Abstract
Severe acute malnutrition is a life-threatening condition that affects millions of children worldwide. For many years, treatment was only available in hospitals, requiring special feeding routines, clean water, refrigeration, and trained medical staff. Dr. André Briend helped change that by developing a new kind of treatment called ready-to-use therapeutic food—a safe, nutritious paste that children can eat at home without needing special preparation. He also helped promote a simple measuring tool called mid-upper arm circumference, which makes it easier to find children who are most at risk of dying from malnutrition. These two simple tools made it possible for families to get life-saving care at home, without the need for long hospital stays—even in remote areas. Thanks to Dr. Briend’s work, millions of children have received faster treatment, improved nutrition, and a better chance to survive, recover, and grow up healthy.
Dr. André Briend was awarded the 2025 John Dirks Canada Gairdner Global Health Award “For the invention of a ready-to-use therapeutic food, which has revolutionized management of severe acute malnutrition in children, allowing treatment to shift from inpatient care to community-based management and saving countless lives”.
A Different Kind of Hunger
Most people have felt hungry at some point—maybe you skipped breakfast because you were late for school or had to miss lunch to make up a missed assignment. You might have felt your stomach growl or found it hard to concentrate in class. That kind of hunger is uncomfortable, but it usually goes away once you eat.
In some cases, hunger becomes something much more dangerous and does not go away after a meal. Severe acute malnutrition is a medical emergency. It happens when a child’s body does not get enough of the energy and nutrients it needs, not just for days, but for weeks or months. When this happens, the body begins to break down. Muscles shrink, energy disappears, and the immune system becomes too weak to fight off infections. Severe acute malnutrition affects about 19 million children, especially in low-income countries. Worldwide, it is one of the leading causes of death in children under five—and yet it is often preventable and treatable.
For many years, the main way to treat severe acute malnutrition was in a hospital. Children were given special milk-based diets through careful feeding routines several times a day. This kind of care was not easy to provide, however. The milk had to be mixed with clean water, used quickly, and kept cold in between feedings to keep it from spoiling. That means hospitals needed safe water, refrigeration, trained staff, and close monitoring to keep the treatment safe—things that were often in short supply.
In many places, hospitals were overcrowded, did not have enough staff, and were too far from children’s homes. Families had to travel long distances and sometimes wait for days to get a bed. Once treatment began, it could take weeks—and many parents could not afford to stay at the hospital that long, especially if they had other children at home or jobs to go to. Some children never reached a hospital at all, and others left before they fully recovered.
When I worked as a young doctor in Africa and Asia, I saw this problem firsthand. Too many children were dying because the right care was out of reach for them and their families. I wanted to find a better way.
A Paste That Changed Everything
In the late 1990s, I began thinking about a new kind of food to treat severe acute malnutrition—one that could be just as effective as hospital diets, but easier to use and safer in places without clean water or electricity. Instead of starting from scratch, I tried to connect simple facts we already understood to find a better solution.
To recover from malnutrition, children need food that is dense in energy, especially from fat. I already knew that the liquid, milk-based hospital diets were dangerous outside the hospital because bacteria grows quickly in foods that have water in them. Bacteria need both food and water to grow, so I had an idea: if we could make a high-fat food that did not contain water, it might be much safer to use in the community. And if it tasted good, children would eat it on their own.
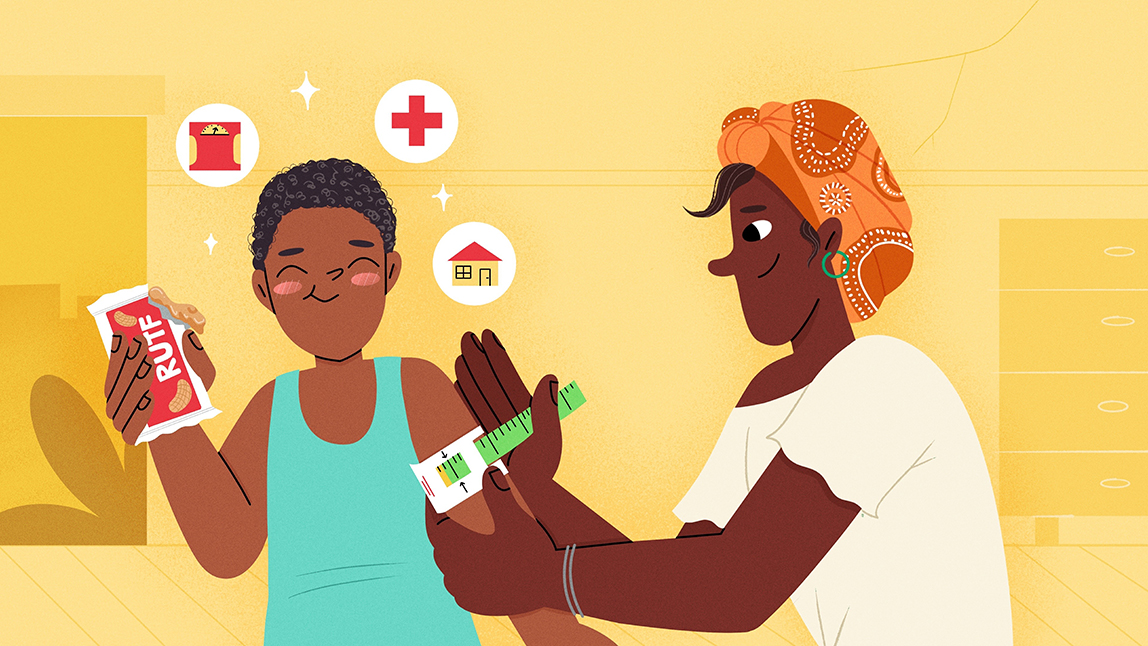
I worked with a food technologist named Michel Lescanne and, together, we explored several options: biscuits, bars, pancakes, and even doughnuts. But these were either too fragile, too hard to store, or the cooking or baking process needed to make them destroyed some of the vitamins children required. Then we realized that a spread—like a nut butter—might work. It could hold all the nutrients of the hospital milk formula, but without the water. We replaced some of the dried milk in the original hospital recipe with peanut butter and created a paste that has the same nutritional value, lasts for months without the need for refrigeration, and tastes good. We tested it for safety by contaminating a sample on purpose—and found that bacteria could not grow in it. That meant it could be stored without refrigeration and safely eaten straight from the packet. The end product was what we now call ready-to-use therapeutic food (RUTF; Figures 1A, B).

- Figure 1 - (A) RUTF is an energy-dense paste that comes in easy-to-use packets and lasts for months without the need for refrigeration (Wikimedia Commons, CC BY 2.0).
- (B) Children can eat RUTF right from the packet at home, reducing the need for hospital stays to treat their malnutrition (Flickr, CC BY-NC 2.0). (C) A MUAC tape being used to measure a child’s upper arm circumference. If the reading is in the red range, the child is in danger of dying from severe acute malnutrition. Yellow indicates they are at risk, and green means they are likely to be okay (Wikimedia Commons, CC BY-SA 2.0).
At first, we tested RUTF in hospitals to make sure there were no adverse effects and to check how it compared to the standard treatment. The results were better than expected. Children liked RUTF and ate it easily, gained weight faster, spent less time in treatment, and recovered just as well—or even better [1, 2]. Even though the idea of treating malnutrition with a sweet, peanut-based spread seemed strange to many experts at the time, we began to wonder: if this paste worked in the hospital, could it also work in the home?
From Hospitals to Family Homes
Once RUTF had been shown to work in hospitals, the next step was to see whether it could help children recover at home. Home-based treatment was a major shift in thinking that many experts did not agree with. But I knew that if a safe, nutritious food could be used outside the hospital, we would be able to reach many more malnourished children—especially in areas where hospitals were overcrowded or far away.
Although I did not lead the first community trials myself, several researchers were willing to test this new approach. In Malawi, a team of researchers began giving RUTF to children in their own homes [3]. Around the same time, another researcher worked with community health programs in Ethiopia and other countries [4]. Their early results were clear: children treated at home with RUTF gained weight, recovered well, and were more likely to finish treatment.
These studies helped change the way people thought about treating malnutrition. When families could give the treatment themselves, care started earlier, reached more children, and fit better with real life (Figure 2). That made recovery faster, safer, and more successful.
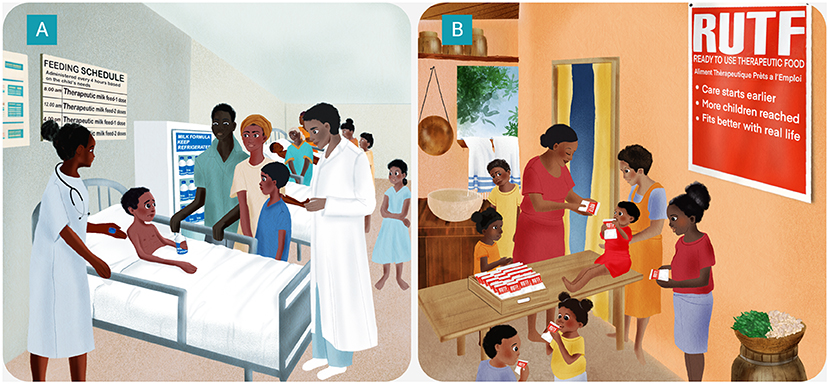
- Figure 2 - RUTF changed treatment of severe acute malnutrition.
- (A) Before RUTF, treatment involved long hospital stays during which children received a milk-based formula on a regular schedule. The formula required refrigeration so it would not spoil. Hospitals were often crowded and sometimes families lived far away and could not stay for the whole treatment. (B) RUTF has many advantages over the traditional milk-based therapy. Studies showed that malnourished children who ate RUTF at home gained weight, recovered well, and were more likely to finish treatment (Figure credit: somersault18:24 Studio BV).
Finding the Kids Who Need Help Most
Even the best treatment cannot help if we do not know which children need it. For many years, the main way to identify severe malnutrition was by comparing a child’s weight to their height. This required careful measurements, special equipment, and complicated charts—things that were difficult to use in crowded clinics or rural villages.
A simpler option is to take a measurement called mid-upper arm circumference (MUAC) (Figure 1C). This method uses a small, color-coded measuring tape that wraps around the middle of a child’s upper arm. Children with severe malnutrition often have very thin arms, so a small measurement can be a warning sign. If the tape shows red, the child is in danger. Yellow means they are at risk. Green means they are likely to be okay. It only takes a few seconds, and even parents or community volunteers can learn to do it.
I was not the first person to suggest using MUAC—that idea had been around for years. But during my research in Senegal and Bangladesh, I helped show something crucial: that MUAC could accurately identify the children who were most at risk of dying from severe acute malnutrition [5]. In other words, it was not just easy to use—it was effective. Today, MUAC is used around the world to spot malnutrition sooner, so that children can get help before it is too late.
From Doubt to a Worldwide Shift
When we first introduced the idea of using a spread to treat severely malnourished children, many experts did not believe it would work. They were convinced that children who were this sick could only recover by drinking liquid formulas in a hospital, where they could be taken care of by trained staff. A peanut-based paste seemed too simple…and too risky. Some even told us the idea would never succeed.
As more researchers studied the use of RUTF in the community, the results became hard to ignore. Children liked the paste, ate it easily, gained weight, and got better. Families liked being able to treat their children at home. Even for those with complicated cases who still needed hospital care, the time spent in the hospital was considerably shorter and, after the complications were treated, malnutrition treatment could be continued safely at home. The evidence changed opinions—and policies. Today, more than 70 countries use RUTF to treat severe acute malnutrition. UNICEF now calls it a “wonder food”, and the World Health Organization includes it on its list of essential medicines. In 2022 alone, UNICEF obtained enough RUTF to treat an estimated eight million children.
When others doubted the idea, I kept going—because I believed it could help. Now when people who use RUTF tell me that it saves many lives, that is very rewarding for me. However, thinking about past successes should not cause us to forget that many children are still suffering from malnutrition—so, trying to improve their situation should still be a major focus. Many scientists from all over the world are working to improve the effectiveness of the current RUTF recipe or trying to make it less expensive. Others are developing products that are better suited for children with health complications, while still others focus on preventing malnutrition in the first place. I try to follow all this research the best I can, offering advice whenever I have the opportunity to help.
A Message From the Scientist Who Helped Change the System
My goal has always been to make sure that children with severe malnutrition can get the care they need, no matter where they live. That meant finding practical solutions, testing them carefully, and working with others to make them available around the world. What inspired me the most was simple: watching a child who had been too weak to smile recover and smile again. That moment reminds me why the work matters.
This kind of progress—turning a scientific idea into a simple tool that helps millions of people—requires teamwork. My role was to connect commonly known facts from different fields and work with others to turn those ideas into something useful. Some of the most important breakthroughs happen when people from different backgrounds—medicine, nutrition, and food science, for example—listen to one another and build on each other’s work.
If you are curious about food, health, or fairness, there are many ways to make a difference. You might become a scientist, a doctor, an engineer, or something else entirely, but the important thing is to stay open-minded, keep asking questions, and look for new ways to use what you already know—especially by working with others. Even problems that seem too big to fix can be solved through small, practical ideas and teamwork.
Glossary
Severe Acute Malnutrition: ↑ A serious condition where the body does not get enough nutrients over time, causing weight loss, weakness, and a higher risk of infection and death.
Nutrients: ↑ The parts of food that the body needs to grow, stay healthy, and have energy. These include proteins, fats, vitamins, and minerals.
Ready-to-use Therapeutic Food (RUTF): ↑ A special kind of food paste used to treat children with severe malnutrition. It does not need to be cooked or mixed with water.
Mid-upper Arm Circumference (MUAC): ↑ A quick way to check for malnutrition by measuring around a child’s upper arm. A small measurement can be a warning sign.
Conflict of Interest
AB was a consultant for Nutriset, the company that industrially produced the earliest RUTF, during the development and testing phases, from 1996 to 2003.
Acknowledgments
I wish to thank Dr. Susan Debad for her thoughtful questions, collaborative input, and her contributions as co-author. Figure 2 was created by Somersault18:24. Written informed consent was obtained from the individual(s) for the publication of any identifiable images or data included in this article.
AI Tool Statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
[1] ↑ Briend, A., Lacsala, R., Prudhon, C., Mounier, B., Grellety, Y., and Golden, M. H. 1999. Ready-to-use therapeutic food for treatment of marasmus. Lancet 353:1767-8.
[2] ↑ Diop, E. H. I., Dossou, N. I., Ndour, M. M., Briend, A., and Wade, S. 2003. Comparison of the efficacy of a solid ready-to-use food and a liquid, milk-based diet for the rehabilitation of severely malnourished children: a randomized trial. Am. J. Clin. Nutr. 78:302–7. doi: 10.1093/ajcn/78.2.302
[3] ↑ Manary, M. J., Ndkeha, M. J., Ashorn, P., Maleta, K., and Briend, A. (2004). Home based therapy for severe malnutrition with ready-to-use food. Arch. Dis. Child 89:557–61. doi: 10.1136/adc.2003.034306
[4] ↑ Collins, S., and Sadler, K. 2002. Outpatient care for severely malnourished children in emergency relief programmes: a retrospective cohort study. Lancet 360:1824–30. doi: 10.1016/S0140-6736(02)11770-3
[5] ↑ Briend, A., Wojtyniak, B., and Rowland, M. G. 1987. Arm circumference and other factors in children at high risk of death in rural Bangladesh. Lancet 2:725–8.