Abstract
Why do we get sick? Medical doctors would say there are many causes, depending on the sickness: the SARS-CoV2 virus causes COVID-19, poor eating habits cause obesity, smoking causes lung cancer. But what if we looked at this question differently…as a species, why have we evolved bodies that are vulnerable to getting sick? Should we not have evolved to be healthy all the time? The field of evolutionary medicine aims to join ideas from medical science with ideas from evolutionary science to better explain health and disease. This approach could provide entirely new ideas for treating human health threats like cancer, antibiotic-resistant bacteria, obesity, and COVID-19, just to name a few!
Evolution can Help us Understand Health and Disease
Have you ever thought about what causes us to get sick? You might say that it depends on the sickness—the SARS-CoV2 virus causes COVID-19, poor eating habits cause obesity, smoking causes lung cancer, and so on. While these things certainly DO make us sick, what if we looked at the question a little bit differently…why do we even have bodies that are vulnerable to getting sick in the first place? If evolution is truly “survival of the fittest,” why does the human species—or any animal species, for that matter—have bodies that get sick at all? While most medical doctors are more concerned with the direct causes of disease, an exciting new field called evolutionary medicine seeks to blend knowledge from medical science with important ideas from the field of evolutionary science, to provide unique insights into health and disease [1].
What exactly can evolutionary ideas teach us about human diseases? Well, for one thing, most “human” diseases are not purely “human”—other animals get them, too. On the other hand, certain animal species are resistant to human diseases, meaning they are somehow protected. Understanding what makes various animal species susceptible (sensitive) or resistant to (protected from) “human” diseases can give us insights into the mechanisms of those diseases and how to fight them. Second, since the process of evolution often involves organisms “resisting” things in their environments that threaten their health (bacteria, viruses, antibiotics, or pesticides, to name a few) evolutionary medicine can help us to address the “battle” between humans and infectious organisms or cancer cells. Finally, evolutionary medicine gives us a new way of looking at “modern” human diseases like obesity and diabetes. What if, for example, although obesity is directly caused by bad eating habits, it also results from a mismatch between the environment past humans evolved in (where food was scarce) and today’s environment (where food is easy to get)? Understanding this mismatch might open doors to new treatments or preventions. In short, evolutionary medicine might help us approach many human-health challenges in new, more effective ways!
What can we Learn From Other Species?
Earth’s animal species are extremely diverse—animals have evolved many unique features that help them to survive and thrive in their specific environments. Some evolved features appear to protect certain species against common human diseases, from infections to cancer to heart disease (Figure 1). Because animal species are so diverse, there are probably many examples of disease resistance in nature. Furthermore, many non-contagious “human” diseases (cancer, diabetes) also exist in other species, including heart diseases, melanoma, breast and lung cancer, cataracts, and arthritis. By studying animals that either get “human” diseases or disorders or do not get them, scientists and doctors might be able learn things that help them understand why humans suffer from these conditions.
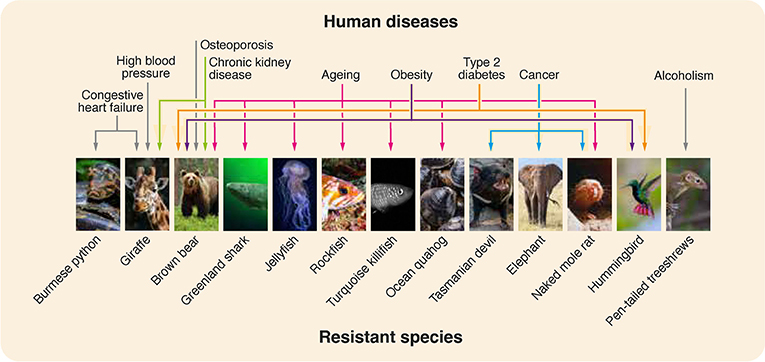
- Figure 1 - Certain animal species have evolved to be resistant to various diseases or disorders that commonly affect humans.
- Studying the unique characteristics of resistant species could help researchers and doctors to better understand these diseases and might speed up the development of new treatments or cures. Human diseases are listed along the top and the colored arrows indicate animals that show resistance to each disease. Different colors were used to make the arrows easier to follow. Figure originally published in [2] in Frontiers in Science.
Before we can benefit from this knowledge, patterns of disease resistance and susceptibility in animals must be identified. This is not easy because many types of human diseases have not yet been studied across species and, even when they have, veterinarians and human doctors do not exchange knowledge as often as they should. If samples from both captive and wild animals were regularly collected and studied after their death, information about their vulnerability to diseases could be gathered in a database. That database could inform doctors and researchers, possibly leading to new treatments, or cures [3].
The Evolutionary “Arms Race”
Evolution involves adaptation—random changes to an organism’s genetic material that help it to survive in its environment, increasing its chances of successfully reproducing and passing its genes to new generations. One way to understand this is as a process of resistance and counter-resistance, kind of like an “arms race” between nations, in which each nation is constantly trying to have the strongest weapons. The evolution of antibiotic-resistant bacteria is an excellent example of this process. Bacteria reproduce quickly (every 20 min or less!), so it is much easier to see and study adaptations in bacteria than it is in humans or other organisms that take years to grow and develop. How does antibiotic resistance happen? Let us imagine a person is infected with a strain of bacteria that is generally sensitive to the antibiotic penicillin. If we “resist” the infection by treating the person with a high dose of penicillin, most of the infecting bacteria will die quickly. However, if one or a few bacteria have a mutation that “resists” the effects of penicillin, those protected bacteria will continue to grow in the presence of the drug. As the penicillin-sensitive bacteria die, the penicillin-resistant bacteria suddenly have a lot of space and resources all to themselves! Before long, the entire population of bacteria in the person’s body will have adapted to resist the penicillin-containing environment—and the only bacteria left will be those that are resistant to penicillin (Figure 2)! If these bacteria spread to another person, the resulting infection will not respond to penicillin treatment.
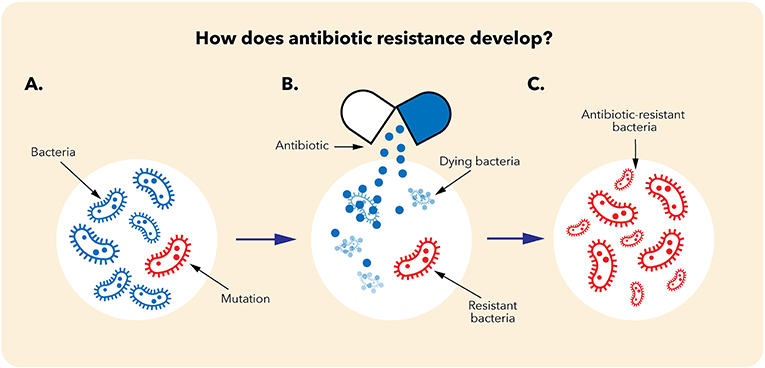
- Figure 2 - How does antibiotic resistance develop?
- (A) In a population of bacteria, most bacteria will be sensitive to the antibiotic used to treat the infection (blue). However, one or a few bacteria might have a mutation that protects them (red). (B) When the antibiotic is given, the sensitive cells will die, leaving only the resistant cells—which suddenly have lots of space and resources. (C) The resistant cells then divide, creating a new population of antibiotic-resistant bacteria. The evolution of chemotherapy resistance by cancer cells occurs by the same process.
The situation is similar for cancer cells [4]. Cancers are often treated using medicines called chemotherapy drugs. High doses of a chemotherapy drug cause the cancer cells that are most susceptible to that drug to die, leaving a population of chemotherapy-resistant cancer cells that can divide and create more resistant cells—just like we saw with bacterial antibiotic resistance. Once the chemotherapy drug stops working, the drug-adapted cancer can grow rapidly and eventually harm or kill the patient. People in developed countries rarely die from drug-sensitive bacterial infections or cancers, so the critical medical problem in both of these cases is the evolution of resistance.
The traditional way to fight antibiotic or chemotherapy resistance is to keep developing new drugs to replace those that fail. While this approach can work for a while, it is expensive and time consuming. More importantly, bacteria and cancer cells keep adapting—developing new and stronger types of resistance. For example, some bacteria have evolved molecular pumps that can get rid of multiple types of drugs—even drugs that have not been invented yet! Instead of continuing to develop new drugs that will eventually fail, maybe we could use an evolutionary medicine approach, and tackle the evolutionary process itself! But how?
Fighting Infectious Diseases and Cancer With Evolutionary Ideas
The principles of evolutionary medicine give us several ideas for fighting antibiotic or chemotherapy resistance [4, 5]. The first approach involves using existing drugs in better ways—ways that are less likely to lead to the evolution of resistance in the first place. For example, we could try combining drugs or adjusting their concentrations to lessen the evolution of adaptations, or we could try switching back and forth between drugs over time. Adaptive therapy for cancer aims to use lower doses of chemotherapy drugs—not to kill the cancer outright, but to keep it drug sensitive and under control for as long as possible. Another approach, called extinction therapy, does aim to eliminate cancer—by first using one drug to reduce the number of cancer cells and then, while the first drug is still working, switching to a different drug to kill the remaining cells. Extinction therapy is based on what scientists have learned from the extinction of animal populations—extinction often starts with a decrease in population size, which is then followed by a new natural event, like a major food shortage or a change in climate, that kills the remaining individuals.
Alternatively, we could develop therapies that interfere with the evolutionary process itself. Approaches involve preventing bacteria from “sharing” resistance genes (which they generally do very well) or by using other drugs together with traditional antibiotics—drugs that kill only those bacteria that develop resistance. For fighting bacterial infections, phage therapy is another unique alternative. Phage are viruses that are harmless to human cells but can infect bacteria and destroy them, while simultaneously producing many more phage—acting like self-replicating “drugs”! However, just as bacteria can become resistant to antibiotics, they can become resistant to phage. If scientists understand the evolutionary processes that result in resistance, they might be able to engineer phage that causes the “right” kind of resistance in the bacteria they infect. What if, for instance, when bacteria develop resistance to a specific phage, they simultaneously become less dangerous or more susceptible to antibiotics or to the body’s own defenses [6]? Maybe phage could be designed to block the antibiotic-expelling molecular pump mentioned earlier, for example.
When Evolution cannot Keep up With Our Changing Lives
Evolutionary medicine can help us understand more than just disease vulnerability and resistance–it can help us make sense of how our rapidly changing societies and cultural practices are causing evolutionary mismatch between our current environment and the characteristics that helped us to thrive in the environments that existed during our long evolutionary history. Evolution is a slow process—much slower than cultural change. When an organism is exposed to a new environment, adaptations that served an important function in the past might no longer be helpful and might instead cause disease [7].
Let us take poor eating habits and they health effects they cause as an example. Food-related health disorders like obesity, heart disease, and type-2 diabetes have been increasing in high-income societies since World War II and, while they are often viewed as “lifestyle” diseases that should be treated with healthier diets and more exercise, these disorders might be more accurately described as a problem of evolutionary mismatch (Figure 3). In our evolutionary past, food was much more difficult to get and processed foods—high in fat, calories, and sugars—did not exist. Thus, our “nutritional ecosystem” changed more quickly than the human species could evolve. Our bodies are not adapted to eating the types (and amounts) of food that are easily available today. The result is increasing levels of obesity and its associated health disorders.
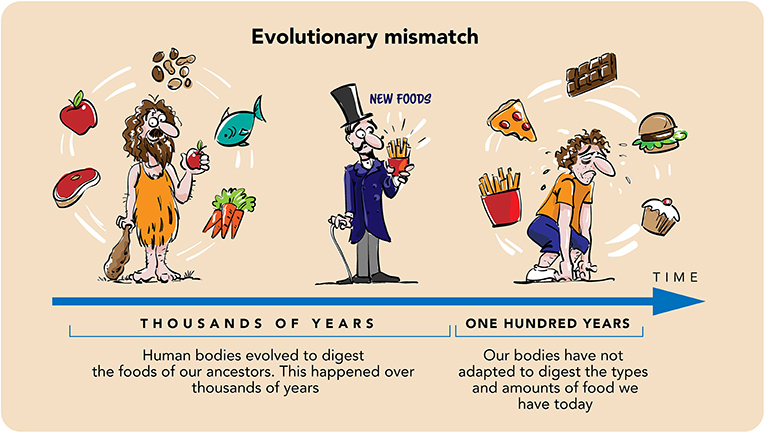
- Figure 3 - The common occurrence of food-related health disorders that we see today is an example of evolutionary mismatch.
- Human bodies evolved to digest the foods of our ancestors, which were sometimes scarce and generally low in fat and sugar. Evolution is a very slow process, while our “food ecosystem” has changed quickly. Our bodies have not adapted to digest the types and amounts of food available to us today, so overeating or eating the types of foods easily available today can result in disease.
The Future Is Evolutionary!
Even with all the progress doctors and scientists have made toward understanding the causes, symptoms, and treatments of various diseases, humans continue to face serious and newly emerging health threats. We hope you now have a clearer picture of why our bodies are susceptible to diseases in the first place, and why threats to human health keep emerging. Evolutionary medicine blends knowledge from medical science and evolutionary science to give us unique and unusual insights into viral and bacterial diseases, cancers, obesity, heart disease, and type-2 diabetes, to name just a few. Studying patterns of susceptibility and resistance in other species can teach us about human diseases; thinking about the evolution of resistance can lead to new treatments for cancer and antibiotic resistance; and viewing “modern” human diseases as a mismatch between our past and current environments can provide fresh perspectives on these health threats. This novel, blended approach to human disease could ultimately improve the health of people all over the world.
Glossary
Evolution: ↑ The process by which animals change over generations to better survive in their environments. Evolution occurs by natural selection—the best-adapted animals are the most likely to reproduce and pass on their genes.
Evolutionary Medicine: ↑ A relatively new field that combines ideas from evolutionary science with ideas from medical science, with the aim of improving human health in novel ways.
Adaptations: ↑ Physical or behavioral characteristics that help an organism to survive in its environment.
Antibiotic-Resistant Bacteria: ↑ Bacteria that have evolved to survive in the presence of drugs (antibotics) that were developed to kill them.
Adaptive Therapy: ↑ A type of cancer therapy in which low doses of chemotherapy drugs are used to keep the cancer under control for a long time, without totally killing it.
Extinction Therapy: ↑ A type of cancer therapy in which one drug is used to reduce the number of cancer cells, then a second drug is used to kill any drug-resistant cells that remain.
Phage Therapy: ↑ The use of viruses that specifically infect and kill bacteria to treat bacterial infections; a potential alternative to antibiotics.
Evolutionary Mismatch: ↑ When helpful characteristics that an organism evolved in past environments are no longer helpful—and might even cause disease—in the current environment.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Co-written by Susan Debad Ph.D., graduate of the University of Massachusetts Graduate School of Biomedical Sciences (USA) and scientific writer/editor at SJD Consulting, LLC. Athena Aktipis, Carl T. Bergstrom, Molly Fox, Peter D. Gluckman, Felicia M. Low, Ruth Mace, Andrew Read, and Paul E. Turner were co-authors on the original manuscript.
Original Source Article
↑Natterson-Horowitz, B., Aktipis, A., Fox, M., Gluckman, P. D., Low, F. M., Mace, R., et al. 2023. The future of evolutionary medicine: sparking innovation in biomedicine and public health. Front. Sci. 1:997136. doi: 10.3389/fsci.2023.997136
References
[1] ↑ Damas, J., Hughes, G. M., Keough, K. C., Painter, C. A., Persky, N. S., Corbo, M., et al. 2020. Broad host range of SARS-CoV-2 predicted by comparative and structural analysis of ACE2 in vertebrates. Proc. Natl. Acad. Sci. U.S.A. 117:22311–22. doi: 10.1073/pnas.2010146117
[2] ↑ Natterson-Horowitz, B., Aktipis, A., Fox, M., Gluckman, P. D., Low, F. M., Mace, R. et al. 2023. The future of evolutionary medicine: sparking innovation in biomedicine and public health. Front. Sci. 1:997136. doi: 10.3389/fsci.2023.997136
[3] ↑ Natterson-Horowitz, B., and Bowers, K. 2013. Zoobiquity: The Astonishing Connection Between Human and Animal Health. New York, NY: Vintage.
[4] ↑ Aktipis, A. 2020. The Cheating Cell: How Evolution Helps Us Understand and Treat Cancer. Princeton, NJ: Princeton University Press.
[5] ↑ Hansen, E., Karslake, J., Woods, R. J., Read, A. F., and Wood, K. B. 2020. Antibiotics can be used to contain drug-resistant bacteria by maintaining sufficiently large sensitive populations. PLoS Biol. 18:e3000713. doi: 10.1371/journal.pbio.3000713
[6] ↑ Goldhill, D. H., and Turner, P. E. 2014. The evolution of life history trade-offs in viruses. Curr. Opin. Virol. 8:79–84. doi: 10.1016/j.coviro.2014.07.005
[7] ↑ Gluckman, P., and Hanson, M. 2019. Ingenious: The Unintended Consequences of Human Innovation. Cambridge: Harvard University Press.
