients are often prescribed exercise as treatment, like yoga or walking. This seems to be one great way to improve IBS symptoms. Exercise behaviors may cause digestive issues because of the way the brain and the gut communicate. The brain talks to the nerves in the digestive tract, and when the brain is stressed, it tells the digestive system to be stressed, too. This communication is called the brain-gut axis [2, 3]. Exercise is one way to calm the brain which, through the brain-gut axis, then will calm digestion. Without enough exercise, a stressed brain tells the digestive tract to be wary, which means it may not work properly.
Getting Your ZZZs
A minimum of 8 h of sleep a night is good for your brain and body, but also for your gut! IBS and sleep go together, and not only can a poor night’s rest cause IBS, but IBS symptoms, like pain that keeps people up at night, can also cause bad sleep. IBS is much more common in people who have sleeping disorders like insomnia. People who work during the night, like doctors and nurses, also have a higher risk of IBS. Researchers found that, in people with IBS, the number of hours of sleep they got the night before could predict how bad their bowel movements were the next day [4]. Just like exercise, this is likely influenced by the role sleep plays in brain health. Getting enough sleep keeps the brain in a good state, which means it sends the right signals to the digestive tract.
Enjoying the Sunshine
Spending time outside is not just fun, it is also good for your health. When you spend time in the sun, your body can make vitamin D, which is important for your bones and skin, and helps prevent you from getting sick. Vitamin D also helps keep the digestive system healthy. When you do not spend time outside, your vitamin D levels may be lower. This is exactly what we see in people with defecation issues, including IBS patients. Low levels of vitamin D are more common in people with IBS, and when people take vitamin D supplements as an IBS treatment, their digestive health improves [5]. Vitamin D plays an important role in keeping the intestines healthy. Your intestines are enclosed in the body, but sometimes they can leak fluids containing bacteria and stomach acid into the bloodstream, which can cause problems with bowel movements. Vitamin D makes sure the walls of the intestines are strong and thick, preventing any leaks [5].
Wrapping it Up
This article introduced you to IBS, a chronic illness that affects a lot of people in the United States and is responsible for uncomfortable changes in bowel movements, pain, and other digestive symptoms. Behavior has a large impact on overall health, and that goes for digestion as well. In addition to their bowel movement habits, behaviors like what people eat, to how much exercise and sleep they get, and the amount of time they spend outside can impact how likely they are to have IBS. Since IBS can significantly affect people’s quality of life, it is important for scientists to keep studying this digestive disorder, to better understand its mechanisms and triggers. This knowledge will hopefully lead to new treatments that may improve the lives of many people with IBS.
Glossary
Defecation: ↑ The process of digestion where a person passes waste from their body, or a bowel movement. This is also known as pooping.
Irritable Bowel Syndrome: ↑ A digestive illness where people experience pain as well as changes in how they poop, including how often and the consistency of poop.
Constipation: ↑ When a person is unable to have a bowel movement regularly (like <3 times per week), causing discomfort.
Gut Microbiome: ↑ The bacteria and other small microorganisms that live inside the digestive tract and help us digest food.
Risk Factors: ↑ Certain behaviors, traits, or environments that give a person a higher chance of getting a certain health condition.
Carbohydrates: ↑ Nutrients found in foods like bread, pasta, and fruits that provide energy to the body and are made up of sugar molecules.
Brain-Gut Axis: ↑ The connection between the nervous system of your digestive tract and your brain, which communicate with each other.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Nanayakkara, W. S., Skidmore, P. M., O’Brien, L., Wilkinson, T. J., and Gearry, R. B. 2016. Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date. Clin. Exp. Gastroenterol. 9:131–42. doi: 10.2147/CEG.S86798
[2] ↑ Schumann, D., Langhorst, J., Dobos, G., and Cramer, H. 2018. Randomised clinical trial: yoga vs. a low-FODMAP diet in patients with irritable bowel syndrome. Aliment. Pharmacol. Therapeut. 47:203–11. doi: 10.1111/apt.14400
[3] ↑ Lenover, M. B., and Shenk, M. K. 2023. Evolutionary medicine approaches to chronic disease: the case of irritable bowel syndrome. Evolut. Anthropol. 33:e22010. doi: 10.1002/evan.22010
[4] ↑ Ibrahim, N. K. 2016. A systematic review of the prevalence and risk factors of irritable bowel syndrome among medical students. Turk. J. Gastroenterol. 27:10–6. doi: 10.5152/tjg.2015.150333
[5] ↑ Linsalata, M., Riezzo, G., Orlando, A., D’Attoma, B., Prospero, L., Tutino, V., et al. 2021. The relationship between low serum vitamin D levels and altered intestinal barrier function in patients with IBS diarrhoea undergoing a long-term low-FODMAP diet: novel observations from a clinical trial. Nutrients 13:1011. doi: 10.3390/nu13031011
