Abstract
Have you ever wondered how doctors can see inside your muscles, joints, and bones without ever opening you up? Thanks to today’s imaging technologies, they can see everything from broken bones to torn ligaments using all kinds of different equipment. From old X-rays to advanced MRI machines, each has its uses and benefits. Some enable quick, easy pictures; others enable very accurate 3D images. With a group of tools at their fingertips, doctors can choose the best tool for every individual case, to arrive at the right diagnosis and to allow them to do the best they can for their patients.
The Musculoskeletal System
If you imagine what a human body is made up of, what comes to mind? You can see your skin, face, arms, and legs, but beneath all of that, there is a basic structure that holds everything together—the skeleton. Your skeleton is made of all your bones and is the structure of your body. Your bones perform many functions, such as holding minerals and making blood cells, but they are mostly responsible for giving shape and support to your body.
Though they are also necessary for movement, bones by themselves alone do not allow you to move. They need the help of your muscles, ligaments, and tendons—that is where the musculoskeletal system comes into play. The musculoskeletal system is a complex team of bones, joints, muscles, ligaments, tendons, and cartilage that all work together to provide movement, absorb impact, and keep a straight posture. Bones are similar to columns of a building, giving your body its shape and holding it upright. Muscles are like motors that stretch and tighten to create movement. Tendons are like strong cables that attach muscles to bones and allow the muscles to pull on bones to get you moving. Joints are like hinges that let doors open and close, or like knobs and holes of puzzle pieces, that allow your bones to move while staying connected with each other. Ligaments are tough bands of tissue that hold bones together at the joints. Cartilage is a soft, cushioning tissue that covers the edges of your bones within joints, allowing them to glide smoothly and enabling you to move freely, without pain. Together, all these parts of the musculoskeletal system work like a well-designed machine, allowing you to run, jump, dance, and play your favorite sports!
What Can Go Wrong With the Musculoskeletal System?
You use your musculoskeletal system pretty much all day every day. There are hundreds of ways you can injure your bones, muscles, and joints, which can make movement difficult and painful. A fall can cause a fracture, while turning too quickly or changing directions too suddenly can result in a sprain or a strain. Over time, repeated movement can lead to wear and tear or osteoarthritis, a condition where the cartilage in joints wears down, making them stiff and painful. Other common issues include tendinitis, where tendons become inflamed from overuse, and bursitis, which happens when the small fluid-filled sacs that cushion joints become irritated.
Sometimes, what feels like a musculoskeletal issue might actually be something else! For example, sometimes pain you feel in your bones and muscles can actually come from another part of the body, like the heart or the kidneys [1]. That is why doctors use different imaging techniques, not just to look at bones and muscles, but also to rule out other conditions that might be causing pain (Figure 1).
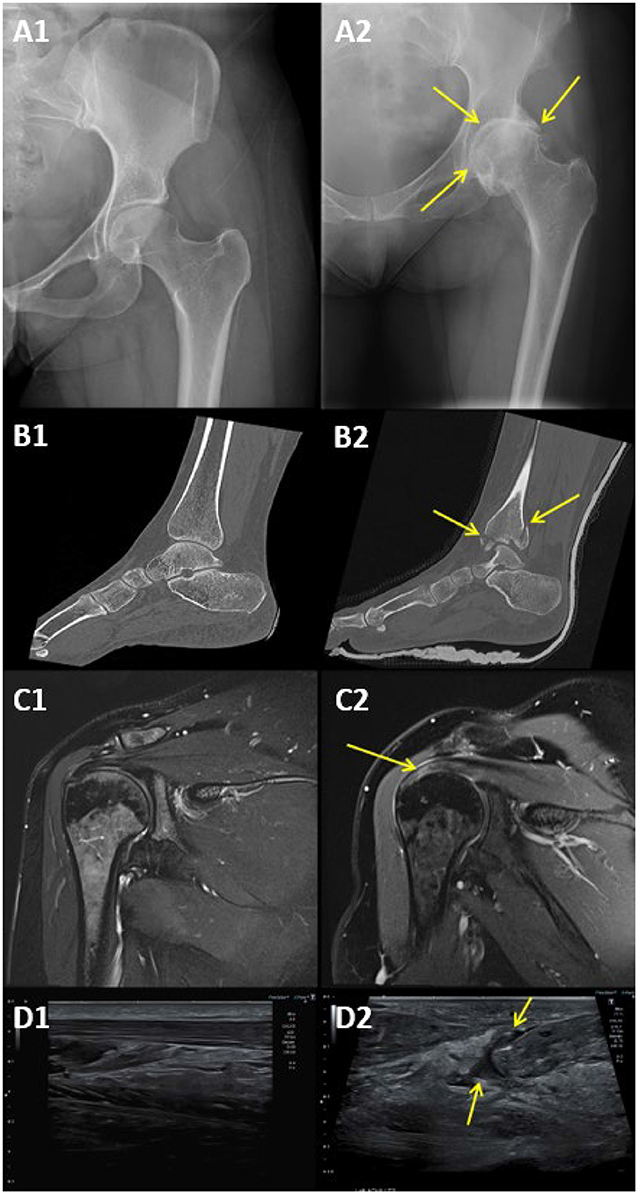
- Figure 1 - (A) X-ray of (A1) a healthy hip and (A2) hip osteoarthritis, pointed out by the yellow arrows.
- (B) CT of (B1) a healthy ankle and (B2) an ankle broken in multiple places, highlighted by yellow arrows. (C) MRI of (C1) a healthy shoulder and (C2) a shoulder with tendon degeneration, highlighted by the yellow arrow. (D) Ultrasound of a (D1) healthy Achilles tendon and (D2) a ruptured Achilles tendon, pointed out by the yellow arrows.
The Classic X-Ray and Its High-Tech Upgrade: CT Scans
Two pillars of imaging technology that are almost always great choices for looking at bones are X-rays and computed tomography (CT) scans. X-rays are one of the oldest and most common imaging tools in orthopedics, which is the branch of medicine that treats the musculoskeletal system. X-rays work by sending invisible rays into the body. Since bones are denser than muscles and other tissues, they absorb more rays. This creates a special image where bones appear white on the X-ray, while air and the soft tissues appear black or gray, allowing doctors to see what is happening inside! Doctors usually take a couple of X-rays from different sides to get a good look at the anatomy from all angles.
X-rays are great for detecting fractures, joint dislocations, and arthritis, but when more detail is needed, doctors use CT scans. CT scans use X-rays to take multiple pictures at different angles all around the body to form a 3D image of bones and joints. This is particularly helpful for complicated fractures, like fractures in the spine or big traumas, and it is also helpful for surgical planning. You might be wondering why we do not just use CT scans for everyone, then—great question! One of the main reasons doctors avoid CT scans is because they give the body a lot of radiation, which is a kind of invisible energy [2]. Some radiation, like light, is completely safe. But other types, like X-rays, can be harmful if you get too much, particularly at a young age.
Seeing Inside Joints With MRI
Magnetic resonance imaging, or MRI, is one of the best ways to see soft tissues like muscles, tendons, ligaments, and cartilage (Figure 2A). MRI is particularly useful for spotting problems like torn ligaments, tendinitis, and cartilage damage in joints. The MRI machine looks like a giant donut, and the patient lies down in the middle of the donut to get their pictures taken. Unlike X-rays or CT scans that give patients radiation, MRI uses powerful magnets to create detailed images. So, you can see why sometimes it is a safer option, especially for younger patients. The downside? MRI scans take a long time, sometimes up to an hour, and patients must stay very still the whole time, or the picture might turn out blurry. It also makes really loud noises, which some people may find uncomfortable. Also, since the magnet is so strong, MRI is not always safe for people with some metallic devices in their bodies, like some pacemakers for the heart.
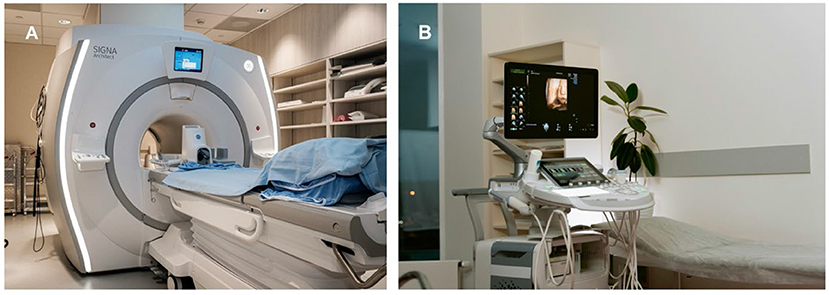
- Figure 2 - (A) An MRI machine.
- (B) An ultrasound machine.
Using Sound Waves: Ultrasound Imaging
Another great option doctors have to look at soft tissues like muscles, tendons, and ligaments is ultrasound (Figure 2B). Interestingly enough, the same ultrasound machine that is used to look at a baby inside a pregnant mother can also be used to diagnose problems with the musculoskeletal system. Ultrasound works by sending sound waves through a small, device called a transducer. The waves then pass through the body and bounce off different tissues to give a real-time image on the screen. Unlike X-rays or MRI, ultrasound can show movement in real time. This makes it especially useful for guiding injections of medications into joints to help with osteoarthritis and watching the movement of muscles, tendons, and joints. Ultrasound is also portable, quick, and does not use radiation. However, just like everything else, ultrasound has some limitations. One of the main issues with ultrasound is that it cannot see very well inside your joints because the sound waves bounce off bones instead of going through them. Also, the accuracy of the images depends on the skill of the person using it [3].
Imaging in Action: Bone Scans
Some conditions require more specialized imaging. A bone scan is like a detective tool for spotting bone problems that might not show up on regular X-rays. Instead of just taking a picture, a bone scan looks at how active the bone cells are. To do this, doctors inject a special liquid, called a radioactive tracer, into a vein in the patient’s arm. The radioactive tracer travels through the bloodstream and settles down in the bones. If there are areas in the bone where extra activity is happening, like a fracture that is healing or an infection, a larger amount of this tracer will go there. A special machine then takes pictures, and the areas with high activity are seen as bright spots on the final image. This helps doctors detect fractures, infections, or even tumors that might be hard to see with other imaging options.
Future Tools for Bone Detectives
The tools that bone detectives use are getting better and better. Scientists are creating new inventions to help doctors make more accurate diagnoses. One exciting new tool is artificial intelligence (AI). In the future, doctors will have AI to help them find problems with bones, muscles, and joints. Imagine a super-smart robot friend that helps solve mysteries about what is going wrong in your body. And the best part? This robot never gets tired and does not need any sleep! AI will help doctors look at X-rays, CT scans, MRIs, ultrasounds, and bone scans faster, more accurately, and with fewer mistakes. It works by looking at tons of pictures and learning what normal ones look like, so it can spot when something looks different. With AI on their team, doctors will be even better at spotting clues and solving the toughest bone mysteries!
The Big Picture
Seeing inside the human body without having to cut it open is one of medicine’s greatest achievements! When it comes to examining the musculoskeletal system, it is fascinating how much the medical field has grown and developed. Imaging is becoming faster, safer, and more detailed. Whether it is detecting fractures with an X-ray, diagnosing ligament tears with an MRI, or guiding treatments with ultrasound, modern imaging plays a crucial role in orthopedic care. To this day, there are many other strategies emerging. Keep an eye out to see how 3D printing is going to become more popular in treating bone deformities over the next couple years [4], and how AI is going to help doctors analyse images and detect problems more accurately [5]! With all these great options, doctors need to use their training and experience to pick the best technique for each patient. They must compare advantages and disadvantages, while balancing accuracy, safety, and efficiency (Table 1). Thanks to all this, doctors are better equipped than ever to diagnose and treat musculoskeletal conditions, and the future of medical imaging is only getting brighter!
| Imaging technique | Strengths | Limitations | Cost | Radiation level | Best used for |
|---|---|---|---|---|---|
| X-ray | Fast, excellent for bones | Poor for soft tissues | $ | + | Simple broken bones |
| CT Scan | High detail, great for complex fractures | High radiation exposure | $$$ | + ++ | Complex fractures (face, spine, pelvis) |
| MRI | Best for soft tissues like muscles, tendons, ligaments, and cartilage | Expensive, long scan time | $$$$ | None | Torn ligaments, spinal cord problems |
| Ultrasound | Real-time imaging, no radiation, portable | Limited for looking inside joints | $$ | None | Muscle tears, soft lumps |
| Bone scan | Detects the activity of bone cells | Requires radioactive tracer injection | $$$ | + + | Bone infections, tumors |
- Table 1 - A summary of the different imaging techniques used for the musculoskeletal system.
Glossary
Musculoskeletal System: ↑ The body’s framework of bones, muscles, joints, and tendons that work together to support movement, protect organs, and keep us upright.
Fracture: ↑ A broken bone. It can be a small crack or a complete break.
Sprain: ↑ An injury where a ligament (the tissue that connects bones) is stretched or torn.
Strain: ↑ An injury to a muscle or tendon (the tissue that connects muscle to bone) from stretching too much.
Orthopedics: ↑ A medical specialty that focuses on keeping the body’s skeleton, muscles, and joints healthy, so people can stand, walk, play, and move without pain.
Soft Tissues: ↑ The parts of the body like muscles, fat, tendons, and ligaments that surround and support our bones and organs.
Transducer: ↑ A device that turns sound waves into pictures during an ultrasound.
Artificial Intelligence: ↑ Computer technology that learns from information and makes decisions or predictions, similar to how people think and solve problems.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AI Tool Statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
[1] ↑ Jin, Q., Chang, Y., Lu, C., Chen, L., and Wang, Y. 2023. Referred pain: characteristics, possible mechanisms, and clinical management. Front. Neurol. 14:1104817. doi: 10.3389/fneur.2023.1104817
[2] ↑ Giordano, B. D., Grauer, J. N., Miller, C. P., Morgan, T. L., and Rechtine, G. R. 2nd. 2011. Radiation exposure issues in orthopaedics. J. Bone Joint Surg. Am. 93:e69. doi: 10.2106/jbjs.J.01328.
[3] ↑ Ohrndorf, S., Naumann, L., Grundey, J., Scheel, T., Scheel, A. K., Werner, C., et al. 2010. Is musculoskeletal ultrasonography an operator-dependent method or a fast and reliably teachable diagnostic tool? Interreader agreements of three ultrasonographers with different training levels. Int. J. Rheumatol. 2010:164518. doi: 10.1155/2010/164518
[4] ↑ Chagas-Neto, F. A., Monteiro, F. C. C., da Rocha, E. L., Gregio-Junior, E., and Nogueira-Barbosa, M. A. 2017. What radiologists need to know about 3D printing and its main applications in musculoskeletal imaging. Radiol. Bras. 50:135–6. doi: 10.1590/0100-3984.2015.0208
[5] ↑ Guermazi, A., Omoumi, P., Tordjman, M., Fritz, J., Kijowski, R., Regnard, N.-E., et al. 2024. How AI may transform musculoskeletal imaging. Radiology 310:e230764. doi: 10.1148/radiol.230764