Abstract
Have you ever pictured yourself as a LEGO®-mini-figure? That is pretty cool, right?! But now, instead of picturing yourself as an astronaut, superhero, or elf-figure, try to imagine your own body being miniature and built from LEGO®–one brick for each of your organs. Sound weird? Let us explain why a mini LEGO®-version of you could be extremely useful and could become reality in the future. Such technology might help end testing that uses laboratory animals and help your doctors understand your disease. We use people’s cells and small plastic housings to build mini-organs the size of small LEGO®-bricks, such as a beating heart or energy-storing fat tissue. Similar to playing LEGO®, we can also connect different organ-bricks and study how they talk and work with each other. In this article, we will tell you how this all works and why it is so much better than animal experiments.
Organs Are Made of Functional Units
Your body is full of organs, such as the heart or the eyes. You probably know that each organ is specialized for a different function: your heart pumps blood through your body and your eyes allow you to see what is happening around you. Almost all our organs consist of many smaller parts that are called functional units. Functional units are made of different types of cells that are very well-trained to perform their assigned tasks. Using the example of the heart, its functional unit is a fiber made from a few heart muscle cells that rhythmically contract. By bundling a great number of fibers together, the heart can pump blood throughout the entire body. Thanks to new discoveries and novel technologies, it is now possible to grow those functional units as mini-organs outside the body, without anyone getting cut open to remove their heart muscle cells first!
Functional Organ Units Outside the Human Body: Organ-on-Chip
A few years ago, scientists found a way to tell skin cells (specialized to sense your surroundings and protect you from damage) to de-specialize and turn back into cells that are similar to the ones found in embryos, called stem cells. Other scientists managed to convince stem cells to re-specialize again, even into cell types that are not in the skin. Taken together, it is now possible to transform your skin cells into any other type of cell, for example a heart muscle cell1.
However, these specialized cells growing alone outside the body, or in vitro (which is Latin for “in the glass”), may not be particularly comfortable. In the body, blood flow and contact with other cells and organs are the keys to keeping the cells happy and functional. To make the in vitro cells more comfortable, scientists have invented the Organ-on-chip technology. Do not let the term “chip” confuse you, these are not computer chips, but have a similar size and are made using similar methods (Figure 1A). Organ-on-chip bricks are made from polymers (kind of like plastic) and are mostly no bigger than a LEGO®-brick. They contain many small channels and chambers, like a house with rooms and hallways. Because these channels and chambers are so small, and because liquids or gases flow through them, the polymer bricks are called a microfluidic platform. The chambers provide a cozy environment for the cells, which helps them to forget that they are not in the body anymore. The cells can arrange themselves in their accustomed configurations and interact with their neighbor cells, similar to the way they would in the human body, forming mini-organs, or functional units (Figure 1B). Once settled down, the cells continuously feed on sugars and other nutrients that are dissolved in a liquid flowing through the channels next to their chambers, similar to blood flowing through blood vessels (Figure 1C). The nutrients can squeeze through tiny pores between the channels and the chambers, but the cells cannot escape the chambers. Similarly, the flow transports the cells’ waste products and messenger substances away.
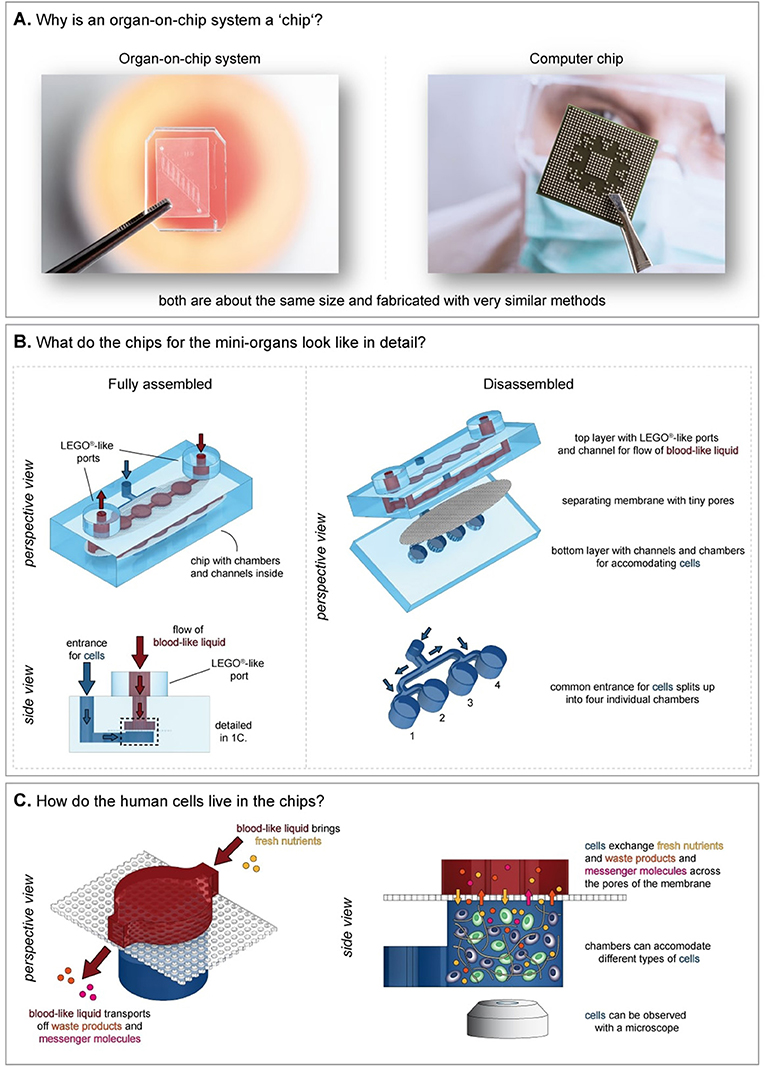
- Figure 1 - An example of an Organ-on-chip.
- (A) Organ-on-chip is called a “chip” because it is about the same size as a computer chip and made with similar methods. (B) An Organ-on-chip is the size of a small LEGO®-brick. It contains channels, chambers, and entrance ports. The chip has multiple layers. Here, the bottom and top layers sandwich a membrane. (C) The chambers in the bottom layer will contain cells. Cells are continuously supplied with fresh nutrients from the channel above. The waste products and messenger molecules from the cells are transported out with the flow. The cells can be viewed with a microscope, through a tiny window on the bottom of the chip.
Our lab has worked on miniaturizing heart and fat tissue [2, 3]. We have also developed miniature versions of the eye and the pancreas, and if we pooled the Organ-on-chip bricks from other labs around the world, we would have a nice collection of almost any organ in the human body.
Examples of Organ-on-Chip: Heart and Fat
To deliver its best performance, each organ has its own specific needs. Therefore, a chip housing heart muscle cells looks very different from a chip accommodating other cell types. The heart muscle cells, also called cardiomyocytes, are elongated and lined up next to each other. In a dog bone-shaped chamber, they can form a real muscle fiber and reach the maximum power for each heartbeat (Figure 2A and video in reference [3]).
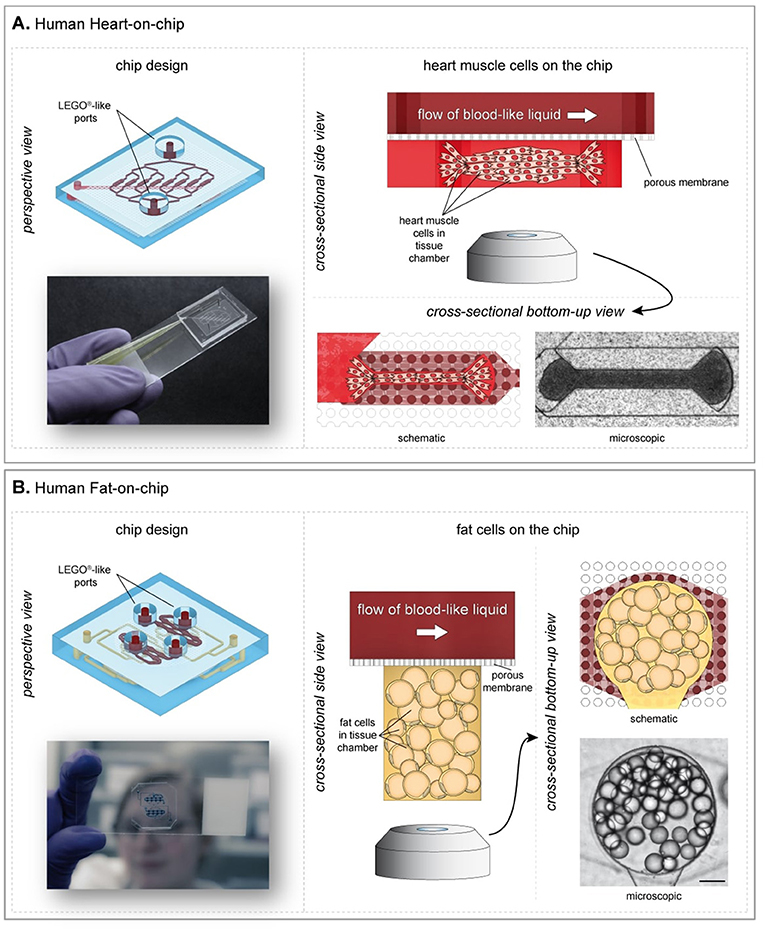
- Figure 2 - Examples of Heart- and Fat-on-chip.
- (A) Heart cells feel comfortable in a dog bone-shaped chamber, because they can align themselves to beat strongly. (B) The Fat-on-chip has two compartments. Adipocytes prefer cylindrical chambers (modified from Rogal et al. [3] and Loskill et al. [4]) (CC BY 4.0).
The fat tissue in your body, also called adipose tissue, stores or releases energy and signals to your brain whether you are hungry or have had enough to eat. Fat is an organ, too. Your fat cells, or adipocytes, are spherical and huge. They store energy from the food you eat. When another organ needs energy, for example in between meals, the adipocytes release it, to ensure that your body always has enough energy. Because the adipocytes do not like sharp edges, they feel most comfortable in cylindrical-shaped rooms entirely without any edges (Figure 2B and Video 1).
From Single-Organ to Multi-Organ-Chips
Despite their individual needs, each organ depends on other organs to perform best: the heart depends on the energy provided by the adipose tissue in between meals, while the adipose tissue depends on the heart to pump blood and provide fresh nutrients and oxygen. All organs communicate with each other using messenger molecules. Like nutrients and oxygen, these messengers travel through the blood stream. So, when you link two Organ-on-chip bricks using a connector brick, they end up with a common blood channel (Figure 3). The organs can then talk to each other. For example, the messenger molecules the heart sends to the fat may translate to “send more fuel.” The connection of many single Organ-on-chip bricks is called a multi-organ chip. With the LEGO®-like connections, there are no limits to the type or number of organs that can be linked [4, 5]. Multi-organ-chips that integrate mini-versions of all the major organs will eventually serve as a mini LEGO®-version of a human.
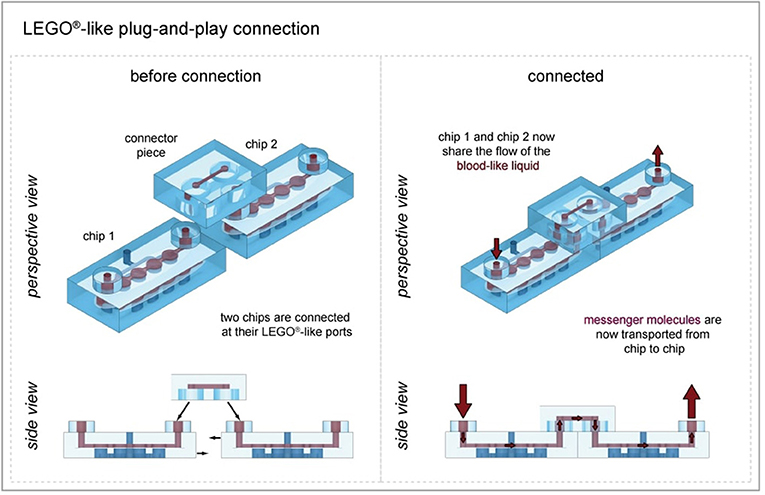
- Figure 3 - Building a mini-human by playing LEGO®.
- Using a connector brick, we can link two Organ-on-chip bricks in a LEGO®-like fashion; for example, chip 1 could be housing the adipose tissue and chip 2 the heart. After connection, the two chips share the same blood-like liquid and can interact with each other using messenger molecules.
How is Organ-on-Chip Technology Used?
So, why would we need Organ-on-chip technology? One of the most important applications for Organ-on-chip is the development of new medicines. Today, animals are used to discover if a medicine works or if it is too dangerous to be used in humans. Animal research is ethically questionable and, more than that, a mouse is not like a human being. Although some of the basic bodily processes might be similar, many processes differ immensely between humans and rodents. The heart of a mouse, for instance, beats 330–840 times per minute, while a human heart normally beats 70–100 times per minute. Because a mouse and a human are so different, a potential medicine might be found to be safe and effective in mice, but is later discovered to be toxic or ineffective in humans. If we use human Organ-on-chip systems, we can add a medicine to the blood-like liquid and then study whether the medicine works and/or if it does any harm. By doing this, we also would not need to use laboratory animals anymore to know if a medicine is safe.
The next level of using Organ-on-chip involves more than finding the right medicines for humans. It could be used to find the best medicine for each individual person. People differ in the ways their bodies handle diseases and react to medicines. Just because a certain medicine at a certain dose might help you treat a disease does not automatically mean it will help your friend, too. In the future, you might be able to painlessly donate cells to build an Organ-on-chip that represents you, and test whether a medicine will work for you personally. This area of research is called personalized medicine.
Conclusion
Organ-on-chip technology has become a powerful tool in recent years. By using modern engineering and new types of materials, researchers create artificial homes for cells that make them feel and behave almost the same as if they were in the human body. Combining the Organ-on-chip technology with new advances in stem cell technology, it is possible to create mini-organs from any individual, for example from you. Soon, Organ-on-chip technology is expected to help us to better understand diseases, to make new medicines safer and cheaper, and to help provide each patient with proper, personalized treatment.
Glossary
Stem Cells: ↑ Stem cells are very special cells that can both replicate themselves as often as they want and change into any other cell type in your body (the changing process is called differentiation).
Polymer: ↑ Polymers are huge molecules that are long chains containing many of the same small molecule. Plastic is an example of a polymer.
Microfluidic Platform: ↑ A polymer brick with small (as thin as a single hair or even thinner) channels and chambers through which a liquid or gas can be pumped.
Cardiomyocytes: ↑ Cardiomyocytes are a specialized cell type in the heart muscle tissue. They are elongated and can pull at each other to make the heart beat.
Adipocytes: ↑ Adipocytes are the specialized cell type in the fat tissue. Adipocytes are spherical and huge, and they store or release energy from the food you eat.
Video 1: ↑ Fat cells taking up fats (colored with a green dye) when food is plenty and releasing it when the food supply stops.
Personalized Medicine: ↑ Because every human is unique, medicines often work differently in different patients. To give every patient the best possible treatment, researchers try to create personalized medicines, specific for each person.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
1. ↑ If you want to learn how this method works, check out this Frontiers for Young Minds article that explain the stem cells in greater detail [1].
References
[1] ↑ Luk, F., Eggenhofer, E., Dahlke, M., and Hoogduijn, M. 2017. The use of stem cells for treatment of diseases. Front. Young Minds 5:9. doi: 10.3389/frym.2017.00009
[2] ↑ Schneider, O., Zeifang, L., Fuchs, S., Sailer, C., and Loskill, P. 2019. User-friendly and parallelized generation of human induced pluripotent stem cell-derived microtissues in a centrifugal heart-on-a-chip. Tissue Eng. A 25:786–98. doi: 10.1089/ten.TEA.2019.0002
[3] ↑ Rogal, J., Binder, C., Kromidas, E., Roosz, J., Probst, C., Schneider, S., et al. 2020. WAT-on-a-chip integrating human mature white adipocytes for mechanistic research and pharmaceutical applications. Sci. Rep. 10:66. doi: 10.1038/s41598-020-63710-4
[4] ↑ Loskill, P., Marcus, S. G., Mathur, A., Reese, W. M., and Healy, K. E. 2015. μOrgano: a Lego®-like plug & play system for modular multi-organ-chips. PLoS ONE 10:e0139587. doi: 10.1371/journal.pone.0139587
[5] ↑ Rogal, J., Probst, C., and Loskill, P. 2017. Integration concepts for multi-organ chips: how to maintain flexibility?! Future Sci. OA 3:FSO180. doi: 10.4155/fsoa-2016-0092
