Abstract
Antibiotics, important medicines that fight harmful bacteria, face a big problem: bacteria are becoming increasingly resistant. This means that bacteria are changing in ways that antibiotics designed to kill them do not cause any harm anymore. Once only a concern in hospitals, antibiotic-resistance has reached Earth’s coldest places, like glaciers and the Arctic. This article explores how bacteria in these icy places learned to withstand antibiotics and how human activities, like tourism, worsen the problem. Join us on a fascinating journey into the ice, to understand how antibiotic-resistance spreads in these faraway places, how strong these bacteria can be, and how human behavior can play a role in bacterial antibiotic-resistance in icy locations. Together, we will find ways to keep antibiotics working well, to protect people’s health everywhere.
Shaping Antibiotic Resistance: Human Influence in Earth’s Coldest Realms
Have you heard of antibiotics? They are powerful medicines that help us fight harmful bacteria that can cause infections. Chances are, at some point in your life, your doctor may have prescribed antibiotics to help you recover from an illness caused by these microscopic single-celled organisms. While most bacteria are harmless and some can actually help our bodies perform important tasks like digesting food, some bacteria can cause serious diseases like pneumonia and need to be treated with antibiotics. Antibiotics come in two main types: natural and synthetic. Natural antibiotics, like penicillin, are produced by living organisms such as fungi and bacteria, which use them as a defense mechanism or natural advantage in the competition against other bacteria for food. Synthetic antibiotics are created in laboratories to mimic or enhance the effects of natural ones.
Antibiotics have saved millions of lives, but sometimes they fail. This happens when bacteria develop antibiotic-resistance (to learn more, check out this Frontiers for Young Minds article). Resistant bacteria have evolved ways to withstand antibiotics, which makes treatments less effective. Scientists are currently worried about the increasing frequency of cases in which antibiotics no longer work. But the problem might be even more serious than researchers thought.
For a long time, experts believed that antibiotic-resistance only happens in places where antibiotics are used to treat infections. However, scientists have found traces of antibiotic- resistant microbes in remote locations like the North and South Poles [1, 2], even though were long considered environments where bacteria cannot grow.
The North and South Poles are part of the so-called cryosphere, which means “cold globe” in Greek and includes all areas on Earth where water exists in its solid form as snow or ice. Humans generally consider these regions as harsh to live in. However, some microorganisms adapted to the extreme conditions, such as low temperatures, no or too much sunlight (depending on whether it is polar night or day), and very low food availability. The discovery that some bacteria in the cryosphere developed resistance to antibiotics was unexpected. Scientists still do not know how these microbes learned to withstand the harmful effects of antibiotics, and they are still trying to understand the extent of the problem.
How Bacteria Become Resistant to Antibiotics
There are several ways bacteria can become resistant to antibiotics. Some are nonspecific defense strategies, meaning they protect the bacterial cell from all sorts of harmful substances. An example for these nonspecific defense strategies are molecular “pumps” that remove antibiotics and other threats from the bacterial cell (Figure 1).
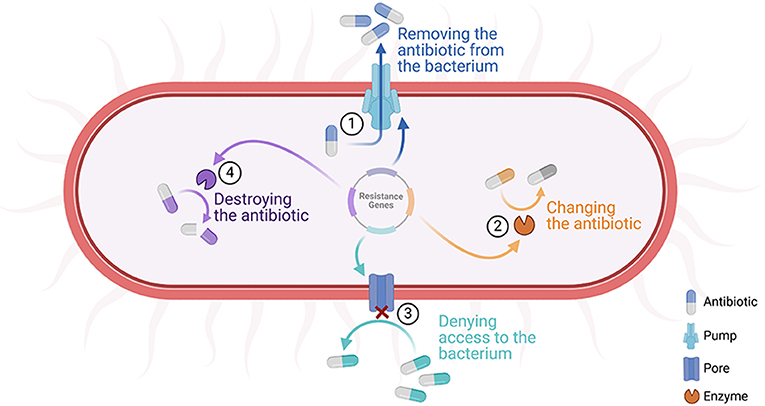
- Figure 1 - Possible defensive strategies that help bacteria to withstand antibiotics.
- Some of the main mechanisms include: (1) pumping out the toxic substance; (2) changing the antibiotic into a harmless substance; (3) preventing the harmful molecule from entering the cell; and (4) destroying the antibiotic (created with BioRender.com).
In contrast to nonspecific defense strategies, specific defensive strategies usually only develop when bacteria are exposed to antibiotics in their environment. This can also be the case in the cryosphere. Additionally, microorganisms, including antibiotic-resistant bacteria, can be transported by animals (e.g., migrating birds), global winds (think about how Saharan dust can travel over the sea to other continents), and humans (e.g., travelers) [3]. All these factors combine to create what is called the cryospheric resistome—the sum of all antibiotic-resistance mechanisms within snow and ice habitats. Scientists have already shown that the transport of antibiotic-resistant bacteria from other areas of the Earth is one of the reasons for the presence of antibiotic-resistance in the cryosphere [4].
Human Impact on Antibiotic-Resistance in Earth’s Coldest Regions
Now, let us think about how human activities can shape the cryospheric resistome. Imagine that bacteria living in snow and ice could resist not just one or two but up to eight different antibiotics! That is what we discovered in our study across multiple cryospheric spots in the Alps. We looked at snow and ice samples with varying levels of human presence. Interestingly, we found that humans play a major role in antibiotic-resistance in cold areas, especially when these regions are easily accessible. For example, the Nature Ice Palace, a popular ice cave on top of an Austrian mountain with many daily visitors, showed some of the highest levels of antibiotic-resistance in all of our samples. Here, we found that 20 out of 21 bacterial isolates were resistant to more than 3 antibiotics, which makes them multi-resistant. In contrast, at the comparatively remote Jamtal Glacier in the Austrian Alps, only about half of the microorganisms were multi-resistant.
In addition, even powerful antibiotics like vancomycin and linezolid, which are often used to treat sick people when other antibiotics fail, could fight only very few of the microbes present in the ice cave. In fact, the number of vancomycin-resistant bacteria in the Nature Ice Palace was higher than what scientists found in some hospitals [5]! Again, bacteria at the Jamtal glacier, which can only be reached by a long hike, also had some resistance to these so-called “drugs of last resort”, but the number was nowhere close to that of the popular ice cave.
We found this trend to be true in all of the almost 300 samples we collected from glaciers, lakes, or seasonal snow on top of some remote mountains, as well as plowed snow from city roadsides. All the samples had one thing in common: the higher the human activity, the higher the number of antibiotic-resistant bacteria. This trend was also evident in the number of bacteria with resistance against synthetic antibiotics. Synthetic antibiotics are usually a good indicator of antibiotic-resistance caused by human (mis)use. Humans can introduce potentially antibiotic-resistant bacteria into the environment by simple actions such as breathing or having skin contact with the ice. And as you might know, humans like to touch what they see, which is also true for beautiful ice features. Together with our results, these interactions highlight that human activities are likely one of the main reasons for the spread of resistant bacteria in unexpected environments like the cryosphere.
Exploring the Secrets of the Toughest Bacteria in Cold Areas
If we take a look at some truly remote areas—far from cities, hospitals, animal farms, or busy ski resorts—the cryospheric resistome appears different. First and foremost, antibiotic-resistant bacteria are less common in these regions. However, the fact that quite a few microbes could withstand many of the tested antibiotics was surprising. While synthetic antibiotics were more effective in remote areas like Jamtal Glacier, other antibiotics could only eliminate 2–5 out of 10 bacteria tested. Fortunately, these organisms do not pose an immediate threat to human health.
One possible explanation for the toughness of these bacteria could be their unique adaptations. Bacteria living under harsh conditions must adapt and may, for example, develop thicker cell walls to survive in cold environments. Such adaptations could also help them resist antibiotics.
Furthermore, like all other bacteria, bacteria in the cryosphere are competing for food, and might have developed protection against other organisms that are potential antibiotic producers. Finally, as previously mentioned, bacteria can travel via a variety of mechanisms (Figure 2), further spreading resistance around the globe.
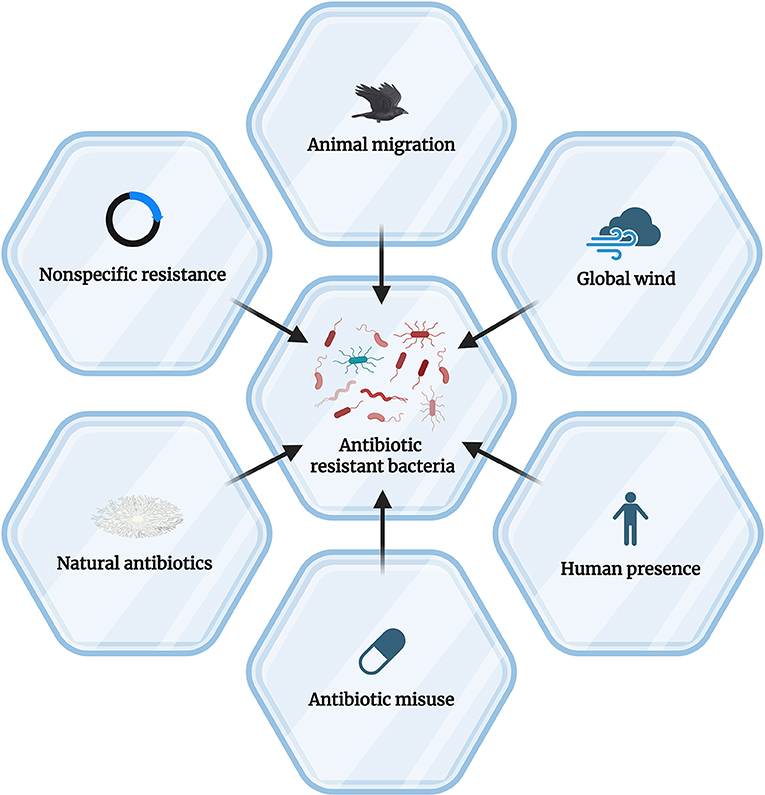
- Figure 2 - How bacteria living in snow and ice can become resistant to antibiotics.
- The main causes include nonspecific resistance mechanisms like pumps, the presence of antibacterial substances in cryosphere regions, and various transport pathways leading to the distribution of antibiotic-resistant bacteria into remote areas (created with BioRender.com).
One thing is clear: we need much more research to understand the cryospheric resistome better. During summer seasons (and increasingly, as global temperatures keep rising), melting ice and snow can release bacteria from the cryosphere into human environments through meltwater (Figure 3). Although they are not a direct threat to humans, these bacteria can potentially teach other bacteria how to survive antibiotics and thus increase the global antibiotic-resistance crisis. Therefore, it is important to continue studying resistant bacteria in all parts of the world, to stay one step ahead.
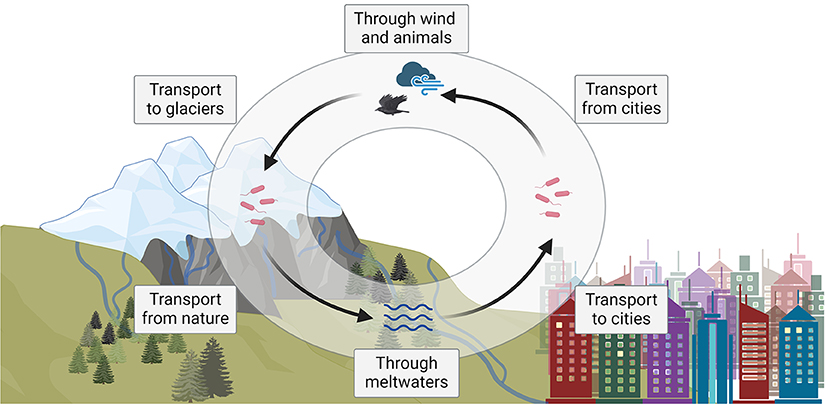
- Figure 3 - The potential cycle of antibiotic-resistant bacteria between cities and the environment (e.g., glaciers) (created with BioRender.com).
All in all, human activity can shape the resistome even in seemingly remote regions like the cryosphere. Our study provided some insight into this topic, but many questions remain. Continued research is essential to understand the full scope of the problem of antibiotic-resistance. And while science is doing its best to find out more, you can already make a small difference today! By using antibiotics responsibly, meaning only when and as prescribed by your doctor, and by spreading awareness about this topic, you can help scientists to stay one step ahead of the antibiotic-resistant bacteria and ensure that our valuable medicines remain effective.
If you want to learn more about antibiotic-resistance, check out our website, where you can explore our blog and our interactive map with real data from this study to learn more about antibiotic-resistant bacteria.
Glossary
Antibiotics: ↑ Medicines that help our bodies fight harmful bacteria and get rid of infections.
Bacteria: ↑ Tiny organisms that can only be seen under a microscope. Some are helpful, but others can cause diseases.
Antibiotic-resistance: ↑ When bacteria change in a way that makes antibiotics no longer able to kill them.
Cryosphere: ↑ The parts of Earth where water exists in solid form, like snow and ice (e.g., the North and South Poles).
Cryospheric Resistome: ↑ The sum of all antibiotic-resistance mechanisms within the cryosphere.
Multi-resistant: ↑ Describes bacteria that have become resistant to at least 3 different antibiotics.
Adaptations: ↑ Special features or behaviors that help organisms survive better in their environment.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Funding derived by Colonel (IL) J. N. Pritzker, IL ARNG (retired), of the Tawani Foundation by the projects BIO.CRYO and ANTHROPO.SNOW. DG was funded by the University of Innsbruck by a Doctoral Scholarship for 12 months. This research was supported by the Autonomous Province of Trento (Accordo di Programma P2211003I to TW).
AI Tool Statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Original Source Article
↑Gattinger, D., Schlenz, V., Weil, T., and Sattler, B. 2024. From remote to urbanized: dispersal of antibiotic-resistant bacteria under the aspect of anthropogenic influence. Sci. Total Environ. 924:171532. doi: 10.1016/j.scitotenv.2024.171532
References
[1] ↑ McCann, C. M., Christgen, B., Roberts, J. A., Su, J.-Q., Arnold, K. E., Gray, N. D., et al. 2019. Understanding drivers of antibiotic resistance genes in high Arctic soil ecosystems. Environ Int. 125:497–504. doi: 10.1016/j.envint.2019.01.034
[2] ↑ Hwengwere, K., Paramel Nair, H., Hughes, K. A., Peck, L. S., Clark, M. S., and Walker, C. A. 2022. Antimicrobial resistance in Antarctica: is it still a pristine environment? Microbiome 10:71 doi: 10.1186/s40168-022-01250-x
[3] ↑ Allen, H. K., Donato, J., Wang, H. H., Cloud-Hansen, K. A., Davies, J., and Handelsman, J. 2010. Call of the wild: antibiotic resistance genes in natural environments. Nat. Rev. Microbiol. 8:251–9. doi: 10.1038/nrmicro2312
[4] ↑ Ly, Y. T., Leuko, S., and Moeller, R. 2024. An overview of the bacterial microbiome of public transportation systems-risks, detection, and countermeasures. Front. Public Health. 12:1367324. doi: 10.3389/fpubh.2024.1367324
[5] ↑ Rodriguez-Mozaz, S., Chamorro, S., Marti, E., Huerta, B., Gros, M., Sànchez-Melsió, A., et al. 2015. Occurrence of antibiotics and antibiotic resistance genes in hospital and urban wastewaters and their impact on the receiving river. Water Res. 69:234–42. doi: 10.1016/j.watres.2014.11.021