Abstract
Focused ultrasound is a new technology that is being used to treat certain kinds of cancers in children, like cancer in the bones and brain. The approach is similar to the ultrasound that mothers receive to view their babies during pregnancy, only more powerful. The increased power of the ultrasound allows it to be used to treat the cancer, rather than just for imaging. How does focused ultrasound work? What type of childhood cancers can it treat? What are the advantages and disadvantages of focused ultrasound compared to more traditional treatments like surgery, chemotherapy, and radiation therapy?
What Is Focused Ultrasound?
If you were to see a focused ultrasound (FUS) system, you might think it looks like something from a science fiction film—but instead, it is a new type of cancer treatment. To treat a brain tumor, for example, the patient places their head into a futuristic-looking helmet, then slides into a colossal magnetic resonance imaging (MRI) scanner. The system allows doctors to both see the brain tumor and to treat it, without even making an incision in the skull. The contraption might seem more fitting aboard an interstellar spaceship, for treating a brain tumor in a Jedi, but the technology is now being used to treat cancers in kids.
Ultrasound is sound with frequencies above the human hearing threshold of 20 kHz. Bats use ultrasound to locate objects they cannot see. Similarly, ultrasound is used in medicine to visualize objects inside the body. For example, it is used to see babies inside pregnant mothers. FUS concentrates the energy from many individual ultrasound waves, which can be used to heat things up—the way the sun rays can be concentrated through a magnifying glass. The device concentrates this focused ultrasound energy on a very small spot. The sound waves pass through the skin and the bones to heat a tumor located inside the body—without the need to cut through the skin. The temperature at the focal spot is hot enough to kill cancer cells, and the focal spot is moved across the tumor, killing the cancer cells in a process called ablation.
To help doctors know if they are heating the correct location, the MRI scanner is used to observe the treatment. The MRI scanner works like a camera, using magnets and radio waves to take photographs inside the body. Similar tissues have similar magnetic properties, and changes in the magnetic properties allow doctors to tell the organs apart. When focused ultrasound is performed during MRI, the temperature increase causes the FUS beam to appear as a bright spot—the brighter the spot, the higher the temperature.
This allows doctors to adjust the system to maintain the desired temperature and to steer the beam across the tumor. The change in temperature with time and the difference in the shade of gray in the MRI scans help the doctors determine if the tumor was fully treated.
FUS technology has been used to treat adult men with prostate cancer for many years, and has been integrated into standard treatment guidelines if cancer returns with radiotherapy. One of the main complications to approving FUS to a primary treatment option (such as surgery and radiotherapy) has been the lack of long-term data to compare risks and benefits. As FUS technology continues to improve [1], this technique may provide a new treatment option for many adult and childhood cancer types, such as liver cancer (Figure 1).
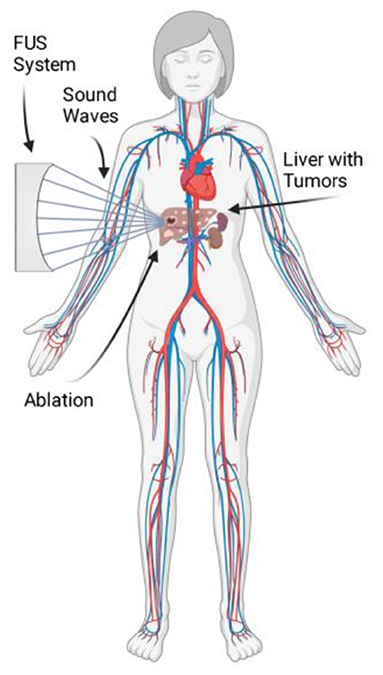
- Figure 1 - A child with liver cancer could be treated with FUS.
- The FUS system focuses the sound waves onto the tumor, heating up and killing the cells in a process called ablation. The focal spot is scanned across the tumor, to kill as much of the cancer as possible (Figure created with BioRender.com).
Common Pediatric Cancers
Tumors are an abnormal group of cells that grow much more than normal cells do. Some tumors are benign, meaning that they do not spread to other parts of the body, and they do not return after being removed by the doctor. Other tumors are malignant, meaning they can spread to other parts of the body and can also return later in life. Malignant tumors are often more dangerous and are called cancer.
Luckily, cancer in children—called pediatric cancer—is rare. The most common pediatric cancer types worldwide are shown in Figure 2. Leukemia, a cancer of the blood, is the most common pediatric cancer. The second most common pediatric cancer is brain cancer, including cancer of the central nervous system, such as the spine. The third most common pediatric cancer is non-Hodgkin’s lymphoma. Lymphoma is similar to leukemia, but the cancer cells collect in tissues as a large lump, instead of staying in the bloodstream (for more information on the treatment of blood cancers, see this Frontiers for Young Minds article).
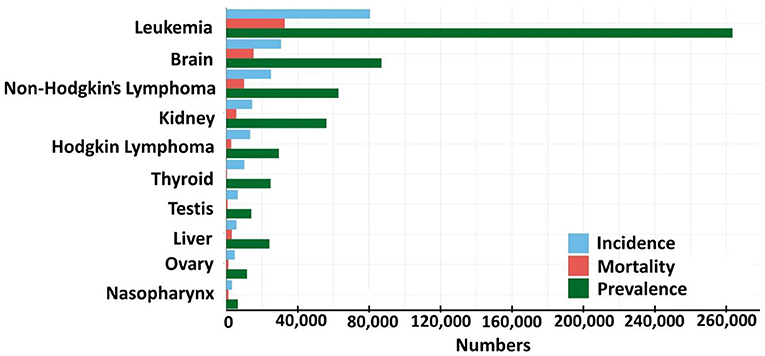
- Figure 2 - This graph shows the estimated number of boys and girls between the ages of 0–19 with cancer in 2020, all over the world.
- Incidence means the number of new cancer cases in the past 5 years. Mortality means the number of people that died from that type of cancer in 2020. Prevalence means the total number of kids living with the type of cancer (Source: GLOBOCAN).
How Is Cancer Normally Treated?
Cancer treatment depends on the situation and type of cancer. Surgery, chemotherapy, and radiation therapy are usually the main treatments. Cancer surgery involves cutting the tumor out of a person’s body. Chemotherapy is a special medicine used to treat cancer, which stops the cancer cells from growing, spreading, and returning. Radiation therapy works by sending X-rays to the cancer site to kill the cancer (for more information on X-ray therapy, see this Frontiers for Young Minds article).
Cancer treatments all have advantages and disadvantages. Surgery can often give the best results but can be painful. Chemotherapy and radiation therapy might be effective, but they can cause people to feel very sick and lose their hair. Cancer cells divide very quickly and chemotherapies are designed to kill dividing cells—but these therapies cannot distinguish between normal and unhealthy dividing cells. Cells in most normal tissues do not divide as frequently as cancer cells and are generally unaffected by chemotherapy. However, side effects result from the death of healthy cells that do divide quickly, such as cells in the lining of the intestines (resulting in nausea and vomiting), as well as skin and hair cells (leading to hair loss).
One main advantage of FUS is that it is non-invasive, which means that the doctor does not need to make an incision to treat the cancer. It is also non-ionizing, which means there is no radiation—this reduces the side effects. However, FUS is not without disadvantages. It is newer than surgery, chemotherapy, and radiation therapy, which makes predicting the results less certain. Also, FUS is not as effective as other treatments in certain situations. For instance, leukemias, the most common childhood cancers, are cancers of cells traveling in the bloodstream, so they cannot be treated with FUS.
What Type of Pediatric Tumors Can Be Treated With Focused Ultrasound?
The types of cancer that can be treated with FUS depends on the country. For example, in the United States, only pediatric tumors in the bones are normally allowed to be treated with FUS. Other types of pediatric tumors can be treated with FUS in special tests called clinical trials. In addition to bone tumors, soft tissue tumors like those in muscle tissue can be treated in countries other than the United States (for more information about where FUS can be used to treat various types of cancers, see here).
Clinical studies are now being performed using FUS to treat pediatric brain tumors. The doctors use MRI to see inside the brain during the treatment. An illustration of an FUS system for brain conditions is shown in Figure 3. The first successful FUS brain tumor ablation was reported in an adult patient in 2014 [3]. Results were recently published for the world’s first clinical trial for pediatric brain tumors, showing the procedure could be performed safely. Childhood brain tumors are often associated with seizures and reduced cognition, such as problems with memory and communication. The treatment significantly reduced seizure occurrence and showed a notable improvement in cognition [4].
![Figure 3 - FUS system with GE MRI, that is used to treat conditions in the brain (Reprint. Figure 1 from Magara et al. [2]. CC BY 2.0).](https://www.frontiersin.org/files/Articles/924872/frym-11-924872-HTML/image_m/figure-3.jpg)
Conclusions
Cancer treatment is very complicated and the treatment choices patients face can be confusing. New and improved therapies have extended the lives of a growing number of cancer patients. FUS is a new treatment currently being tested in clinical trials for various pediatric cancers, including brain cancer. Brain cancer is one of the most common childhood cancers and FUS has many potential benefits in the treatment of brain tumors. FUS is non-invasive, non-ionizing, and doctors can visualize the treatment using MRI. The number of pediatric cancer clinical trials involving FUS is increasing, and this technology will hopefully be used to successfully treat many cases of childhood cancer in the future.
Glossary
Focused Ultrasound (FUS): ↑ A technique to concentrate ultrasonic waves within the body, with the purpose of treating or diagnosing a disease.
Magnetic Resonance Imaging (MRI): ↑ An imaging method that uses a large magnet and radio waves to take images of structures inside the human body.
Frequencies: ↑ The number of times a sound wave oscillates each second.
Ablation: ↑ A medical treatment that heats cancer cells to destroy a tumor.
Benign: ↑ Irregular growth of certain tissues, but does not spread to nearby tissue or to other parts of the body.
Malignant: ↑ A type of cancerous cell that is capable of spreading to surrounding tissue or to other locations within the body.
Clinical Trial: ↑ A research study to test a new medical treatment, to evaluate how effective it is and whether it has dangerous side effects.
Cognition: ↑ Collection of mental processes used to acquire new knowledge, such as the processes of thinking and remembering.
Acknowledgments
Thanks to the Center for Biomedical Imaging and the Image-guided Interventions Laboratory for supporting the development of this manuscript. Thanks to Hailey Grace Bell for reviewing the article and providing constructive feedback. This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Skłodowska-Curie Grant Agreement No: 813766.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Original Source Article
↑ Lorton, O., Guillemin, P. C., M’Rad, Y., Peloso, A., Boudabbous, S., Charbonnier, C., et al. 2022. A novel concept of a phased-array HIFU transducer optimized for MR-guided hepatic ablation: Embodiment and first in-vivo studies. Front. Oncol. 12:899440. doi: 10.3389/fonc.2022.899440
References
[1] ↑ Lorton, O., Guillemin, P. C., M’Rad, Y., Peloso, A., Boudabbous, S., Charbonnier, C., et al. 2022. A novel concept of a phased-array HIFU transducer optimized for MR-guided hepatic ablation: Embodiment and first in-vivo studies. Front. Oncol. 12:899440. doi: 10.3389/fonc.2022.899440
[2] ↑ Magara, A., Buhler, R., Moser, D., Kowalski, M., Pourtehrani, P., and Jeanmonod, D. 2014. First experience with MR-guided focused ultrasound in the treatment of Parkinson’s disease. J. Ther. Ultrasound 2:1–8. doi: 10.1186/2050-5736-2-11
[3] ↑ Coluccia, D., Fandino, J., Schwyzer, L., O’Gorman, R., Remonda, L., Anon, J., et al. 2014. First noninvasive thermal ablation of a brain tumor with MR-guided focused ultrasound. J. Ther. Ultrasound 2:1–7. doi: 10.1186/2050-5736-2-17
[4] ↑ Tierney, T. S., Alavian, K. N., Altman, N., Bhatia, S., Duchowny, M., Hyslop, A., et al. 2022. Initial experience with magnetic resonance–guided focused ultrasound stereotactic surgery for central brain lesions in young adults. J. Neurosurg. 137:760–7. doi: 10.3171/2021.10.JNS21416
