Abstract
Rare diseases are diseases that affect fewer than 1 in 2,000 people. Due to their rarity, it can be extremely challenging for doctors to diagnose these diseases in their patients—it often takes 6–8 years for some patients to get a diagnosis. Even though they are uncommon, rare diseases still have a significant impact on families and communities and need greater attention. Fatal familial insomnia (FFI) is a rare disease that affects the brain and gradually reduces a person’s ability to sleep. FFI gets worse over time and causes severe complications. There is currently no cure for FFI, so more research is crucial—not only for understanding FFI but also for unlocking potential treatments for other rare diseases. Rare disease research brings hope for a better future to those living with FFI and other rare conditions.
Why are Rare Diseases Important?
Rare diseases are diseases that affect only a small portion of the world’s population, generally fewer than 1 in 2,000 people. Due to the small number of people affected by each rare disease and the limited amount of information available, it can be very difficult for doctors to identify (diagnose) a rare disease—almost like solving a complex puzzle. It can frequently take between 6–8 years for patients to receive the right diagnosis, which can be a very long and frustrating experience for patients and their families. Although each rare disease affects only a small number of people, over 6,000 rare diseases have been identified—so all together these diseases are a major burden for many patients and their families. Thus, research to understand, diagnose, and treat rare diseases is critical, as is finding ways to support people living with these conditions.
What is Fatal Familial Insomnia?
In the mid-1980s, a family with a mysterious problem lived in a small town in Italy. For many years, members of this family had trouble sleeping, but no one knew why. One day, a family member named Silvano decided to find out what was causing this strange problem. Silvano traveled to the city of Bologna to meet with the best sleep doctors. He told them all about his family’s mystery.
The doctors were intrigued by Silvano’s story and immediately began to study his case. After much research, the doctors discovered something never seen before: a tiny change in a special gene passed down from generation to generation in Silvano’s family, which stopped them from sleeping. They called this disease fatal familial insomnia (FFI).
Fatal familial insomnia is an extremely rare disease. Like many other rare diseases, FFI is passed on through the DNA from parents to their children. The symptoms of FFI start slowly and get worse over time. People with FFI start to have difficulty falling and/or staying asleep, and then, as it gets worse, they may suddenly fall asleep without warning. People with FFI also tend to develop other problems like a fast heartbeat; high blood pressure; hormonal, mood and behavior swings; anxiety; excessive sweating; and trouble thinking clearly and moving their bodies [1]. The symptoms usually start between the ages of 51 and 60, although rarely they can start as early as 18–20 years old. FFI affects both men and women equally. To date, more than 70 families around the world have been found to have FFI [2].
What Causes FFI?
FFI is caused by prions. Unlike most infectious diseases, which are typically caused by bacteria or viruses, prions are proteins that do not contain genetic material. They have the unique ability to reproduce on their own and become infectious. Cells normally contain healthy prion proteins called PrPC. The diseased form, called PrPSc interacts with normal prion protein and causes them to take on the incorrect shape of PRPSc, leading to prion disease. Some prion diseases can develop without any known reason, some (like FFI) are due to genes that are passed on across generations, and some can be “caught” like other infectious diseases.
As we just mentioned, FFI is a genetic prion disease, caused by a mutation in the prion gene (called PRNP) that is normally responsible for producing the healthy prion protein PrPC. When the PRNP gene is mutated, it stops producing the healthy form of the prion protein and instead produces PrPSc [3]. This abnormal prion protein accumulates in the brain and eventually destroys brain cells called neurons, leaving holes in the brain where neurons used to be. Because of this, prion diseases like FFI cause a gradual and permanent loss of thinking and movement abilities.
Certain brain areas are more affected by FFI than others. The thalamus, which plays a key role in regulating sleep, is the most affected area [3]. When abnormal prion proteins accumulate in the thalamus, they disrupt its ability to regulate the sleep-wake cycle, which is why FFI patients have trouble sleeping (Figure 1).
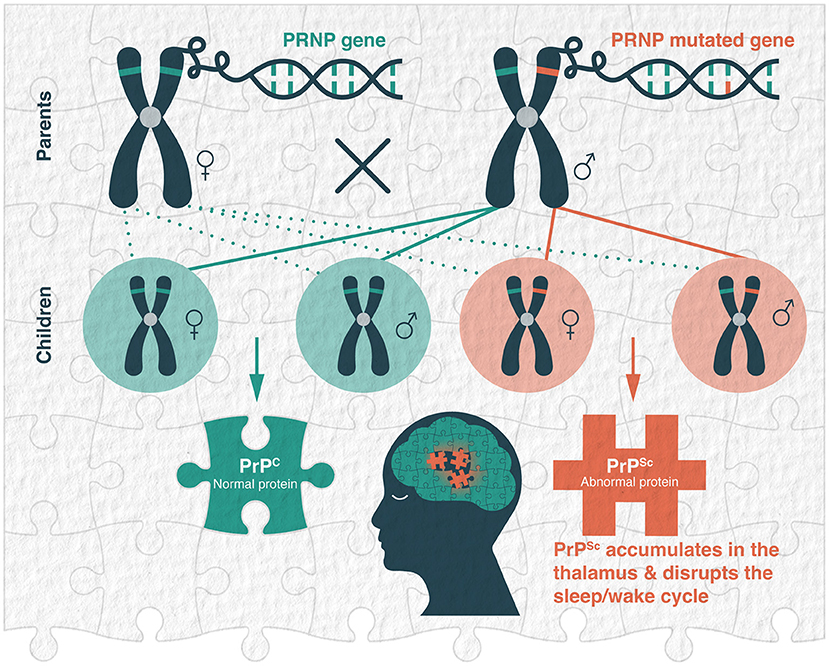
- Figure 1 - The genetic basis of fatal familial insomnia.
- FFI is caused by a change in a gene called PRNP, which causes the body to make an incorrect protein called PrPSc instead of the normal cellular prion protein PrPC. If one parent has the genetic change that causes PrPSc, their children have a 50% chance of inheriting it. When a person has this change, the incorrect protein builds up in the brain, initially in a region called the thalamus, which makes the person unable to sleep.
How is FFI Inherited?
FFI is an autosomal dominant disease. Humans have 23 pairs of chromosomes (one pair received from each parent): 22 pairs of autosomal chromosomes and one pair of sex chromosomes. When a disease is autosomal, the defective gene is on one of the non-sex chromosomes, so it affects both sexes equally. The word “dominant” means that only one copy of the defective gene is enough to cause the disease. Therefore, when a disease is autosomal dominant, there is a 50% chance that a child will be affected by the disease if one of the parents carries the altered gene. This is because the child’s chances of inheriting either the normal copy of the gene or the defective copy are each 50% (Figure 1).
Is There a Treatment Or Cure for FFI?
There is currently no cure for FFI, as is the case for most rare diseases [4]. Disease care varies for each person based on their specific symptoms, and treatment involves various health professionals. Psychological and emotional support for patients and their families is crucial. Medications can relieve the symptoms, and physiotherapy can help with some movement-related problems. Genetic counseling is recommended for affected individuals and their families for three reasons. First genetic counselors can explain the genetic nature of the disease. They can also assess a person’s likelihood of developing the disease, which can help people make informed decisions about family planning and medical care. Finally, genetic counseling can offer guidance on the available genetic testing options, including their benefits and risks.
Why is it Important to Study FFI?
Although there is still no cure for FFI, research is happening all over the world. Researchers are working to find new pieces to help them solve the complex puzzle of FFI and to develop treatments that can improve the lives of those affected (Figure 2) [4]. Ongoing research aims to understand the underlying mechanisms of FFI, especially how genetic mutations change healthy prion proteins into abnormal ones and how the buildup of abnormal prions in the brain causes FFI symptoms. This understanding is essential for developing effective therapies.
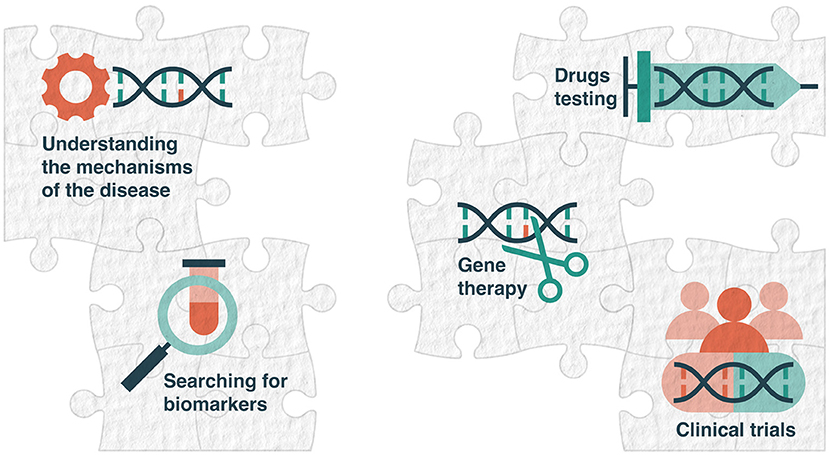
- Figure 2 - Piecing together the puzzle of fatal familial insomnia.
- Although there is still no cure for FFI, researchers are working to find new pieces to solve this complex puzzle and to develop treatments that can improve the lives of those affected. The strategies include understanding the underlying mechanisms of the disease; searching for biomarkers of FFI; developing therapies, particularly gene therapy; and testing potential drugs, both in animals and in human patients.
Additionally, researchers are searching for biomarkers of FFI. Biomarkers are things that can be measured through blood tests or brain scans, for example, that indicate the presence of a disease or the risk of developing it. Biomarkers could help doctors to diagnose FFI earlier and to track how it changes over time.
In terms of developing therapies for FFI, gene therapy is a promising approach that aims to fix or replace defective genes. Gene therapy could eventually improve patients’ quality of life. Researchers are also studying drugs that might stop or slow down the buildup of PrPSc in the brain. New drugs are first tested on animals to see if they work and are safe, and drugs that pass these initial tests are then tested on people. With effective new medicines, it might be possible to slow down or even stop FFI.
Getting the Pieces Together
FFI is a good example of why it is so important to study and understand rare diseases. FFI prevents people from sleeping and affects their lives in many ways. Although there is still no cure, scientific advances in several fields are helping researchers find the right pieces of the puzzle to enhance their understanding of FFI and help develop treatment options to improve the lives of patients and their families.
Thanks to the joint efforts of doctors, researchers, patient organizations, and companies that make medicines, the search for FFI treatments continues. Everyone deserves a chance for a better life. We believe that future research progress will lead to better treatments, not only for FFI but also for other rare diseases, thus offering a brighter future for everyone affected by these challenging conditions.
Glossary
Genes: ↑ Portions of DNA that contain instructions (genetic code) to produce proteins.
Prions: ↑ Infectious proteins capable of causing brain diseases in various species, including humans.
Thalamus: ↑ An egg-shaped structure in the middle of the brain that acts as a relay station, passing movement and sensory information (except smell) from the body to other brain areas.
Autosomal Dominant Disease: ↑ A genetic condition in which inheriting a faulty gene from just one parent causes the disease. Each child has a 50% chance of inheriting it, regardless of gender.
Genetic Counseling: ↑ A special doctor helps people understand how traits and diseases can be passed from parents to children, and what that means for their health and choices.
Biomarker: ↑ A sign in the body that indicates whether people are healthy or if they might have a disease. Biomarkers can be found in blood, saliva, or brain scans, for example.
Gene Therapy: ↑ A special medical treatment that add or fix genes in the cells to help it work better and fight certain illnesses.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was financed by the European Regional Development Fund (ERDF), through Centro 2020 Regional Operational Programme COMPETE 2020 - Operational Programme for Competitiveness and Internationalization and Portuguese national funds via Fundação para a Ciência e a Tecnologia (FCT; UIDB/04539/2020, UIDP/04539/2020, and LA/P/0058/2020), and the European Social Fund through the Human Capital Operational Programme and Portuguese national funds via FCT under 2020.04499. BD, PD/BD/135497/2018, 2020.04850.BD, 2021.05334.BD, and under COVID/BD/152507/2022. This work was supported by Mapfre, with the project “InsomniaO’clock”- reference IT137-24-400. This work was supported by FCT - Fundação para a Ciência e Tecnologia, I.P. by project 2021.05334.BD and DOI identifier https://doi.org/10.54499/2021.05334.BD.
References
[1] ↑ Khan, Z., and Bollu, P. C. 2024. “Fatal familial insomnia”, in StatPearls (Treasure Island (FL): StatPearls Publishing). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK482208/ (accessed February 13, 2024).
[2] ↑ Baldelli, L., and Provini, F. 2019. Fatal familial insomnia and Agrypnia Excitata: autonomic dysfunctions and pathophysiological implications. Auton. Neurosci. 218:68–86. doi: 10.1016/j.autneu.2019.02.007
[3] ↑ Lindsley, C. W. 2017. Genetic and rare disease of the CNS. Part I: fatal familial insomnia (FFI). ACS Chem. Neurosci. 8:2570–2572. doi: 10.1021/acschemneuro.7b00463
[4] ↑ Genetics and Rare Diseases Information Center. 2023. Fatal familial insomnia. Available online at: https://rarediseases.info.nih.gov/diseases/6429/fatal-familial-insomnia (accessed February 13, 2024).
