Abstract
On a scale of 1–10, imagine a headache turned up to 10. That is a migraine, caused by intricate changes in the brain’s nerves and chemicals. Despite affecting 15% of the population, the exact cause of migraines remains a puzzle, with genetic, environmental, and hormonal factors all at play. Migraines unfold in four phases: prodrome, aura, headache, and postdrome, each with its distinct symptoms and challenges. Delving into the brain’s workings during a migraine, scientists have discovered a complex interplay between various aspects of the nervous system. Far beyond mere headaches, migraines are an intense experience. For people grappling with migraines, treatment options can range from medications to lifestyle adjustments. Treatment options depend on the person and the type of migraine they have. Fortunately, migraine treatments are constantly improving. So, the next time your headache feels like it might be more than a “regular” headache, consider the possibility of a migraine.
What is a Migraine?
Have you ever experienced a pounding headache and wondered if there is more to it than meets the eye? Well, sometimes there is. Some headaches are not just “regular” headaches—they might be migraines. Migraines are like super headaches caused by changes in the brain’s nerves and chemicals. When these brain pathways change during a migraine, they send signals for serious pain, causing the symptoms of a migraine. Migraines are not just about head pain. They can also cause nausea, dizziness, sensitivity to light, and tiredness. Believe it or not, around 15% of people experience migraines, and there are several types, which makes diagnosing and treating them quite complicated [1]. Knowing exactly which type of migraine a person has can help the doctor figure out how to tackle the pain.
The underlying cause of migraines is still a bit of a mystery, but here is what scientists say so far—migraines result from a combination of a person’s genes, their surroundings, and chemicals in the brain. For instance, if someone in your family has migraines, you are three times more likely to have them, too [1]. Because migraines are influenced by both genes and the environment, they are a complex disease—like a puzzle with lots of pieces. It is not just one thing causing the trouble—it is a whole bunch of factors teaming up. Not only are genes and the environment causing migraines, but hormones, the body’s chemical messengers, can cause them, too. Changes in female hormones can increase the chances of migraine attacks. Females, on average, are more likely to be treated for migraines compared to men [1]. But if you are female, do not worry—as females get older, these hormone-related changes tend to be less of a problem.
Migraine Attack
Migraines have four main phases, kind of like a rollercoaster: they are called prodrome, aura, headache, and postdrome [2]. But a person does not have to go through all four phases to have a migraine (Figure 1) [2].
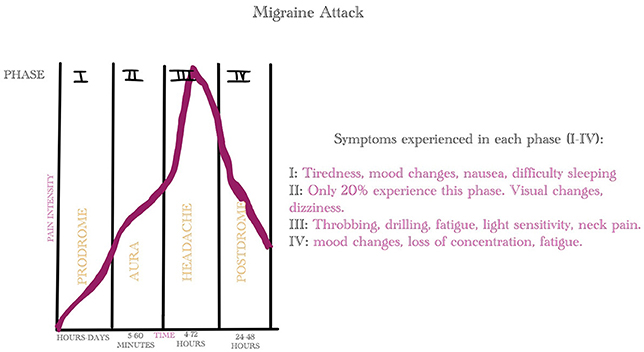
- Figure 1 - Migraine attacks have four phases: prodrome, aura, headache, and postdrome.
- Not every migraine sufferer goes through all four phases. The graph shows how the pain develops across the four phases of a migraine. Made by Mary Atkisson on GoodNotes.
First up is the prodrome phase. This is the starting point of a migraine attack, and it can be triggered by various things. Triggers are the keys to starting a migraine (Figure 2). These triggers are unique to each person, but most of them are related to how we live our lives. Things like stress, lack of sleep, too much caffeine or alcohol, and other things people eat or drink can be triggers. These triggers kickstart the first phase of a migraine attack. During the prodrome phase, migraine sufferers start feeling tired, moody, a bit down, have trouble focusing, or even get a sore neck. These symptoms can pop up hours to days before the classic migraine symptoms begin.
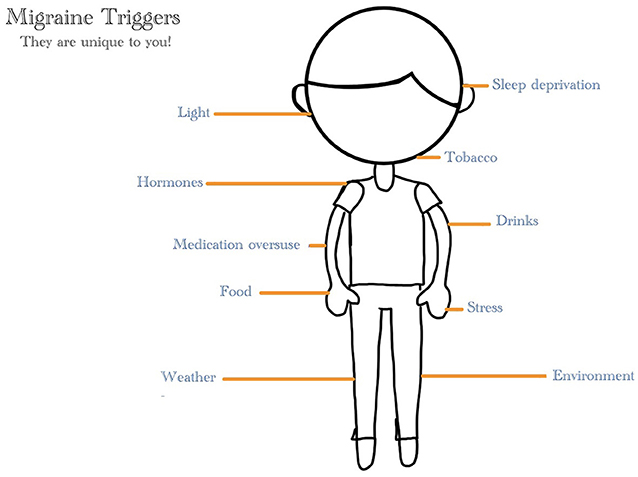
- Figure 2 - There are a number of things in a person’s body and environment that can lead to a migraine attack.
- These things are called triggers. They include certain behaviors as well as hormones and things people eat or drink. Made by Mary Atkisson on GoodNotes.
Next is the aura phase, which only happens in about 20% of people with migraines [2]. Auras are sensory symptoms that kick in about an hour before the headache phase and can mess with the migraine sufferer’s vision or even make a person temporarily lose their vision.
The third phase is the headache itself, and it can last anywhere from 4 to 72 h [2]. This is where the classic migraine symptoms come in—a throbbing, drilling pain in the head. Ouch!
Finally, people reach the postdrome, also known as the "migraine hangover” [3]. It is the body’s way of recovering from the intense headache and pain. During this phase, a person might feel tired, they might experience mood swings, and it might be tough for them to stay focused. A migraine attack can stick around for days, and that can really hurt a person’s lifestyle. Some people take days to recover, and people who have chronic migraines—frequently recurring migraines—can get stuck in a loop of constant migraine attacks. So, as you can see, migraines are not just headaches—they are so much more.
How a Migraine Works
What happens to the brain during a migraine attack? In simple terms, the body has a boss called the nervous system, which has two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS contains the brain, which is like the body’s headquarters, while the PNS is like the messenger of the CNS, sending signals to other parts of the body. During a migraine, changes in normal brain activity in the CNS and the PNS lead to a migraine attack. However, scientists are still trying to work out exactly what brain changes cause migraines.
Scientists originally believed that blood vessels were the culprit. Imagine the blood vessels as highways in the brain that sometimes act up. Scientists thought maybe these highways got too big and had too much blood “traffic”, which led to a migraine. But recent research found out there is more to the story than just blood vessels. There is also something called cortical spreading depression, which is like a slow wave of abnormal brain activity. Cortical spreading depression messes with how the brain talks to itself and changes the normal blood flow, causing the aura phase of migraines [4]. This wave of brain activity also causes the release of certain chemicals, like the hormone serotonin, which messes with blood vessels and can make them get bigger or inflamed.
There is one more important piece of the migraine puzzle: the trigeminovascular system. Think of this as a team of messengers, led by the trigeminal nerve, which is responsible for transmitting sensations to the brain from the head and face. When a migraine hits, the trigeminal nerve releases signals that cause swelling and pain in the brain (Figure 3). This swelling is particularly felt in the protective membranes around the brain, contributing to the throbbing sensation that characterizes a migraine headache [4].
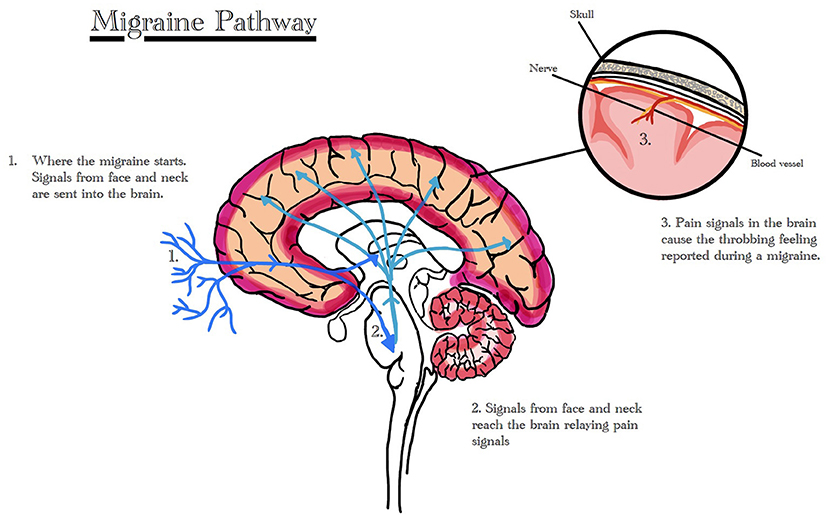
- Figure 3 - Scientists believe that, at least in some cases, the trigeminovascular system contributes to migraines.
- This team of messengers is led by the trigeminal nerve, which carries signals from the head and face to the brain. When these pain signals reach the brain, they cause the throbbing pain characteristic of a migraine. Made by Mary Atkisson on GoodNotes.
Treatment Options for Migraines
Once a person finds out they have a migraine, what comes next? There are several ways to treat migraines, like taking medicines, making lifestyle changes, or using natural remedies. Doctors prescribe medicines based on the specific type of migraines and how often a person gets them. If the triggers that cause migraines are known, doctors might suggest preventative therapy, which involves making lifestyle changes to avoid those triggers. This could mean reducing foods or drinks that serve as triggers, keeping an eye on how much water and caffeine are consumed, or adjusting the amount of exercise a person gets. About 40% of people who get migraines might need to try preventive therapy [5].
If the migraines still do not go away, there are other things to try. Some people use special devices called neuromodulation devices that help stop the pain signals in the nerves during a migraine attack [5]. And for those who do not want to use regular medicines, some doctors recommend natural supplements to help with migraines, especially if medicines cause unwanted side effects. Overall, migraine treatments continue to be improved as more people are needing preventative treatment.
Take Home Message…
So, the next time your head is throbbing a bit too much, pay attention and remember that it might not just be an ordinary headache—it could be a migraine attack. If you do have migraines, understanding what they are will help you to find the best way to manage them.
Glossary
Triggers: ↑ Something that starts a migraine attack, like lack of sleep or stress.
Central Nervous System: ↑ The body’s main control center, consisting of the brain and spinal cord.
Peripheral Nervous System: ↑ The network of nerves outside the brain and spinal cord that sends messages between the central nervous system and the rest of the body.
Cortical Spreading Depression: ↑ A slow wave of abnormal brain activity associated with auras in migraines.
Serotonin: ↑ A hormone that modulates sleep, eating, moods, and body temperature.
Trigeminovascular System: ↑ A network of nerves led by the trigeminal nerve, sending the brain sensations from the head and face.
Preventative Therapy: ↑ Preventative treatment works to prevent a migraine from starting. Rather than treating the migraine during an episode, treatment is given prior.
Neuromodulation Device: ↑ A device that acts directly on the nervous system to decrease pain.
Preventative Treatment: ↑ Something that stops a migraine attack from starting in the first place.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Authors would like to thank the young reviewer Chenxi for aiding in the editing of this article.
References
[1] ↑ Amiri, P., Kazeminasab, S., Nejadghaderi, S. A., Mohammadinasab, R., Pourfathi, H., Araj-Khodaei, M., et al. 2022. Migraine: a review on its history, global epidemiology, risk factors, and comorbidities. Front. Neurol. 12:800605. doi: 10.3389/fneur.2021.800605
[2] ↑ Davis, L. L., and Torphy, B. 2022. Managing migraine on the frontline: Identifying disease, understanding burden, and incorporating CGRP pathway-targeting therapies in primary care. Br. J. Pain. 16:560–73. doi: 10.1177/20494637221104292
[3] ↑ Ruschel, M. P. 2020. “Migraine headache”, in StatPearls - NCBI Bookshelf. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK560787/ (accessed August 23, 2023).
[4] ↑ Jenkins, B. 2020. Migraine management. Aust. Prescr. 43:148–51. doi: 10.18773/austprescr.2020.047
[5] ↑ Mungoven, T. J., Henderson, L. A., Meylakh, N. 2021. Chronic migraine pathophysiology and treatment: a review of current perspectives. Front. Pain Res. 2:705276. doi: 10.3389/fpain.2021.705276
