Abstract
Proximal humerus fractures are a type of break of the upper bone of the arm that occurs near the shoulder. Because of special cartilage areas near the end of each bone called growth plates, kids have a remarkable ability to grow and heal their bones. In a study looking at proximal humerus fractures in kids 10–16 years old, doctors compared the outcomes of kids whose proximal humerus fractures were repaired with surgery with those who did not have surgery. We learned that by 6 months after the injury, there was no difference in pain, movement, function, or mood between kids who received surgery and those who did not. This is an exciting discovery that means in kids whose growth plates are still open, it is possible to avoid the risks associated with surgery and heal proximal humerus fractures without operating.
What is the Humerus and How Can it Break?
The humerus is the long bone that forms the upper part of the arm. A break, or fracture, of the humerus can happen anywhere from the part that connects at the shoulder down to the part that connects at the elbow. When a fracture happens near the shoulder, it is called a proximal humerus fracture. Proximal humerus fractures make up about 3% of fractures in kids [1]. Proximal humerus fractures can happen while doing activities like riding a horse, skiing, snowboarding, trampolining, or they can be caused by traffic accidents [2].
An X-ray of the broken arm can tell doctors if the humerus has moved out of place, which is called displacement, or if it is left at an angle instead of being straight, which is called angulation (Figure 1). Our study specifically looked at serious fractures that were displaced more than half the width of the bone and angled more than 30 degrees.
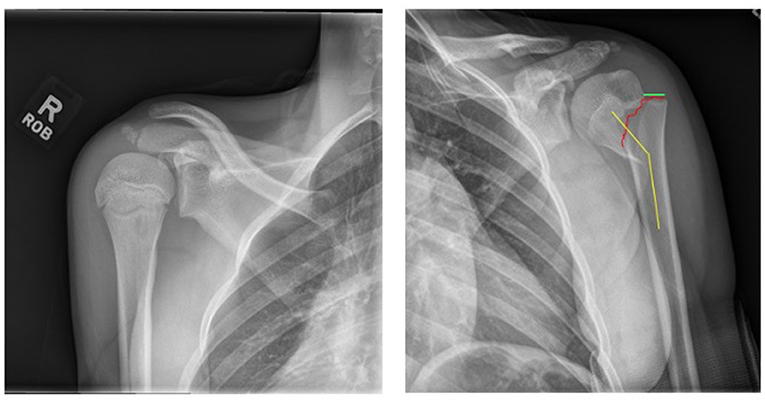
- Figure 1 - X-ray showing a non-injured shoulder on the left and a proximal humerus fracture (red line) on the right, with displacement (green) and angulation (yellow).
What is a Growth Plate?
Kids’ bones have special parts called growth plates. Growth plates are bone areas that are in charge of helping bones grow wider and longer as children get older. Growth plates also play an important role in repairing broken bones. Growth plates turn into a mature piece of bone when puberty ends, but kids have a special ability to heal and grow their bones while their growth plates are open. Up to 80% of the growth of the upper arm comes from the very powerful proximal humerus growth plate, which led some doctors to believe that fractures in this area may be able to heal and straighten themselves without surgery—better than some fractures in other parts of the body [3].
How Can Broken Arms Be Fixed?
When someone breaks a bone, there are different options for fixing it. The bone can be put back in place with or without surgery. To help keep the bone in place so it can heal, there are external options like casts, braces, and slings, as well as internal metal options like pins, plates, or screws. Most fractures in kids can be treated without surgery, but sometimes operations are required to put in metal pins, plates, or screws. Surgery has some rare but serious risks, like bleeding, damage to nerves or blood vessels, and scarring, so most kids and doctors prefer to avoid surgery if possible. However, there are not many studies telling us what the right treatment is in certain humerus fractures.
When doctors fix a broken bone with or without surgery, it is important to know how well the patient is recovering. Doctors check to see if a young patient has full movement (range of motion), if they have trouble using their arm (function), if they have pain or discomfort, or if they have mood changes because of their injury. Asking these questions helps the medical team understand how patients are being impacted by their injury.
Our Study
Between 2018 and 2022, six hospitals across the United States enrolled 10- to 16-year-olds who had proximal humerus fractures. The decision on how the patients were treated was made by the doctor, together with the patient and their family. More than half of the kids did not have surgery (54%). Some kids were treated with just a sling or cast, without pulling or pushing on the arm, and letting the bone heal itself. Others had a procedure called a reduction, where the doctors pushed the bone back in place but did not fix the bone with any metal. The remaining 46% of kids had surgery with either pins or plates and screws to hold the bone in place after it was reduced.
Patients came back to the doctor 6 weeks, 3 months, and 6 months after their injury. When they came back, they were assessed for movement, function, pain, and mood changes through surveys called PROMIS, QuickDASH, and SPADI. These surveys asked about specific things like how well the kids could use their arms for dressing, eating, and other daily activities, and how much pain interfered with these activities.
What Did the Study Find?
Patients who received surgery had similar outcomes to patients who did not receive surgery—the surveys showed kids had similar levels of pain, range of motion, mood changes, and function. At 6 weeks, the kids who had surgery had better PROMIS Upper Extremity survey scores, showing better use of their arms, but by the 3- and 6-month follow-up appointments, there was no difference between the two groups (Figure 2).
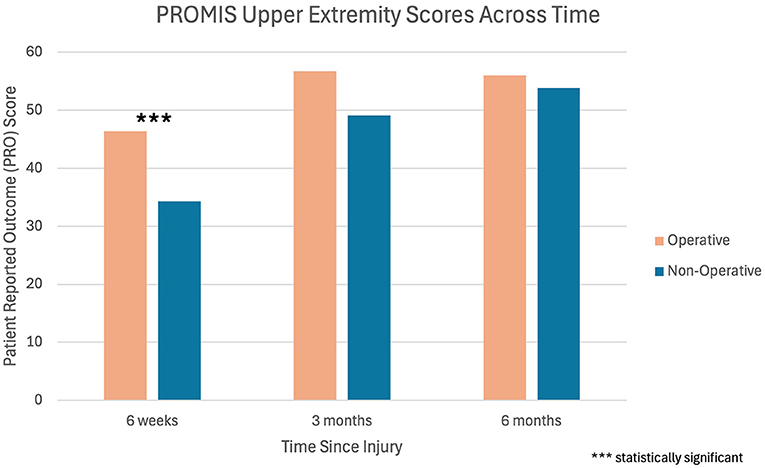
- Figure 2 - Survey results from PROMIS Upper Extremity scoring system at 6 weeks, 3 months, and 6 months after the proximal humerus fracture.
- Patients who received an operation had higher scores at 6 weeks, but the scores at 3 and 6 months were similar and not statistically different. This means that kids who had surgery did better initially, but by 3 months the kids who had surgery and those who did not were functioning the same. *** indicates statistical significance.
What About the Really Bad Fractures?
Some kids had very bad fractures in which the humerus was extremely displaced (>75%) or was very angulated (>40%). Sixty percent of the patients with severe fractures had surgery and 40% did not. The surveys showed that patients healed over time and had good movement in their arms by 3 months, whether they had surgery or not.
What did we Learn?
Six months after the proximal humerus fracture, there were no differences found between patients who received surgery and those that did not receive surgery. Because surgery can be risky and expensive, it is important to understand when surgery can be avoided. We now know that, due to the power of bone healing in kids with open growth plates, proximal humerus fractures in kids aged 10–16 can be treated without surgery. This can help guide doctors and their patients in making the best treatment decisions.
Glossary
Proximal Humerus Fracture: ↑ A break in the long bone of the upper arm that occurs close to the shoulder.
Displacement: ↑ The amount that a bone moves when it breaks, relative to its normal position; calculated using the width of the bone.
Angulation: ↑ The angle a bone creates when it breaks, relative to its normal straight position.
Growth Plate: ↑ A special area near the end of kids’ bones made of cartilage that is responsible for helping bones grow longer, wider, and recover after injury.
Range of Motion: ↑ How far a body part can move around a joint, like your knee or shoulder. It is measured in degrees and shows how much you can bend, stretch, or rotate that joint.
Reduction: ↑ A procedure where a doctor sets or straightens a broken bone to make it straighter.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AI Tool Statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Original Source Article
↑Hosseinzadeh, P., Torres-Izquierdo, B., Tippabhatla, A., Denning, J., Vidyadhar, U., Sanders, J., et al. 2024. Operative versus nonoperative treatment of displaced proximal humerus fractures in adolescents: results of a Prospective Multicenter Study. J. Pediatr. Orthop. 44:e823–9. doi: 10.1097/BPO.0000000000002755
References
[1] ↑ Peterson, C. A. and Peterson, H. A. 1972. Analysis of the incidence of injuries to the epiphyseal growth plate. J. Trauma. 12:275–81. doi: 10.1097/00005373-197204000-00002
[2] ↑ Hannonen, J., Hyvönen, H., Korhonen, L., Serlo, W., and Sinikumpu, J. J. 2019. The incidence and treatment trends of pediatric proximal humerus fractures. BMC Musculoskelet. Disord. 20:571. doi: 10.1186/s12891-019-2948-7
[3] ↑ Neer, C. S., and Horwitz, B. S. 1965. Fractures of the proximal humeral epiphyseal plate. Clin. Orthop. Relat. Res. 41:24–31.
